Children are not just mini-adults
• Higher head to torso ratio: Head injury & Upper C-spine fractures
• Light weight – projectile when struck
• BSA to Wt. ratio – higher (rapid hypothermia)
• Large cardiopulmonary reserves – normal SBP in significant hypovolemia
Growth contribution by Proximal & Distal Physes
- Proximal humerus: 80%
- Distal humerus: 20%
- Proximal radius: 25%
- Distal radius: 75%
- Proximal ulna: 80%
- Distal ulna: 20%
- Proximal femur: 30%
- Distal femur: 70%
- Proximal fibula: 60%
- Distal fibula: 40%
- Proximal tibia: 55%
- Distal tibia: 45%
Age of appearance and fusion of Secondary Ossification Centers
Organization of Physis
• Collagen in Proliferative & Hypertrophic zone:
- Content: Lower
- Orientation: Vertical
- Effect: ↑Strain of compressive loading
• Zone of Ranvier = At periphery of physis (peripheral physeal growth)
• Ring of Lacroix = Overlying zone of Ranvier (Connects metaphyseal periosteum & cartilaginous epiphysis)
Biomechanical stability of Physis
• Zone of provisional calcification
• Nonplanar topography: Long bone physes • Undulating
• Lappet formations
• Reinforce periphery of physis: • Perichondral groove of Ranvier • Perichondral ring of Lacroix
• Additional: Muscular, capsular, ligamentous attachments
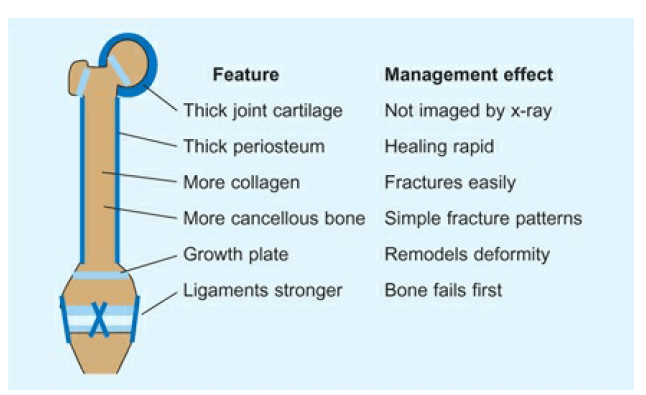
Fracture healing physiology
Rapid healing
• Increased bone vascularity
• Highly osteogenic periosteum
• Limited soft tissue disruption
Adequate healing & alignment maintenance of vast majority fractures = Cast immobilization
When fixation necessary – less rigid implants that are easily removed & don’t violate growth plate (smooth wires & flexible IMN)
Remodelling capacity
• 2 Mechanisms:
- Bone drift (some)
- Changes within physis (most)
• Factors affecting capacity to remodel: best for –
- Younger (>2 yr skeletal growth remaining)
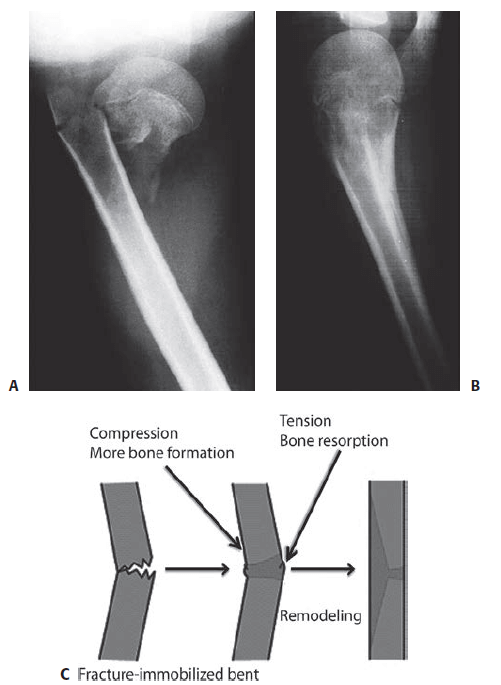
- Fracture site closer to physis & growth potential of physis
- Alignment of the angulation in normal plane of joint motion
• Spontaneous angulation correction unlinkely if –
- In other directions – Cubitus varus deformity
- Rotational deformities
- Plastic deformations
Growth stimulation
Symmetric growth stimulation:
• Loss of periosteal tension
• Increased blood flow to physes of fractured bone
• Most common after femur shaft fractures between age 2-10 years
Asymmetric growth stimulation:
• Asymmetrical hyperemia – overgrowth at fracture site
• Asymmetric periosteal tethering of physeal growth on C/L side • Incomplete proximal tibia metaphysis # Valgus overgrowth
Epidemiology
• Variable age across studies: 16-21 years; 25% of Pediatric injuries
• Physeal fractures: 14.5-27.6%
• Open fractures: 1.5-2.6%
• Multiple fractures: 1.7-9.7% • Recurrent fractures: ~1%
• Male to Female = 2.7:1
• Dominance: Left > Right upper limbs & Right > Left lower limbs
• OBESITY
• Distal radius > Supracondylar > Forearm shaft > Tibia shaft
Mechanism of Injury
• Occur at lower energy level than adult fractures
• Compression # – m/c at metaphyseal-diaphyseal junction (torus/buckle fracture) rarely cause physeal injury
• Torsional injuries –
- \Very young child with thick periosteum – diaphysis fails before physis (spiral fracture)
- Older child – physeal fracture
• Bending injuries –
- Young child – Greenstick fracture/Plastic deformation
- Older child – Transverse/Short oblique fractures
Incomplete fractures
A: Plastic deformation (Diaphyseal cortical bone)
- Disruption of junction between osteon units
- Reduction if >20 degrees or >4 years
B: Torus/Buckle fracture (Diaphysis-Metaphysis)
- M/c in Distal radius
- No extravasation of # hematoma minimal swelling
C: Green stick fracture
- Failure on tension side and plastic deformation on compression side
- Not enough residual force to complete the failure of entire osseous structure
Complete fractures
• Butterfly & Oblique fracture may be length unstable – CR & cast insufficient
• Fixation – sometimes necessary to maintain length
• Comminuted fractures – less common
• More readily dissipates energy before failure
• Porosity limits propagation of fracture lines
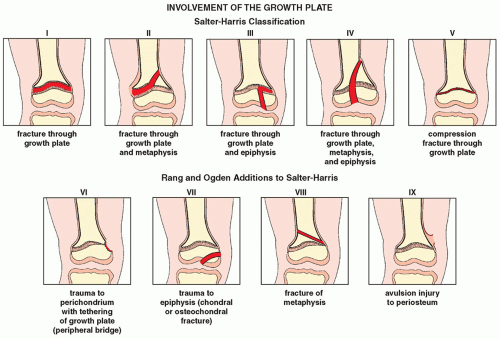
Physeal Injuries
Birth fractures
• Fracture within 1st week of life without any evidence of trauma
• Incidence: 0.1/1000 live births
• M/C = Humerus, clavicle, femoral shaft
• Risk factors: Difficult delivery, Large size, Breech presentation
• Warmth, swelling, pain, irritability with motion, pseudoparalysis
• R/O septic causes and brachial plexus injury
Non-accidental Trauma (NAT)/Child Abuse
• 12.1/1000 children
• Suspect if:
- Humerus diaphyseal fracture in <3 year
- Femur fracture in < 1 year old
- Metaphyseal corner fractures
- History (MOI) inconsistent with fracture pattern
- Multiple fractures in various stages of healing
- Skin stigmata suggestive of abuse
• Risk of reabuse: 50% and risk of death: 10%
Clinical Evaluation
Priorities
1. Pulmonary, Cardiovascular and Neurologic status
2. Musculoskeletal priorities:
- 1. C-spine injury
- 2. Joint dislocations
- 3. Unstable and open fractures
Evaluation
• Screening examination 1st
• Look at the whole child
• Look for obvious deformity and spontaneous movement
• Pseudoparalysis in child/infant – may be due to trauma
• Remove any splints or bandages to complete examination
• Deformity and swelling
• Point of maximum tenderness (PMT) – most important step in diagnosing occult injuries
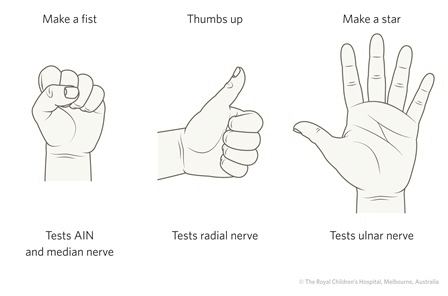
• Vascular status: NOT just pulse (CRT + Reaction while extending fingers/toes)
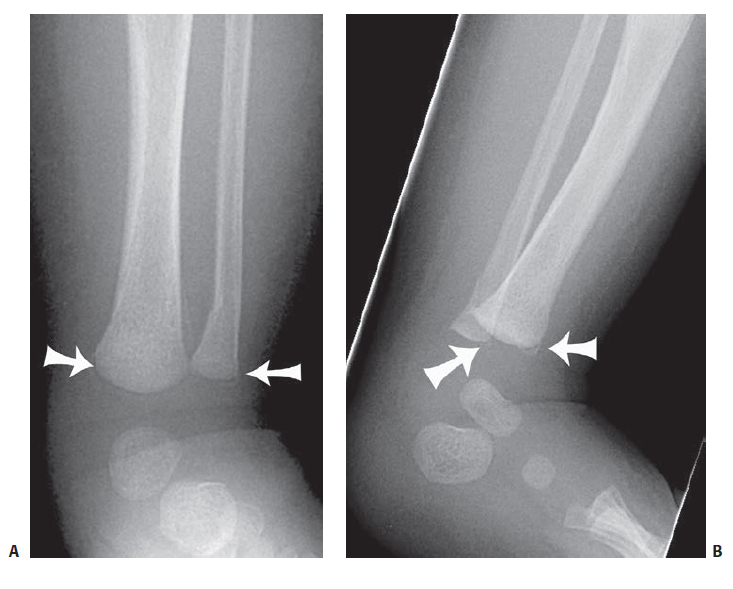
Imaging
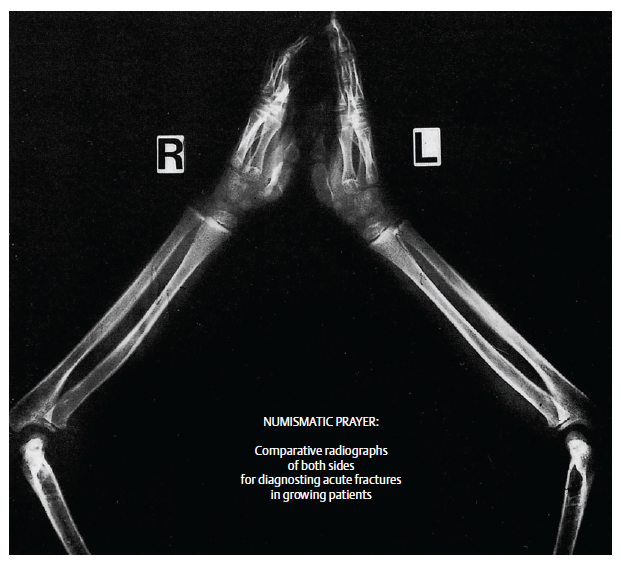
• Performed after pain management
• Knowledge of ossification centers – Normal variants vs Abnormal lesions
• Fracture lesions are larger than they appear (unossified cartilage)
• When in doubt:
- C/L radiograph can be ordered
- Oblique views can be ordered
• Skeletal survey for suspected child abuse or multiple trauma
• “Soft signs” eg. posterior fat pad sign in elbow – to be closely evaluated
• “Treat first, diagnose later” – readily possible in case of initially undetectable or minimally displaced and easily overlooked diaphyseal & metaphyseal fractures
• Exceptions – “Litigation injuries”
1. Non-displaced lateral condyle fracture of humerus 2. Dislocation of radial head (Isolated or Monteggia)
3. Rotational deformity in supracondylar fracture of humerus 4. Proximal greenstick fractures of tibia
5. Fracture of medial malleolus
• Arthrography – may be useful in assessing cartilaginous injury
• MRI: Spinal injuries & Occult physeal/epiphyseal trauma
• CT: evaluating complicated intra-articular fractures
• Bone scans:
- Evaluation of fractures and Occult stress fractures
- Screening of entire skeleton in suspected child abuse
• USG: detecting non-displaced or minimally displaced fractures
• Examination under anesthesia: Should not be performed without intent of therapeutic intervention during the same setting
Treatment
Aims
1. Quick and effective relief of pain
2. Reconstruction of normal anatomy and function
3. Early mobilization and resumption of child’s activities
4. Avoidance of unnecessary and repeated reduction attempts
5. Avoidance of late complications
6. Treatment appropriate to child’s age & type of injury
7. Achieving optimal result with minimal invasion
General principles
1. Children heal faster
2. Growing bones remodel more easily
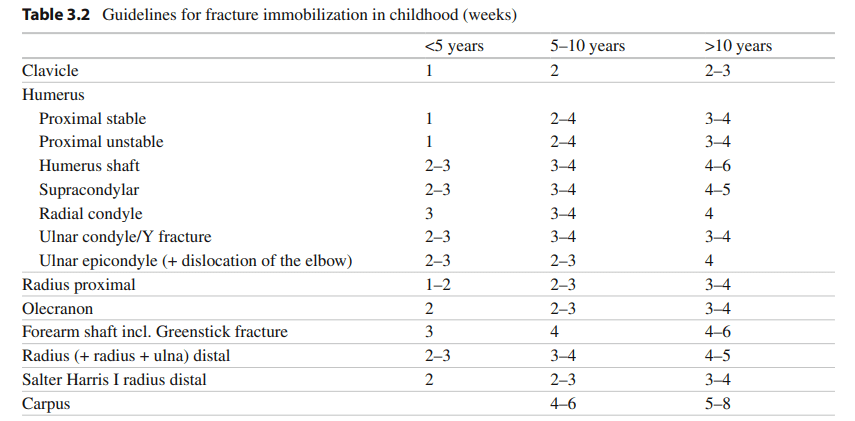
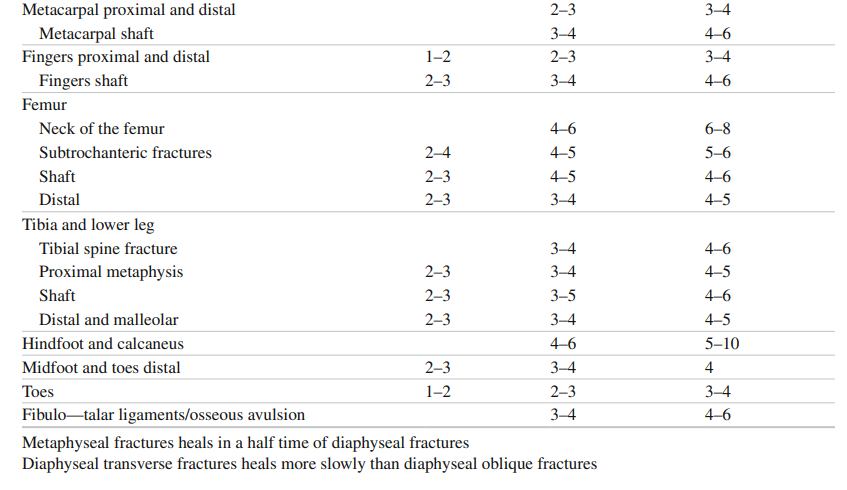
3. Need less immobilization time
4. Stiffness of adjacent joints less likely
5. When possible, restore: length, alignment and rotation
6. Maintain residual angulation as small as possible using closed treatment methods – molded casts, cast changes, cast wedging, etc.
7. Displaced intra-articular fractures will not remodel – anatomic reduction mandatory
Conservative management
WITHOUT ANESTHESIA (No reduction)
• All “non-displaced” epiphyseal, metaphyseal and diaphyseal fractures
• All diaphyseal & metaphyseal fractures with slight angulation of fragments (betn 10-30 degrees depending upon patient’s age) later treated with wedges
• All clavicular fractures in <12 years age
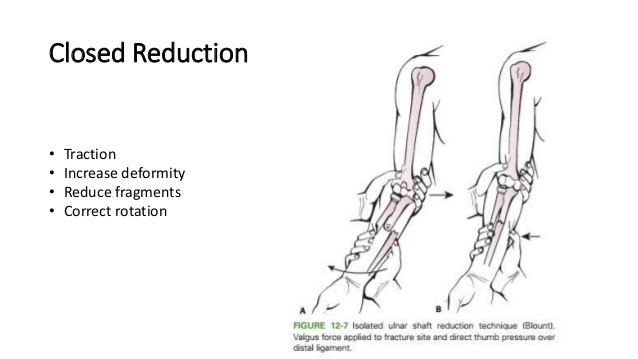
WITH ANESTHESIA (Closed reduction with some form of anesthesia)
• Common & notorious technique of “pressing” a fracture with & without pain medication should be avoided
• All completely displaced fractures that can be transformed into stable situation by reduction (esp. transverse fractures)
Birth injuries:
• Clavicle or humeral shaft fractures treatment = Pinning baby’s sleeve to front of shirt X 1-2 weeks until healed
• Femoral shaft fractures treatment = Splinting or Pavlik harness
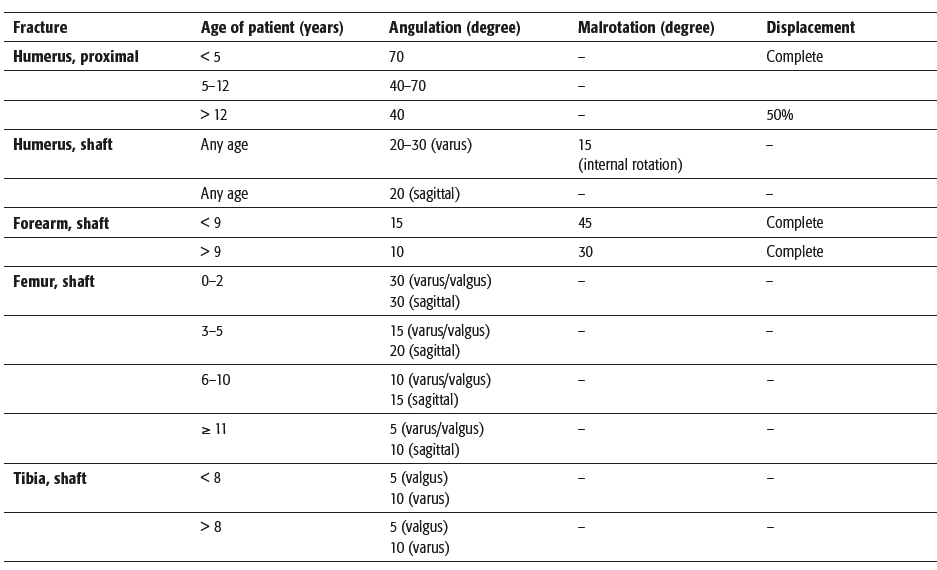
Acceptable malalignment after non-operative management
Closed Operative Management
Indications – Potential signs for instability like:
• Oblique fracture line
• Same level in paired bones
• Fully displaced fractures
Options:
1. K-wires
2. Cannulated screws 3. ESIN
4. External fixation
Open Reduction and Fixation
• Open fractures
• Polytrauma
• Head and spinal injuries
• Femoral neck fractures
• Lateral condyle fracture – humerus
• Displaced articular
• Salter Harris 3 and 4
• Nonunion or Delayed union
• Irreducible fractures if several attempts are not successful
Open fractures
• Classification – same as for adults
• Management Sequence – same as for adults
• Management principle different in children:
- Soft tissue healing is more rapid and complete
- Non-contaminated devitalized bone left in place will incorporate
- Periosteum will generate new bone when bone is lost
- Delayed union or nonunion is uncommon
- External fixators may be left in place for prolonged periods to be certain bony union is solid
Physeal injuries
Goal: Achieve and maintatin acceptable reduction without subjecting germinal layer of physis to any further damage
Type I & II: Accepting any displacement after 7-10 days and perform osteotomy later
Type III & IV (intra-articular): Must be reduced regardless of the time elapsed since injury
K-wires
• Closed or open reduced metaphyseal fractures
• Separated epiphysis in distal radius and femur, distal and proximal tibia
• When physis must be crossed – Smooth K-wires
• Smallest diameter possible
• K-wires inserted at low speed and as close as possible to anatomic center of physis
• Avoid repeated drilling
• Removed as soon as fracture is stable (3-4 weeks)
• Supplemented with cast or splint
Lag screw fixation
• Articular and peri-articular fractures
• For Physeal injuries
• Preferable – Self drilling self tapping cannulated screws
• Parallel to physis, either in metaphysis, epiphysis or both
• Should always be removed if growth potential remains
ESIN (Elastic Stable Intramedullary Nailing)
• All diaphyseal fractures in children between 3-4 yrs to puberty
• Maximum weight of child = 50-60 kg
• Not indicated for intra-articular fractures
• Can be used in:
- Femur: Sub-trochanteric, Diaphyseal, Distal metaphyseal
- Leg: Diaphyseal
- Humerus: Diaphyseal, subcapital, even supracondylar
- Radius and ulna: Shaft, Radial neck
Intramedullary nail
• Femur shaft fractures in children >13-14 years
• ESIN is not stable enough, especially with overweight
• Must not violate active growth plate
External fixation
• Comminuted fractures in older children (femur, tibia, forearm)
• Polytrauma
• Open fractures with skin/bone loss or burns
• Unstable fractures
• Tapping the pin rather than drilling recommended by some
• Removed asap after some initial fracture stability
• Joint bridging can be done
Plate fixation
• Reserved to exception and special cases
• LC-DCP or LCP using MIPO technique whenever possible • Comminuted fractures of diaphysis in older children
• Complex metaphyseal fractures
Traction
Skeletal traction – obsolete
• If used – growth plates must be protected
• When growth plates are still open – traction through tibial tubercle is not permissible
Skin traction:
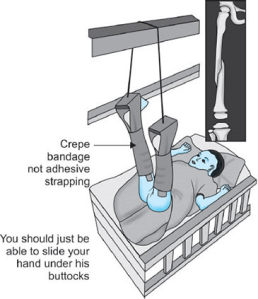
• Acceptable upto 3 years
• Used as overhead skin traction
• More used for lower extremity (femur fracture)
Radiographic follow-up
To verify correct position
• On 4th day (X-ray out of plaster): Only in cases of undisplaced lateral condyle fracture of humerus (to check displacement)
• Best time: 8th day (Soft tissue swelling has completely receded, Cast has been closed and Soft callus has partially formed)
- Ideal for application of cast wedges
• 2nd verification: On about 14th day
• Not necessary after this point: Negligible displacement risk, Secondary reduction not possible, Cast wedging unsuccessful
To Verify Consolidation
• Between 4-5 wks after accident
• Not needed in:
- All clavicle fractures
- Non-displaced metaphyseal impacted fracture
- All metaphyseal phalangeal fractures
Growth arrest line (Appear 6-12 wks after fracture)
Parallel to physis – physiological
Converge towards physis – suspect physeal bar
To evaluate growth
Performed at long intervals
If growth disturbance due to partial physeal closure: MRI>CT
Followup examinations
• 1st day: Cast and periphery should be examined
• 4th day after closure of cast: Cast, soft tissue and periphery
• At every radiographic follow-up
• When the fracture has consolidated
- Consolidation examinations – Onset of motion and onset of use
- Palpation of fixation callus is more important than callus in out of plaster radiograph
- If callus is still tender to palpation – limb immobilized for next 2-3 weeks until pain is absent
Functional examination
• Only after 2-3 weeks of removing cast
To evaluate growth
• Upto 2 years: Growth disturbance with clinical sequelae expected or any intra-articular fractures
• At long intervals: 1-2 years
Aftercare
• Mobilization without any rules and restrictions during 1st 3 weeks after cast removal
• Only restriction: Should not participate in school sports until 3 weeks after full use has been allowed
• No need of medication or physiotherapy
Complications unique to pediatric fractures
• Complete growth arrest
• Overgrowth
• Progressive angular or rotational deformities
• Osteonecrosis
• Malunion – not usually a problem (except Cubitus varus)
• Non-union – hardly seen (except Lateral condyle)
• Compartment syndrome – 3 “A”s
References
1. Rockwood and Wilkins’ Fractures in Children – 8th Edition (2014)
2. Pediatric Fractures and Dislocations – 1st Edition (2004), Lutz Von Laer
3. Fundamentals of Pediatric Orthopedics – 5th Edition, Lynn T. Staheli
4. Tachdjian’s Pediatric Orthopedics – 5th Edition (2014)
5. AO Principles of Fracture Fixation – 3rd Edition (2017)
6. Skeletal Injury in the Child – 3rd Edition, John A. Ogden
7. Campbell’s Operative Orthopedics – 13th Edition
8. Management of Musculoskeletal Injuries in the Trauma Patient – 2014