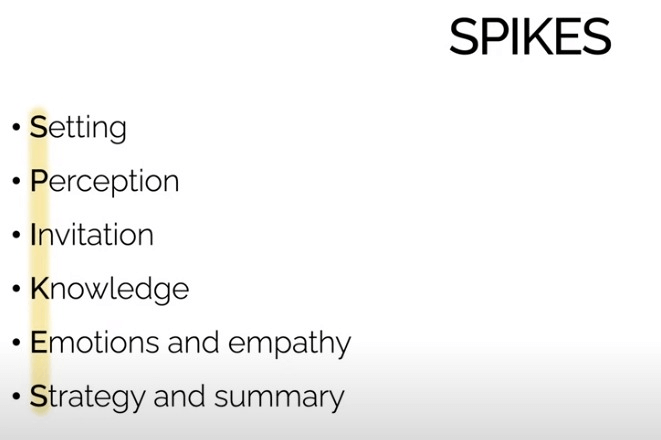
Setting
Mnemonic: IPC
- Introduce yourself
- Identify patient with 2 pieces of information like name and DOB
- Infection control measures (wash hands or sanitize hands)
- Involve significant others (establish whether the patient would like someone to be in the consultation with them)
- Privacy must be arranged
- Pager must be silenced
- Consent must be taken
Perception of condition/seriousness
- Take a brief history to identify important symptoms
- Elicit “ICE” history (Ideas, Concerns and Expectations)
- Accept denial but do not confront at this stage
Invitation from the patient to give information
- Ask patient if s/he wishes to know the details of the medical condition and/or treatment
- Accept patient’s right to not know
- Offer to answer questions later if s/he wishes
- To find out what your patient wants, simply ask questions like:
- Would it be helpful for you to know what to expect from here on out with your illness?
- Would it be OK if we talk about some serious issues with your care?
- We have these lab tests back. Can we talk about them?
Knowledge – giving medical facts
- Fire a warning shot, e.g. “I’m afraid the results are worrying”, “This may be serious than we originally hoped”.
- Keep the terms simple and direct, e.g. use “cancer” instead of “growth” or “malignancy”
- Break the news in small chunks
- Give any positive aspects first, e.g. “cancer has not spread to lymph nodes”, “treatment is available locally”, “it is highly responsive to therapy”, etc.
- Avoid giving false hopes, despite the need for confirmatory test
- Give facts accurately about treatment options, prognosis, costs, etc.
Explore Emotions and Empathize
- Identify emotions expressed, give them time to respond and allow them to express their emotions.
- Silence – avoid the temptation to fill it, give them a few moments to respond
- Cries – offer them tissue and allow them to express their emotions
- Use the mnemonic “NURSE“:
- Name: “It sounds like you are distressed”, “I wonder if you are feeling angry”
- Understand: “If I understand what you are saying, you are worried how your treatment will affect your work”, “People going through your situation often report experiencing….. is that how you feel?”
- Respect: “I’m impressed with how well you have handled this”
- Support: “I’ll be with you during the treatments”, “Please let me know what I can do to help you”
- Explore: “Can you tell me more about this?”
Strategy and Summary
- Strategy – Give a clear plan but avoid too much technical information
- Advise CT scan or biopsy if needed
- Mention about treatment options
- Ask whether they want to clarify something
- If the patient asks how long they have to live, never give a precise answer. Ask for specific reason why they would like to know.
- Arrange a follow-up appointment as appropriate. Offer agenda for the next meeting.
- Leave contact details, e.g. bleep number as appropriate
- Close consultation and thank the patient
SPIKES protocol in application
Practice:
https://www.oscesense.com/osce-practice-communication-breaking-bad-news-2
References:
- DrExam Part B MRCS OSCE Revision Guide Book 2
- SPIKES: A Strategy for Delivering Bad News (utah.edu)
- SPIKES_Protocol_for_Breaking_Bad_News.pdf (ubccpd.ca)

Awesome, thank you for sharing 🙏🏾🙏🏾🙏🏾🙏🏾