Case Summary
A 45-year male presented to emergency with complaints of pain and swelling over scrotum for 10 hours (at around 11:00 pm). Upon further inquiry he had undergone vasectomy (no scalpel) at a local health post camp at around 1 pm on the same day. He had no known co-morbidities and prior surgical history.
On examination:
- He was alert with GCS of 15/15.
- He had no evidence of pallor and his hydration status was normal
On local examination:
- Swelling was present over scrotum; bluish discoloration was observed.
- Tenderness was present and bilateral testis could not be palpated separately.
Rest of the systemic examination were unremarkable.
An ultrasound scan was ordered in the ER which revealed scrotal hematoma.
Then the patient was planned for scrotal exploration with all the necessary pre operative investigations.
In the operating theatre:
- Spinal anesthesia was given.
- Patient was positioned in supine position and painting and draping was done after foley catheterization.
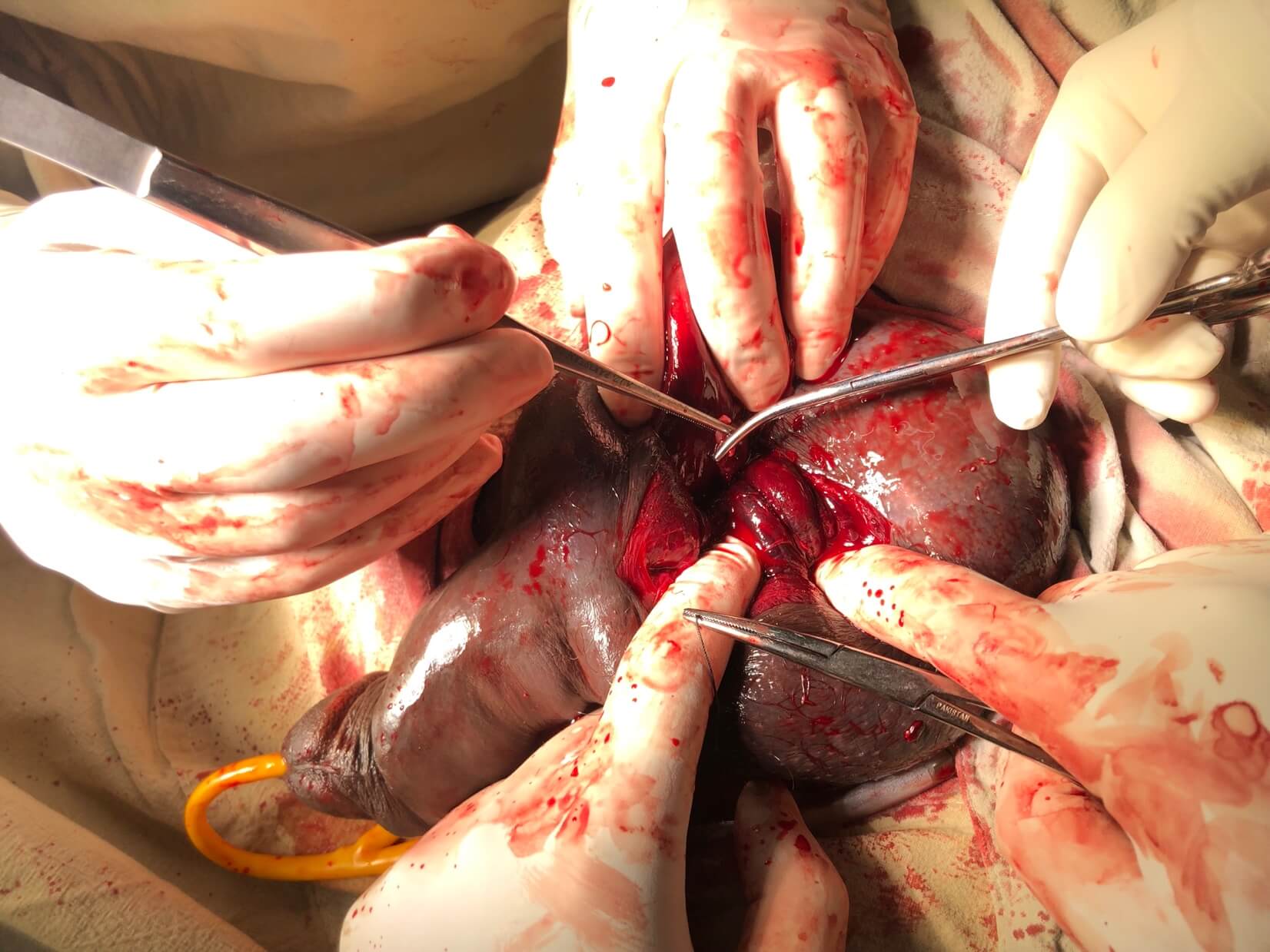
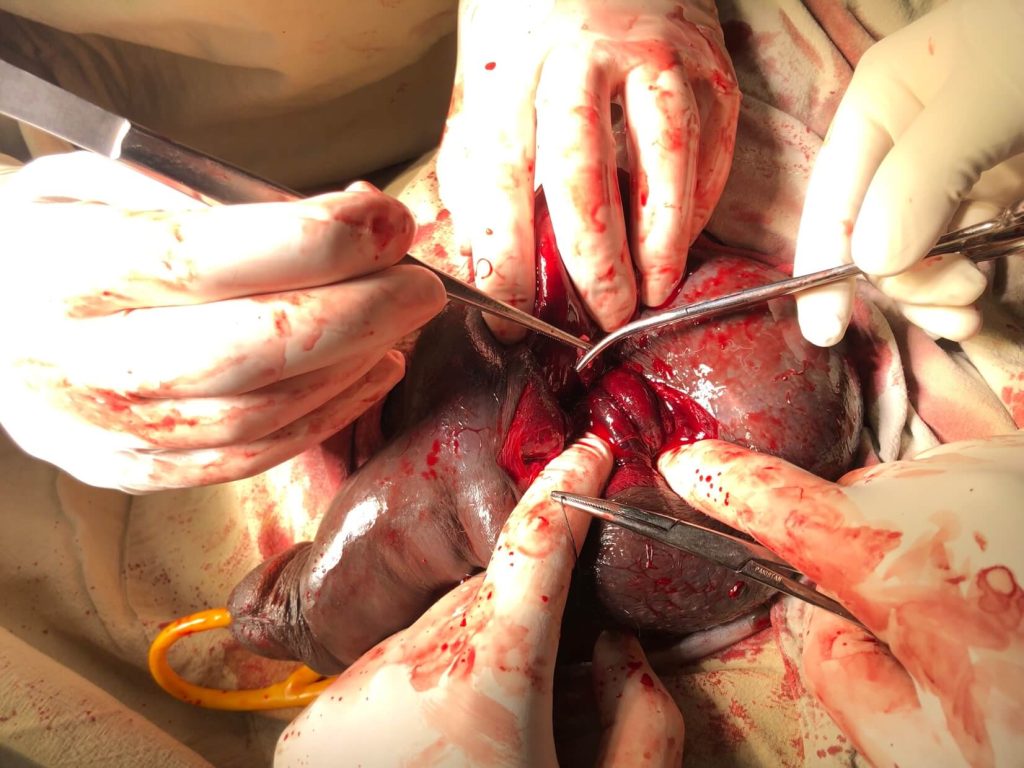
- Following findings were revealed on exploration. (pictures were obtained after taking consent from the patient)


Post operatively:
Patient was stable with no pain and fever. He recovered uneventfully and was discharged on day 2.
Discussion
Vasectomy is a highly effective and safe form of contraception. It was first described by Sir Ashley Cooper in UK. It is the most commonly performed urologic surgical procedure.
It is chosen as method of contraception by 11% of married couples, and 0.01% of men between ages of 25 and 49 undergo vasectomy annually (Barone et al, 2006).
The most preferred and commonly used method to perform vasectomy is the “no scalpel” method. It can be done under local anesthesia in an outpatient setting as a day care surgery.
The overall rates of local complication after vasectomy are 1-2% which include hematoma, infection, Fournier gangrene, chronic scrotal pain and traumatic fistula/scrotal sinus (Awsare et al, 2005).
The most important predictor of postoperative complications is surgeon volume and experience (Kendrick et al, 1987). Hematoma is the most common complication following surgery which varies from 0.09% to 29% with mean incidence of 2% (Kendrick et al).
But the cause for hematoma due to arterial injury has been reported very less in the literature. The cited cause for these scrotal hematomas is due to faulty surgical techniques, surgeries not performed by high volume surgeon and surgeries performed outside the controlled settings as in this case. A national survey in the United States reported that the incidence rate of hematoma for physicians who performed vasectomies 1–10 times annually was 4.6%, whereas the rates for those who performed vasectomies 11–50 times and more than 50 times annually were 2.4% and 1.6%, respectively reflecting the importance of surgical volumes (Forste R et al, 1995).
In conclusion, it can be said that the complication of hematomas following vasectomy can be reduced or prevented when performed in hospital settings under controlled environment by a group of experienced surgeons

He is an avid reader, guitar player, melodious singer and old songs lover. He has a passion for making medical knowledge accessible and comprehensive.