Definition of Diabetic foot
According to the WHO and International Working Group on the Diabetic Foot (IWGDF), diabetic foot is defined as the foot of diabetic patients with ulceration, infection and/or destruction of the deep tissues, associated with neuropathy and/or peripheral artery disease in the lower extremity of a person with (a history of) diabetes mellitus.

Diabetic Foot Management
Mnemonic: AIM DOC
1. Arterial disease assessment
- If pulses are not palpable, ABI <0.5 is the threshold for healing without angioplasty or vascular bypass surgery.
- Look for classic signs and symptoms of arterial disease even if ABI is normal:
- Cool, hairless feet with shiny skin, and claudication
- Ulcers on heel, outside foot or between toes
2. Infection
- Predominant organisms: Gram positive cocci especially S. aureus
- In chronic wounds: Gram negative rods may be found
- In foot ischemia or gangrene: Anaerobes may be present
- Use appropriate antibiotics with appropriate route (NERDS and STONEES mnemonic may guide this)
- Silver dressings or honey may be beneficial as topical antimicrobial
3. Measure (Grade) the wound
- Ulcers that fail to reduce by half over the first 4 weeks of treatment are unlikely to achieve wound healing over a reasonable period
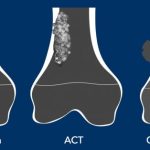
- Wagner classification/grading (higher the grade, lower likelihood to heal):
- 0 – No ulcer (may have deformity or cellulitis)
- 1 – Superficial ulcer (partial or full thickness)
- 2 – Deep ulcer (ligament, tendon, joint capsule or deep fascia without abscess, osteomyelitis or joint sepsis)
- 3 – Deep ulcer with abscess, osteomyelitis or joint sepsis
- 4 – Gangrene localized to forefeet or heel
- 5 – Extensive gangrenous involvement of entire foot
- Other various classification and grading systems: PEDIS, DEPA, University of Texas system, S(AD)SAD, etc. (https://onlinelibrary.wiley.com/doi/full/10.1002/dmrr.3272)
4. Debride
- Using surgical blade or diathermy
- Layer by layer starting with skin, subcutaneous tissue, deep fascia and muscle (cut until health bleeding obtained)
- Secure hemostasis
- Flush the wound with hydrogen peroxide (thermocoagulative)
- Flush the wound with normal saline
- 4 corner biopsy is obtained and sent for culture and sensitivity
- Paraffin or calcium alginate dressing (hemostatic) or a Negative Pressure Wound Therapy (NPWT) if hemostasis is well secured
Sharp debridement should be avoided if the limb has poor circulation or the wound is covered by eschar (provides protective barrier) without signs of infection.
5. Off-load the wound
This is vital for treating neuropathic ulcers. Total contact casting (TCC) works because it diminishes pressure on the wound, increases the surface area on the plantar aspect of the foot and limits all muscle-tendon activity. abnormal stresses, usually from bony prominences. TCC needs to be changed weekly and hence is costly and patients are often non-compliant.
Method of total contact casting – http://www.podiatryinstitute.com/pdfs/Update_2003/2003_51.pdf
Removable cast walkers (RCW) may be used but are less effective than TCC.
6. Cover with moist dressing
- Evidence to recommend any particular variety of moist dressing is insufficient
Adjunctive therapies
- Hyperbaric oxygen therapy (HBOT)
- Maggots (Lucilia sericata larvae)
Based on the article: https://cdn.mdedge.com/files/s3fs-public/Document/September-2017/5812JFP_Article4.pdf
Do not forget to go through Diabetes Made Easy Series: