Chronic wounds are wounds that have failed to proceed through an orderly and timely reparative process to produce anatomic and functional integrity over a period of 3 months.
Factors that Adversely Affect Wound Healing
Mnemonic: DIDN’T HEAL
- Diabetes (Diminished sensation, peripheral perfusion and impaired polymorphonuclear phagocytosis)
- Infection
- Drugs (Steroids and antimetabolites)
- Nutritional problems (Protein calorie malnutrition, deficiencies of Vitamin A, C and Zn)
- Tissue necrosis
- Hypoxia
- Excessive tension on wound edges
- Another wound (Competition between several healing areas for the substrates required for wound healing)
- Low temperature (Slower healing at distal part of extremities)
Diagnosis of Increased Bacterial Burden in Chronic Wounds
Signs suggestive of Superficial Infection (Can be treated topically):
Mnemonic: NERDS
- Non-healing
- Exudated
- Red friable tissue
- Debris (discoloration)
- Smell
Finding 3 clinical signs increased the specificity to 80.5% and sensitivity to 73.3%.
Signs suggestive of need for systemic antibiotics:
Mnemonic: STONEES
- Size increasing
- Temperature elevation
- Os (probes to bone)
- New breakdown
- Edema/Erythema
- Exudate
- Smell
Finding 3 clinical signs increased the specificity to 69.4% and sensitivity to 90%.
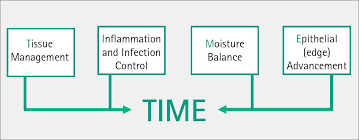
Wound Bed Preparation
Wound bed preparation is the management of a wound in order to accelerate endogenous healing or to facilitate the effectiveness of other therapeutic measures.
Mnemonic: TIMES
a. Tissue management
- Non-viable, necrotic, slough, eschar: Determine best type of debridement
- Viable: Choose optimum dressing and address dead space
b. Infection and inflammation control
- Presence of bacteria in a chronic wound does not necessarily indicate that infection has occurred or that it will lead to impaired wound healing (low level of certain bacteria can even facilitate wound healing by producing hyaluronidase)
- Diagnosis of infection is primarily a clinical diagnosis (use NERDS and STONEES)
- Treatment of infection:
- Healthy eating
- Encourage smoking cessation
- Address comorbidities like diabetes
- Local methods: Debridement, Cleansing, Topical antibiotics (iodine and silver preparations)
- Systemic antibiotics: Indicated when –
- Deep infection (systemic signs of infection, such as fever, and cellulitus extending at least 1cm beyond the wound margin and underlying deep structures)
- Where infection cannot be managed with local therapy
Sterilized honey can be used in chronic wounds. The antibacterial property can be attributed to following mechanisms:
- It creates hyperosmotic wound environment
- It produces hydrogen peroxide on dilution with wound fluid
Honey has been found to be a superior wound dressing agent compared to EUSOL (Edinburgh University Solution) in infected wounds. EUSOL is made with 1.25 gm boric acid, 1.25 gm bleaching powder and sterile water upto 100 ml. It has acidic pH and is useful in wounds infected with pseudomonas. It released nascent chlorine and becomes useless after 24 hours.
c. Moisture balance
- Moisture in wound enhances the natural autolytic process and also acts as a transport medium for essential growth factors during epithelialisation.
- Too dry wound bed: Scab formation leading to delayed healing and wound contraction; dessicated collagen matrix and surrounding tissues
- Excessive exudate: Wound bed becomes saturated and moisture leaks out onto peri-wound skin causing maceration and excoriation
- Choose dressing type according to volume and viscosity of exudate
- VAC therapy or total negative pressure can be used
- Compression bandages can be used in venous leg ulcers and lymphedema
d. Epithelial edge advancement
- Address T, I and M first
- Corrective therapies: Debridement, Grafts, Biologic agents
e. Skin around wound
- Protect peri-wound skin from infection, mechanical damage, maceration and dessication
Principles of Palliative Wound Care
Mnemonic: SPECIAL
- Stabilize the wound
- Prevent new wounds
- Eliminate Odor
- Control pain
- Infection prevention
- Absorb exudates
- Less Dressing Changes
Odor management in Chronic wounds
Most significant odor causing anaerobes include Bacteroides fragilis, Bacteroides prevotella, fusobacterium nucleatum, Clostridium perfringens, and anaerobic cocci. Other pathogenic organisms belong to the aerobic group of bacteria, the most common being Proteus, Pseudomonas, and Klebsiella.
The deodorizing effect of topical and oral administration of metronidazole has been shown to correlate with eradication of anaerobic infection, and its use on malodorous wounds has been well-documented.
For wound odor caused by aerobic bacteria, triple antibiotic ointment (polymyxin B, bacitracin zinc, and neomycin) is effective if used frequently and abundantly.
References:
- Sabiston Textbook of Surgery By Courtney M. Townsend, R. Daniel Beauchamp, B. Mark Evers, Kenneth L. Mattox
- https://www.woundscanada.ca/docman/public/wound-care-canada-magazine/2008-vol-6-no-2/323-wcc-2008-v6n2-free-papers/file
- https://www.woundsinternational.com/uploads/resources/content_9029.pdf
- Alvarez, O. M., Kalinski, C., Nusbaum, J., Hernandez, L., Pappous, E., Kyriannis, C., … Comfort, C. P. (2007). Incorporating Wound Healing Strategies to Improve Palliation (Symptom Management) in Patients with Chronic Wounds. Journal of Palliative Medicine, 10(5), 1161–1189. doi:10.1089/jpm.2007.9909

He is the section editor of Orthopedics in Epomedicine. He searches for and share simpler ways to make complicated medical topics simple. He also loves writing poetry, listening and playing music.