Everyone must be aware of the normal visual pathway and their defects. Here, I’ve tried to enlist the topics related to the visual pathway that are “nice to know” but you may have missed it or failed to understand properly. Below is the basic visual pathway:
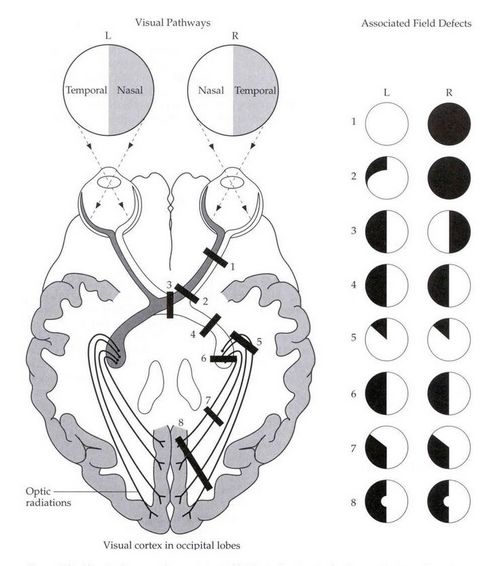
Loss of field of vision in both eyes: Homonymous or Heteronymous
Homonymous: Bilaterally involving same side of vision (right or left) i.e. nasal of one side and temporal of other
Heteronymous: Involving different side of vision (right and left) i.e. bilaterally nasal or temporal
Lesions from optic tract to visual cortex cause contralateral homonymous hemianopia (i.e. defect of vision in right when left pathway is impaired and vice-versa).
Central lesion of chiasma: Bitemporal heteronymous hemianopia
Lateral lesion of chiasma (bilateral): Binasal heteronymous hemianopia
Wilbrand’s knee
Anterior Wilbrand’s Knee
After the nasal retinal fibers cross in the optic chiasma, and before projecting down the optic tract:
- Inferior nasal hemiretinal fibers loop into the proximal contralateral optic nerve – anterior Wilbrand’s knee.
- The inferior nasal hemiretinal field corresponds to superior temporal visual field.
Posterior Wilbrand’s Knee
Before crossing in the optic chiasma:
- Superior nasal fibers form a redundant loop in the ipsilateral optic tract – posterior Wilbrand’s knee.
Anterior Junction or Anterior Chiasmal Syndrome
Lesion of optic nerve just anterior to the optic chiasma –
- Ipsilateral optic nerve involvement
- Anterior Wilbrand’s knee (Contralateral inferior nasal retinal fiber) involvement
Posterior Junction or Posterior Chiasmal Syndrome
Lesions of optic tract just posterior to the optic chiasma –
Remember: Macular fibers that cross do so in the central and posterior portions of chiasma.
- Ipsilateral temporal retinal fibers involvement
- Contralateral nasal retinal fibers involvement
- Posterior Wilbrand’s knee (Ipsilateral superior nasal retinal fibers) involvement
They produce centrally placed bitemporal scotomas.
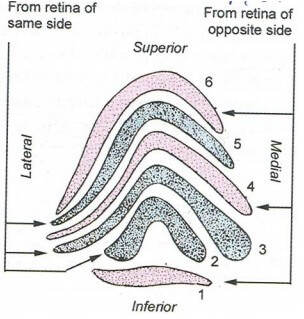
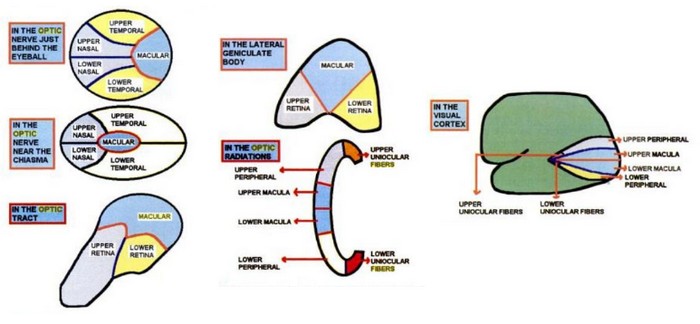
6 Laminae of Lateral Geniculate Body (LGB)
Grey matter is split into 6 parts by the white matter.
- Axons from the ipsilateral eye end in laminae 2, 3 and 5.
- Axons from the contralateral eye end in laminae 1, 4 and 6.
They divide into parvocellular and magnocellular subtypes.
- Parvocellular subtypes – projections from small ganglion cells sensitive to color and shape
- Magnocellular subtypes – projections from larger ganglion cells sensitive to motion
2 Eponymous Optic Radiations
Optic radiations extend from Lateral Geniculate Body (LGB) to Visual cortex.
- Meyer’s loop (Inferior retinal fibers) – pass through temporal lobe looping around inferior horn of lateral ventricle to the lingual gyrus (occipital lobe below calcarine sulcus).
- Baum’s loop (Superior retinal fibers) – pass through the parietal lobe to the cuneus (occipital lobe above calcarine sulcus).
Lesions:
- Temporal lobe: Inferior retinal fibers involved (Superior qudrantic hemianopia – pie on sky contralateral to lesion)
- Parietal lobe: Superior retinal fibers involved (Inferior quadrantic hemianopia – pie on floor contralateral to lesion)
Optic radiation pass through Internal Capsule
These fiber pass through retrolentiform part of internal capsule.
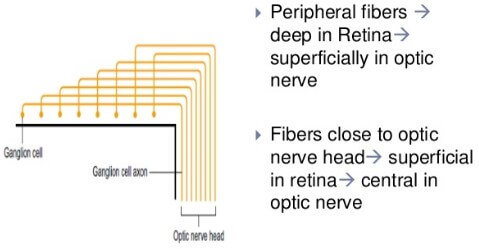
Orientation of Retinal Fibers
| Optic tract | Lateral Geniculate Body | Optic Radiation | Cerebral cortex | |
| Macular fibers | Dorsolaterally | Posterior 2/3rd | Center | Posterior |
| Upper retinal fibers | Medially | Medial Anterior 1/3rd | Upper part | Anteriorly – above calcarine sulcus |
| Lower retinal fibers | Laterally | Lateral Anterior 1/3rd | Lower part | Anteriorly – below calcarine sulcus |
Macular sparing in Posterior Cerebral artery Occlusion:
- Due to bilateral projection to occiput and collateral blood supply from Middle Cerebal Artery (MCA)
- Posterior tip of occipital cortex unaffected
Macular involvement if tip of Occipital cortex involved:
- In head injury or gunshot injury
Wernicke’s Hemianopic Pupil
Everyone probably knows this defect. It is the defect seen in optic tract lesion which receives crossed nasal fibers and uncrossed temporal fibers:
- Ipsilateral temporal retinal fibers involvement: Ipsilateral nasal visual field defect
- Contralateral nasal retinal fibers involvement: Contralateral temporal visual field defect
This is called contralateral homonymous hemianopia and also Wernicke’s Hemianopic pupil.
Optic atrophy
- Present in lesions of Lateral Geniculate Body (LGB) and pathway anterior to it – Descending optic atrophy.
- Absent in lesions posterior to LGB (i.e. optic radiations and cortex).
- This is because 2nd order neurons synapse in LGB.
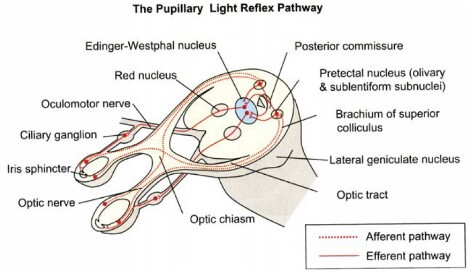
Pupillary reflexes
Defect in lesions anterior to LGB.
Normal in lesions of LGB and pathway posterior to it (i.e. optic radiations and cortex).
Afferent pupillary defect
Lesions upto pre-tectal nucleus –
- Absolute:
- No light perception in eye
- No direct reflex in ipsilateral eye and no consensual reflex in opposite eye
- Normal direct in opposite eye and normal consensual in involved eye
- Pupils are equal
- Normal near reflex (Like light reflex, near reflex is also consensual and hence, normal)
- Relative (RAPD): Marcus-gunn pupil in Swinging flash light test
- Pupils constrict to brighter light and dilate to dimmer light
- The affected eye instead of being completely blind, perceives as if the light is dimmer
- Hence, pupils appear to be dilated when light is shown on affected eye relative to the normal eye.
Near reflex: Comprises of –
- Convergence reflex: Convergence of visual axis and associated pupillary constriction (mediated by fibers projecting from medial rectus via mesencephalic nucleus of CN V to the E-W nucleus)
- Accomodation reflex: E-W nucleus activation leads to pupillary constriction and contraction of ciliary muscles makes lens more spherical and powerful.
Unlike in the light reflex, projections are from the supranuclear level (corticonuclear fibers from frontal eyefield) in near reflex.
- Efferent pupillary defect: Lesions behind pre-tectal nucleus i.e. from E-W nucleus to short ciliary nerves to both constrictors of the eyes
- Ipsilateral absence of direct and consensual light reflex
- Ipsilateral absence of near reflex (E-W nucleus and tracts further are also the part of accomodation reflex).
- Ipsilateral fixed and dilated pupil leading to Anisocoria (Affected eye is unresponsive and apparently perceiving dimmer environment with impaired consensual light reflex from the opposite eye as well).
The 2nd order neurons (Ganglion cells) do not synapse in LGB in the pathway of light reflex. It passes between the LGB and MGB to end in ipsilateral pretectal nucleus. The internuncial fibers project to bilateral Edinger-Westphal nucleus from the pretectal nucleus which forms the basis of consensual light reflex.
Near-Light Dissociation
This is a condition when light reflex is absent and near reflex is present.
- Light reflex: retina → optic nerve → optic chiasm → optic tract → pretectal area → bilateral E-W nucleus
- Near reflex: frontal eye field → corticonuclear fibers → bilateral E-W nucleus
For near-light dissociation to be present:
- Consensual near reflex must be intact
- Consensual light reflex must be impaired
The consensual light reflex is mediated by the internuncial fibers from pretectal nucleus to bilateral E-W nucleus. Hence, afferent lesions around this region gives rise to near-light dissociation because the afferent fibers of near-reflex that enter E-W nucleus more rostrally in midbrain and are spared.
Causes of near-light dissociation:
- Lesion in dorsal midbrain:
- Damage to pre-tectal nuclei (demyelination): Argyll-Robertson pupils (Syphilis, Diabetes)
- Damage to posterior commisure (compression by pineal tumor): Parinaud syndrome (Dorsal midbrain syndrome)
- Bilateral total afferent defect:
- Convergence reflex pathway is unaffected as it starts from the medial recti, leading to near-light dissociation.
- Adie’s tonic pupil:
- Injury to ciliary ganglion and or post-ganglionic fibers resulting in abnormal regrowth of short ciliary nerves.
- Near-reflex is not spared but restored later and hence, also called pseudo-near light dissociation.
- In short ciliary nerves – Accommodative fibers : Sphincter fibers = 30:1
- Hence, with random regeneration of fibers, power of accommodation is likely to recover, whereas the light reaction will not.
- Like a single eye Argyll-Robertson pupil.
Kernohan’s Notch
In transtentorial (uncal) herniation, due to mass effect there is compression of the contralateral crus cerebri of midbrain against the free edge of tentorium cerebelli. This is known as Kernohan’s notch. This may also put pressure on the ipsilateral CN III and posterior cerebral artery. The neurologic defects in this setting are:
- Contralateral corticospinal tract involvement in crus cerebri: Ipsilateral hemiparesis (False localizing sign, i.e. UMN sign is expected on side contralateral to the lesion but seen in the ipsilateral side).
- Ipsilateral occulomotor nerve involvement: Ipsilateral fixed-dilated pupil, ptosis, “down and out” eye
- Ipsilateral posterior cerebral artery involvement (visual cortex): Contralateral homonymous hemianopia
Left sided lesion → Kernohan’s notch on right → Right corticospinal lesion → Left hemiparesis
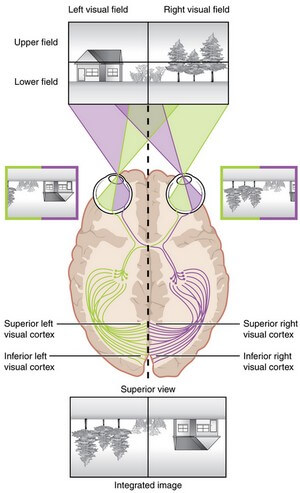
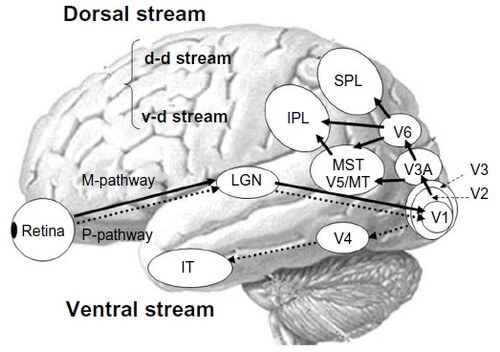
Central Visual Processing
The visual field projects onto the retina through the lenses and falls on the retinae as an inverted, reversed image. The topography of this image is maintained as the visual information travels through the visual pathway to the cortex.
- Area V1 (aka striate cortex) is the primary cortical processing area for macular retinal images.
- Areas V2 and V3 (aka extrastriate cortex) are the primary cortical processing areas for peripheral retinal images.
- Areas V4/V8 (aka occipito-temporal region corresponding to lingual and fusiform gyri) is the center for color processing.
- Lesion leads to achromatopsia (defect in color perception).
- Area V5 (aka temporo-parietal-occipital junction) is the motion detection area.
- Lesion leads to akinetopsia (disorder of motion perception).
- Midway along Medial-lateral plane of inferior occipital-temporal surface: Visual object recognition
- Lesion leads to visual object agnosia (loss of object recognition).
- Lateral inferior occipito-temporal fusiform gyrus: Familiar face recognition
- Lesion leads to prosopagnosia (deficit for recognition of familiar faces, such as those of family, friends, and colleagues).
- Medial inferior occipito-temporal parahippocampal gyrus: Place recognition
- Lesion leads to difficulty in recognition of familiar environment.
- Caudal portion of the intraparietal sulcus: Stereoscopic processing
- Remaining portion of intraparietal sulcus: Reach area
- It tells the motor cortex where to move to produce a desired effect.
- Lesion leads to optic ataxia (impairment of reaching for objects in the environment) and oculomotor apraxia (impairment of voluntary eye movements to command).
- Superior and inferior parietal lobule: Body spatial awareness
- Lesion results in hemineglect.
Anton Syndrome:
- Bilateral lesions in V1 have bilateral blindness but are unaware of their deficit (anosognosia).
- When asked directed questions about their environment, patients with Anton syndrome confabulate confidently.
- Suggests right frontoparietal disorder.
Bálint syndrome:
- Simultagnosia (only able to visualize one object at a time) along with optic apraxia and optic ataxia
- Suggests widespread bilateral occipito-parietal lesions





EXCELLENT INFORMATION , PASS ON TO MY STUDENT; ESPECIALLY THOSE WITH PROBLEMS