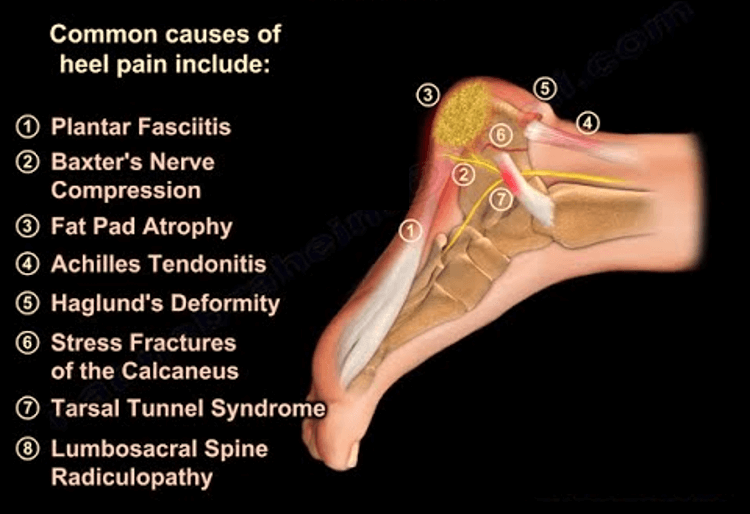
Mnemonic: HEEL PAINS
1. Heel pad syndrome
2. Enthesopathy
3. Entrapment
4. Ligaments
5. Plantar fasciitis
6. Posterior tibial tendinopathy/tenosynovitis
7. Peroneal tendinopathy/tenosynovitis
8. Arthritis
9. Impingement
10. Neuroma
11. Spurs
12. Stress fracture
13. Sinus tarsi syndrome
14. Sever’s disease
15. S1 radiculopathy
| Condition | Description | Site of heel pain | Symptoms | Signs | Management |
| Heel pad syndrome | Inflammation or atrophy of heel fat pad | Plantar | Walking after rest or barefoot painful, pain increases with activity; patient often overweight | Tender to palpation of heel pad; tiptoe standing/walking may cause pain relief | Rest, ice, taping, anti-inflammatory/analgesic medicines, heel cups, proper foot wear |
| Enthesopathy – Achilles | Achilles insertional tendinopathy | Posterior | Change to weight bearing load (foot wear or running); middle aged; worsens with activity; fluoroquinolone use | Tenderness +/- palpable prominence on both sides of achilles tendon insertion; passive dorsiflexion increases pain | Tier 1: Heel-lifts, open back shoes, cryotherapy/topical anlagesics, limit activities, oral anti-inflammatories, orthoses, physical therapy, weight loss Tier 2: + Immobilization (cast or CAM walker) Tier 3: Surgery (resection of insertional spurring; tendon debridement) |
| Entrapment | |||||
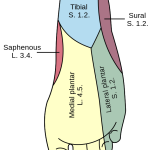
| a. Posterior tibial nerve (Tarsal tunnel syndrome) | Can be caused by trauma, space occupying lesions, poor biomechanics or systemic diseases | Medial | Neuropathic pain in posteromedial ankle/heel (sometimes into distal sole and toes); worsening with standing, walking, running; relieved with rest, elevation, loose footwear; pain radiating to medial aspect of leg (Valleix phenomenon) | Tinel sign positive; Provocative maneuver (dorsiflexion-eversion or plantar flexion-inversion); often hyperpronated or flat feet | Activity modification, corticosteroid injection, oral or topical NSAIDs, orthotic devices, neuromodulator drugs (TCAs, antiepileptics) |
| b. Baxter’s nerve entrapment (between abductor hallucis/AH and Quadratus plantae/QP) | Baxter nerve is the 1st branch of lateral plantar nerve (motor to Abductor digiti minimi; sensory to plantar heel) | Medial | Neuropathic pain; common in running atletes | Tenderness over the medial aspect of the heel in line with the posterior border of the medial malleolus; no sensory deficit | Like tarsal tunnel syndrome Surgical release of abductor hallucis fascia |
| c. Jogger’s foot (medial plantar nerve entrapment) | Compression at knot of henry (FDL and FHL); most common cause is foot orthotics; also in running athletes | Medial | Pain and numbness at the medial heel and arch radiating towards the first and second toe | Medial arch tenderness; Abductor Hallucis tenderness at navicular tuberosity; Tinel sign; Provocative (forced passive heel eversion) | Discontinue/modify orthotics Surgical release |
| Ligaments | Deltoid and spring ligaments | Medial | |||
| Lateral ligaments of ankle | Lateral | ||||
| Plantar fasciitis/fasciosis | Inflammation of the plantar fascia aponeurosis; baxter’s neuritis may co-exist | Plantar | Pain with first steps after prolonged rest (often morning) | Tenderness of medial calcaneal tuberosity (insertional) or along plantar fascia; Provocative (passive toe dorsiflexion – tightens windlass mechanism) | Tier 1 (trial of 6 weeks): Padding and strapping, stretching exercises, OTC arch support/heel cup, shoe recommendations, oral anti-inflammatories, corticosteroid injection Tier 2 (trial of 6 months): Corticosteroid injection, custom orthotics, night splint, immobilization, physiotherapy Tier 3: ESWT; Fascia release +/- Nerve release (nerve release cant be done endoscopically) |
| Posterior tibial tendinosis (PTT)/dysfunction (PTTD) | PTTD – increased laxity of posterior tibial tendon resulting in flat foot and heel varus; overuse and obesity; arthropathies | Medial | Pain at posterior edge of medial malleolus that may extend toward arch of foot | Swelling or redness over painful area; progressive loss of arch of foot; Unable to perform single limb heel raise | Early – weight loss, NSAIDs, icing, physical therapy, orthotics or bracing for arch and ankle support Trial of short leg cast for 6 weeks Surgery – tendon repair, tendon transfer, calcaneal osteotomy, tarsal bone fusion |
| Peroneal tendninopathy | Lateral | ||||
| Arthritis | Subtalar joint | Deep, vague | |||
| Impingement | Soft tissues or os trigonum | Posterior | Repetitive flexion activities; Pain in plantar flexed/en pointe position | Posterolateral ankle pain with passive ankle plantar flexion | NSAIDs, rest, immobilization, restricted weight bearing Surgical excision – open lateral approach or posterior ankle arthroscopy |
| Neuroma | Plantar | Neuropathic pain | Painful lump on palpation | Decrease pressure over affected area | |
| Spurs | Haglund deformity/runner’s bump/calcaneal exostosis/pump bump +/- retrocalcaneal bursitis | Posterior | Enlarged posterosuperior calcaneal prominence; aggravated by shoe wear; relieved by barefoot/open shoes | Tenderness lateral to the Achilles tendon, usually associated with a palpable posterior lateral prominence (but it is a radiographic diagnosis) | Tier 1: Open back shoes, cryotherapy/topical analgesics, orthoses, accommodative padding, oral anti-inflammatories, physiotherapy, weight loss Tier 2: + immobilization( cast or CAM walker) +/- injection of bursa Tier 3: Resection of Haglund’s/bursa; Calcaneal osteotomy |
| Plantar heel spur | Plantar | Associations – plantar fasciitis, arthritides (osteoarthritis, ankylosing spondylitis, psoriatic arthritis) | Decrease pressure to affected area | ||
| Stress fracture | Calcaneum | Plantar | Increased activity or change to harder walking surface; pain with activity progressively worsens to pain at rest | Tenderness with compression of calcaneus (but it is a radiographic diagnosis) | Activity modification with occasional non-weight bearing Heel pads or walking boots |
| Sever disease | Calcaneal apophysitis | Posterior | Adolescents; Worsens with activity or during growth spurt | Tenderness at achilles insertion; Pain with passive dorsiflexion and mediolateral calcaneal compression | Activity modification; NSAIDs; Ice; Stretching/strengthening exercise; Orthotics/shoe modification |
| Sinus tarsi syndrome | Sinus tarsi, or talocalcaneal sulcus, is an anatomic space bound by the calcaneus, talus, talocalcaneonavicular joint, and posterior facet of the subtalar joint | Lateral (anterior and inferior to lateral malleolus) | Pain in lateral calcaneus or ankle; feeling of foot/ankle instability; worse with exercise or uneven surface; history of repeated ankle sprains | Subtalar instability and increased ROM | Orthotics, Icing, Anti-inflammatory/Analgesics, Physiotherapy, Corticosteroid injections |