Absolute contraindications to Ascitic Tapping (Paracentesis)
While some authors have claimed ascitic paracentesis to be free from absolute contraindications, others have listed following as absolute contraindications:
- Clinically evident fibrinolysis
- Disseminated Intravascular Coagulation (DIC)1
- Clinically apparent oozing from needle sticks
- Acute abdomen requiring surgery2
Relative contraindications to Blind Paracentesis
Ultrasound guided paracentesis should be considered in following conditions:
- Pregnancy
- Severe bowel distension (risk of bowel perforation)
- Previous extensive abdominal/pelvic surgery (adhesions leading to risk of bowel perforation)
- Massive organomegaly
Precautions for Abdominal Paracentesis
- Stop anticoagulation – 3 days prior for warfarin and 1 day prior for subcutaneous heparin.
- Coagulopathy is no more regarded as a contraindication for ascitic tapping. However, some authors recommend considering Fresh Frozen Plasma (FFP) or Platelet concentrates for INR >2 and Platelet count <20,000 respectively despite scanty evidence, to support safety of patient.3
- Percuss the area of dullness.
- Make sure the spleen is not palpable.
- Catheterization of distended urinary bladder.
- Nasogastric decompression in case of bowel obstruction.
Needle entry sites to Avoid
- Avoid anatomical landmark for inferior epigastric artery which traces from a point just lateral to the pubic tubercle (which is 2 to 3 cm lateral to the symphysis pubis), cephalad (upward) within the rectus sheath.
- Avoid areas of skin infection.
- Avoid areas near surgical scars.
- Avoid visibly engorged veins (likely to be present in patients with liver disease).
Preferred Needle entry site
1. Selected site for needle entry must always be lateral to the rectus abdominis muscle to prevent puncturing inferior epigastric artery as described earlier.
2. Shifting dullness (percussing for resonance and moving laterally until dullness is percussed) is used to identify areas of fluid for paracentesis.
3. Lateral approach (Left lower quadrant vs Right lower quadrant): Left lower quadrant is preferred because 4 –
- Studies have found skin to be thinner in left lower quadrant
- Studies have found pooling of fluid to be deeper in left lower quadrant
- It avoids appendectomy scar and puncturing gas-dilated cecum especially in critically ill patients.
4. Selecting the lower quadrant site:
- 2-4 cm (2 finger breadths) cephalad and medial to anterior superior iliac spine (ASIS).
5. Infraumbilical midline approach: The site 2 cm below the umbilicus was used previously as it was along the linea alba which is devoid of vessles. However, this approach has been abandoned now as one laparoscopic study found that in patients with portal hypertension there are collaterals in the midline which can rupture during paracentesis.5 Also, the recanalized umbilical vein may be present caudad to the umbilicus in the midline, an area that should be avoided.
Choice of Needle
- Diagnostic paracentesis: 20 G needle (for thin patients) and 18-20 G needle (for obese patients).
- Therapeutic paracentesis: 16 G IV cannula is preferred (Central venous catheter can also be used)
Plastic cannula vs Metal catheter: The AASLD Practice Guideline recommends using large caliber, multi-hole cannulas for therapeutic paracentesis as plastic cannulas possess risk of kinking and breakage into the peritoneal cavity requiring unnecessary laparoscopy or laparotomy.
Preventing leakage of fluid from puncture site
Needle insertion techniques
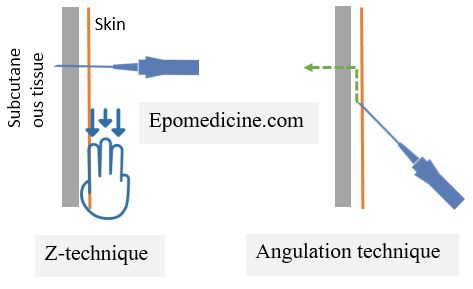
2 commonly used techniques to prevent leakage of peritoneal fluid from puncture site by sealing the needle tract when skin resumes normal shape:6
1. Angular insertion: Enter the skin in 45° angulation and advance the needle 1-2 cm under the skin, before piercing the subcutaneous tissue perpendicularly.
2. Z-track technique: Skin is pulled 2 cm downwards before insertion of the needle and is then let go only after ascitic fluid is seen to be flowing.
Pressure dressing
After collection of the sample, remove catheter or needle, and apply firm pressure to the site for 5 minutes.
Suturing
If leaking of ascitic fluid persists despite a pressure dressing, close the paracentesis tract with a mattress stitch.7
Qunatification of leak
When a leak occurs, placing an ostomy bag over the leak site allows quantitation of the amount of fluid that is leaking.
How do you know that the needle has entered peritoneal cavity?
When the needle enters the peritoneal cavity, following can be noticed:
- Dense connective tissue of the peritoneum will yield a noticeable “pop” when pierced.
- Loss of resistance
- Flash of ascitic fluid filling hub of needle or cannula
Volume Ascitic Paracentesis and Fluid Replacement
Diagnostic paracentesis
- Collection of 50 ml of ascitic fluid in a syringe is adequate.
Therapeutic paracentesis
Single Removal of <4-5 l ascitic fluid:
- Fluid replacement with crystalloid like NS is adequate.
Large volume paracentesis (≥5 l) or Total volume paracentesis (even >20 l):
- Supplementing 6-8 of albumin per each liter over 5 L of ascitic fluid removed is recommended to decrease possible complications of electrolyte and circulatory disturbances. 8
Indications of large volume paracentesis:
- Refractory ascites
- Tense ascites
- Respiratory distress
- Impending rupture of umbilical hernia
Cessation of drainage of Ascitic fluid
Possible causes:
- Abdomen is empty of ascitic fluid.
- Patient’s position is inhibiting drainage.
- The ascitic fluid has clotted in the drainage system.
- Plasstic cannula has kinked.
Prevention:
- Teach the patient to avoid exerting pressure on the drainage tubing.
- Keep drainage bag on a stand and lower than the puncture site to facilitate drainage by gravity.
Management:
- If the tapped volume is adequate, there is a probability that the abdomen is empty. In such cases, cannula should be removed and drainage must be discontinued.
- Change the patient’s position (gently move the patient onto their side to encourage flow by gravity) or gently press on the other side of abdomen.
- ‘Milk the tubing’ or change the drainage system if ascitic fluid has clotted.
Detecting and managing life threatening complications during abdominal paracentesis
1. Patient starts to cough:
- Keep “re-expansion pulmonary edema” in mind especially during Large Volume Paracentesis in Cirrhotics who are at risk of pre-morbidity with cardiovascular compromise like cirrhotic cardiomyopathy, hepatopulmonary syndrome and portopulmonary hypertension.9
- Management: Stop drainage by clamping IV set and manage pulmonary edema if present.
2. Hypotension and Shock:
- Usually seen in large volume paracentesis due to rapid mobilization of fluids from vascular space to third space, sudden release of intra-abdominal pressure and vasodilation.
- Prevention: Monitor blood pressure and consider volume replacement if large volume paracentesis is expected.
- Management:
- Clamp the drainage iv tube.
- Administer a bolus of IV fluid.
- Monitor vitals.
- If hypotension is persistent: consider starting a vasopressor infusion10
3. Circulatory disturbance and Bloody aspirate:
- Suspect intraperitoneal hemorrhage.
- Management:
- Correct coagulation abnormalities.
- Surgical consultation.
4. Peritonism and Initial fecal aspirate:
- Suspect bowel perforation and peritonitis.
- Management:
- Usually, small perforations are sealed off by omentum and abdominal pain gradually subsides.
- In case of persistent or worsening sign of peritonitis: Perform erect abdominal x-ray and look for gas under diaphragm; Surgical consultation.
5. Myocardial infarction:
- A rare complication of large volume paracentesis which is believed to occur due to activation of renin-angiotensin-aldosterone and sympathetic system leading to high systemic vascular resistance and blood pressure. 11
- Management of such patients may pose a great difficulty due to pre-morbid coagulopathy.