To make an appropriate diagnosis through a chest radiograph, it must be analyzed in a systematic manner. One of the common mistakes that students do is to miss the regions that needs to be looked for – commonest being the rib fractures. A mnemonic has been devised for this purpose: ABCDEFGHI
A) Assessment of Quality:
Mnemonic: PIER
1. Position:
- PA or AP radiograph: How to differentiate a PA and AP Chest X-ray?
- Pitfall: AP radiographs magnify the heart and mediastinum.
2. Inspiration:
- Is inspiration satisfactory?
- A good inspiration is indicated if the anterior end of the left 6th rib reaches or is projected above the level of the dome of the diaphragm.
- Pitfall: A small inspiration can cause-
- the heart to appear enlarged
- vessel crowding at the bases mimicking infection
3. Exposure:
- Is the exposure adequate?
- If the bony cage, ribs and vertebral bodies are just visible through the cardiac shadow, then exposure/penetration is adequate.
- If they are too clearly visible, then it is over-penetrated and if not visible, then it is under penetrated (under exposed).
- Pitfall: In over-penetrated X-rays you are likely to miss low density lesions.
4. Rotation:
- Is the patient rotated?
- The medial end of each clavicle should be equidistant from a vertical line drawn through the spinous processes of the T1–T5 vertebral bodies.
- Pitfalls:
- Rotation can distort the mediastinal and hilar appearances mimicking a mass
- One lung may appear blacker than the other
B) Bones and Soft tissues:
- Note the central vertebral column and the horizontal ribs.
- Look for scoliosis, relative crowding of ribs (collapse or fibrosis) or wide separation of ribs (pleural effusion,
pneumothorax), osteoporosis, fractures, metastatic lesions, cervical rib, bony erosion of the ribs. - Look for subcutaneous emphysema, edema or foreign bodies
- Pitfall: Nipple shadow (bilateral) may mimic intra-pulmonary nodule
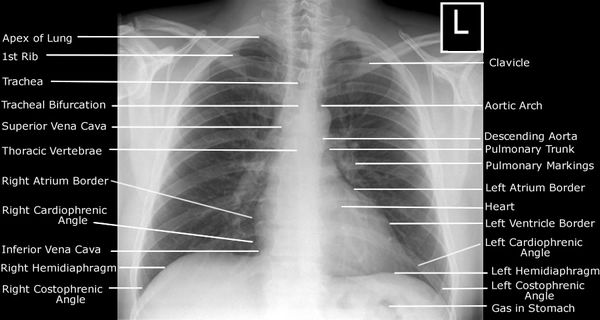
C) Cardiac Shadow:
- Is the heart enlarged? Are the heart borders clearly seen and well-defined?
- In an adult, the cardio-thoracic ratio (CTR) should be less than 50% on a PA radiograph. In young children the normal CTR can be slightly larger than 50% (~60%)
- An unclear heart border indicates a probability of pathology in the immediately adjacent lung.
- The right border is smooth, formed from above downwards by the superior vena cava, right atrium and inferior vena cava. The left border is formed from above downwards by aortic knuckle, pulmonary conus (artery), left atrial appendage, and left ventricle
- Pitfalls:
- A heart may have a CTR of less than 50% but it can still be enlarged — if its transverse diameter was very narrow to begin with. It may take some time before an enlarged heart reaches and exceeds a CTR of 50.
- A confluence of normal veins entering the left atrium outlined by air in the right lung appears as a density behind the right side of the heart – mistaken for an enlarged left atrium, or a mediastinal mass, or a paravertebral soft tissue swelling. This normal structure is not seen on the left side.
- If an apparent mass at the cardiac apex or adjacent to the right side of the heart: (a) is of low density; and (b) blurs the cardiac margin — then it is most likely to be a pad of fat.
D) Diaphragm:
- Are both domes of the diaphragm clearly seen and well-defined?
- If part of a dome is obscured — suspect pathology in the adjacent lower lobe.
- A flat diaphragm indicates hyperexpansion (COPD, emphysema, bronchiolitis) and a higher placed diaphragm indicates pleural effusion, collapse or diaphragmatic paralysis.
- Normally, right hemidiaphragm is placed slightly superiorly due to the liver.
- Air under diaphragm is normal on left side (gastric bubble)
E) Effusion:
- Are the costophrenic angles clear and well defined?
- Pleural effusion oscures these angles.
F) Fields and Fissures:
- For radiological purposes, the lung fields are divided into 3 zones.
- Upper zone: extends from the apex to a transverse line drawn through the lower borders of the anterior ends of the 2nd costal cartilages.
- Mid-zone: extends from this line to another line drawn through the lower borders of the 4th costal cartilage.
- Lower zone: extends from this second line to the bases of the lungs or to the dome of diaphragm.
- Each zone is examined on both sides and compared with each other for any abnormal finding (infiltrates, consolidation, mass, pneumothorax, etc.)
- Vessels should taper and become almost invisible towards the periphery of lung field.
- Look for thickening or fluids in major and minor fissures.
G) Great vessels:
- Is the aortic size and shape normal? Are the outlines of pulmonary vessels normal?
- Aortopulmonary window is a radiological mediastinal space between the aortic arch and left pulmonary artery seen on frontal chest x-rays. The AP window normally has a concave lateral border.
- A newly straightened or convex lateral border of AP window is considered abnormal and may be due to abnormality in it’s contents:
- mediastinal lymphadenopathy
- prominent mediastinal fat
- aortic or bronchial artery aneurysms
- malignancy – e.g. nerve sheath tumour (laryngeal nerves)
- More than 16 mm of the right descending pulmonary artery in the postero-anterior view suggests Pulmonary arterial hypertension (PAH).
H) Hila and mediastinum and Hidden areas:
- Are the hila normal – position, size and density?
- The left hilum should be at the same level or higher than the right – never lower than the right.
- The hilar density on each side should be similar.
- Look for mediastinal widening (aortic dissection), tracheal deviation and thymic shadow in children (not to be confused with a mass)
- Check the tricky hidden areas: lung apex, superimposed over the heart, around each hilum, below the diaphragm.
I) Impression:
- Does the impression correlate with the clinical finding of patient?
You can develop your own sequence of viewing X-rays but make sure that all the areas are covered so that the pathology is not missed. Generally, in examinations going from “out to in” or “in to out” is preferred.



Thank you very much, this was really very informative, I am now feeling confident in going in front of the class and reading a chest x-ray