Pediatric hydronephrosis is a broad term and encompasses various spectrum of disease. It can be broadly classified into:
- Antenatal hydronephrosis
- Post-natal hydronephrosis
Antenatal hydronephrosis (ANH)
It accounts for 1-3% of all pregnancies (Shamshirsaz et.al;2012) and the incidence will continue to rise due to increase use of prenatal ultrasound scan. USG is the mainstay of diagnosis due to advantage of no radiation hazards and cost effectiveness but has lot of interobserver variability.
Definitions:
Numerous grading systems have been devised to define ANH but there is no consensus on the best and reliable grading system. Currently 3 systems are utilized with their pros and cons.
1. APRPD (antero-posterior renal pelvis diameter) based:
| Degree | 2nd Trimester | 3rd Trimester |
| Mild | 4 to <7 mm | 4 to <9 mm |
| Moderate | 7 to ≤10 mm | 9 to ≤15 mm |
| Severe | >10 mm | >15 mm |
Advantage: easier to reproduce
Disadvantages:
- Fails to comment on calyceal dilatation and pelvic configuration
- Varies according to gestational age
- There are no formal studies on its reliability
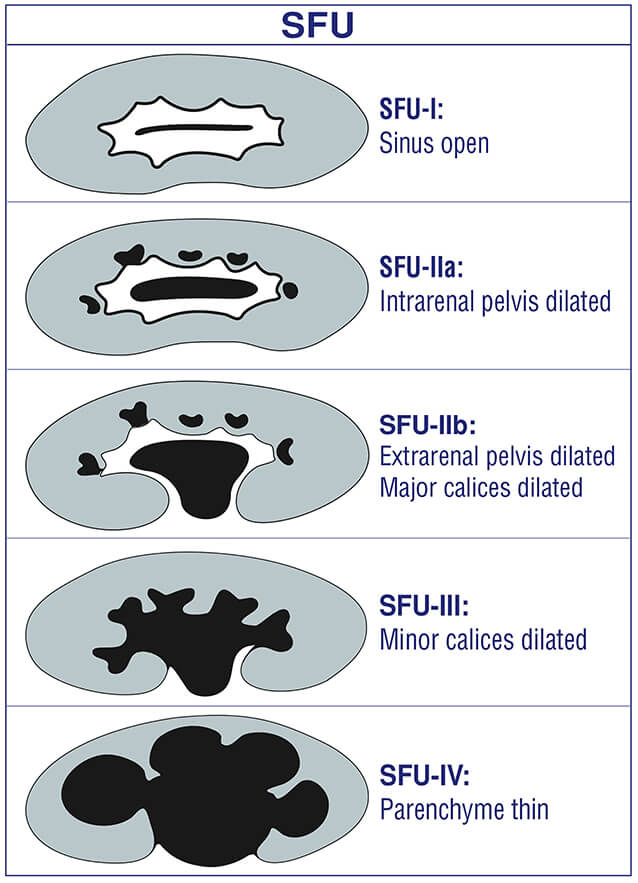
2. SFU system (society for fetal urology):
Broadly used by pediatric urologists and radiologists.
It has an added advantage of commenting on pelvic configuration and considers amount of calyceal dilatation
3. UTD classification (urinary tract dilatation):
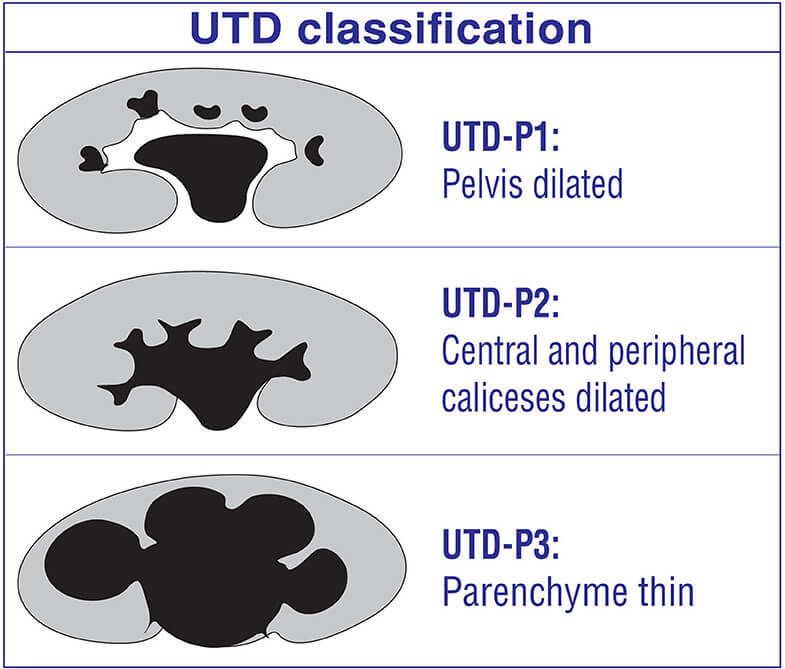
Advantages:
- Includes antenatal as well as post-natal grading
- Includes APRPD, calyceal and ureteral information
- Includes parenchymal, bladder abnormalities
- Comments on oligohydramnios
This system is widely used by pediatricians.
Causes of ANH:
| Etiology | Percentage |
| Transient hydronephrosis of fetal development | 41-88 |
| Ureteropelvic junction obstruction | 10-30 |
| Vesicoureteral reflux | 10-20 |
| Ureterovesical junction obstruction | 5-10 |
| Duplex collecting system | 5-7 |
| Posterior urethral valves | 4-6 |
Most common cause: transient hydronephrosis of fetal development (about 80%); self-limiting and does not require intervention.
Most common pathological cause: Ureteropelvic junction obstruction (UPJO)
Diagnostic findings:
Investigation of choice: USG (discussed earlier)
Abnormal findings:
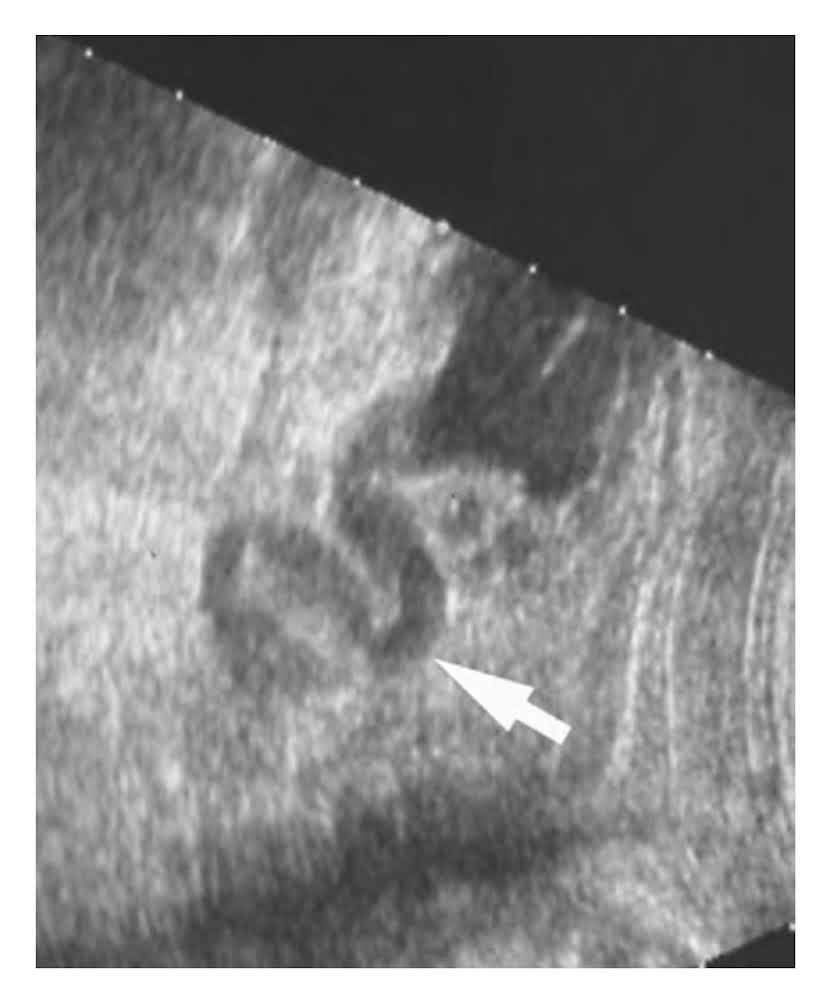
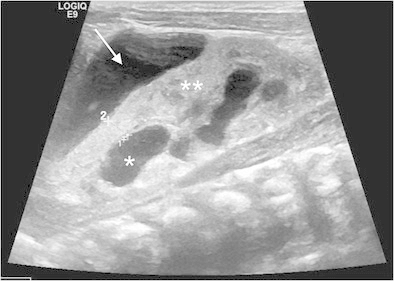
Figure below shows multiple, round anechoic lesions in the renal parenchyma indicating a cystic disease of kidney which has 2 differentials in fetal kidney:
- Multicystic dysplastic kidney (MCDK)
- Autosomal recessive polycystic kidney disease (ARPCKD)

This figure shows a tortuous, dilated ureter along with renal pelvis indicating a case of Hydroureteronephrosis.
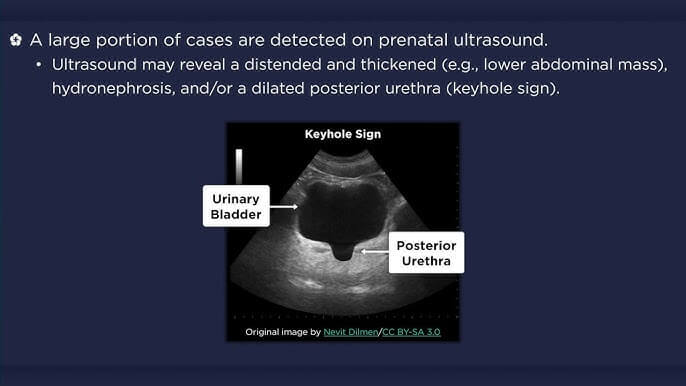
This picture shows thick trabeculated bladder along with dilated posterior urethra giving a classical “key hole sign” indicating posterior urethral valve
This picture shows a large collection around the kidney indicative of perinephric urinoma or urinary ascites. This is thought to be a protective “pop off mechanism” as a part of acclimatization to continuous high pressure from obstruction such that the renal parenchyma does not rupture.
In summary: a good USG should comment on –
- Number, size and location of kidney
- APRPD diameter
- Echogenicity of renal parenchyma
- Presence of cysts (if any)
- Pelvicalyceal dilatation
- Ureteral dilatation
- Bladder wall abnormalities (thickness, trabeculations, ureterocele)
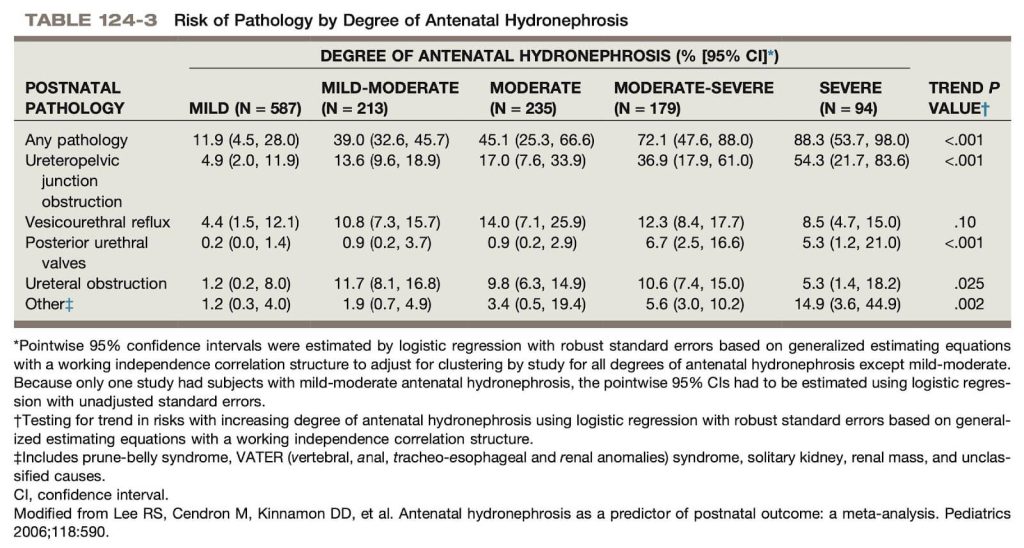
This was a landmark meta-analysis performed in 2006 to determine ANH as a predictor of postnatal outcome in terms of disease progression. All the disease progressed postnatally based on severity of ANH except VUR. So, this study concluded that ANH is not a predictor of progression of VUR postnatally.
What can be done antenatally?
The mainstay of management antenatally focuses primarily on monitoring of progression of disease via USG and parent counselling.
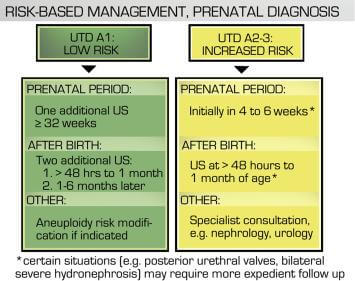
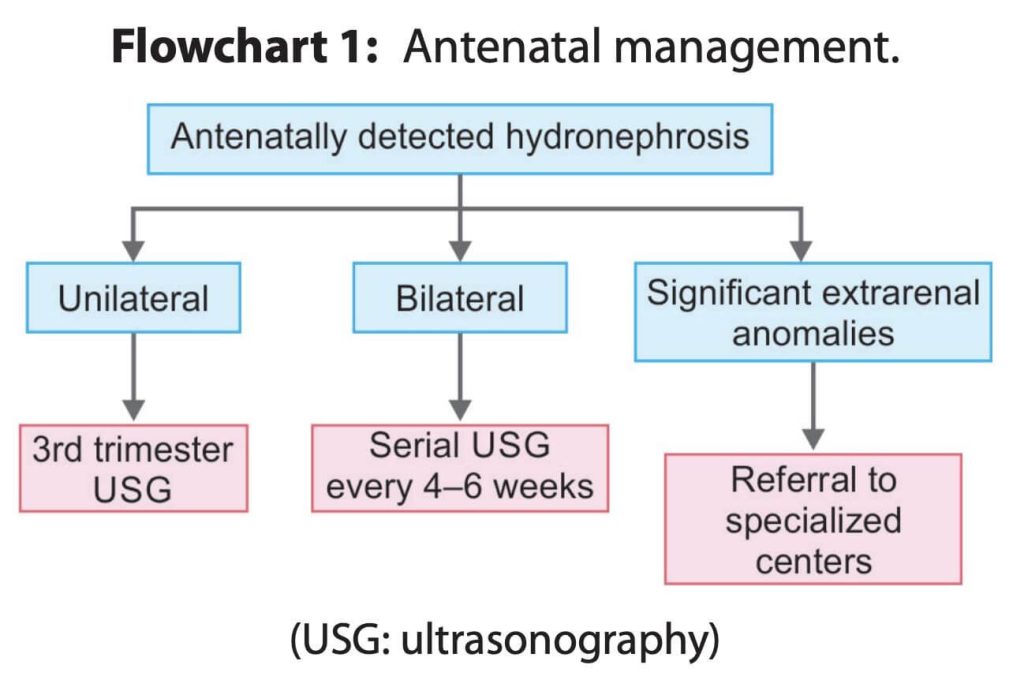
There are 2 recommendations on how to monitor a fetus antenatally.
1. UTD system recommendation
2. IAP (2022) recommendations:
Counselling antenatally:
- Is an integral part of management
- Should focus on:
- Reassurance and dispel misconceptions
- Provide a reasonable differential diagnosis
- Supply information regarding the natural history of disease
- Give antenatal recommendations
- Provide a post-natal management plan (discussed later)
Fetal intervention – rationale and indications:
It is uncommon and is not done usually as it has already been established that there are lots of risks to the mother and fetus and is expensive.
The major reason why fetal intervention can be tried in certain subsets of patient is to maximize pulmonary development; this is because most of the neonates with renal anomalies have associated oligohydramnios. Amniotic fluid is required for pulmonary development. Most of these neonates die postnatally due to complications related to pulmonary hypoplasia.
But before intervention risk benefit ratio should be taken into account which forms the basis of indications for fetal intervention which are listed below:
- Normal karyotype with no other associated systemic anomalies (E.g.: VACTERL)
- Adequate AFV up to 30 WOGS; as lung development would have more or less completed by then
- Non cystic kidneys
- Favorable urinary indices (Na<100mg/dl, Cl<110 mg/dl, osmolality<210 mg/dl, B2 micro-globulin<10 mg/L)
Modalities of intervention:
Both procedures have no survival benefit to one other [Morris et. Al, 2011].
1. In utero shunt placement
- USG guidance using Seldinger technique
- Vesicoamniotic shunt (Rodeck shunt)
- Shunt dislodgement, bowel herniation, need for amnioinfusion are attributed drawbacks
2. Fetoscopic approach
- Bladder cycling, no risks of dislodgement are attributed advantages
- Injuries to urethra, bladder neck and external urethral sphincter are attributed disadvantages
Clinical outcomes (long term) of fetal intervention:
- Long term outcomes – are mixed (this study followed up the child till mean age of 5.8 years)
- Acceptable renal function (44%), mild impairment (22%), renal failure (33%). Patient with prune belly syndrome – best outcome (57%) followed by PUV (43%) and urethral atresia (25%). [Biard and associates (2005)]
- PLUTO trial (Morris et al. 2013): landmark trial
- Compared VAS with conservative management (n:16 vs n:15)
- 12 live births in both; 4 vs 8 post-natal deaths at 28 days (all from pulmonary hypoplasia)
- Non-significant survival benefit
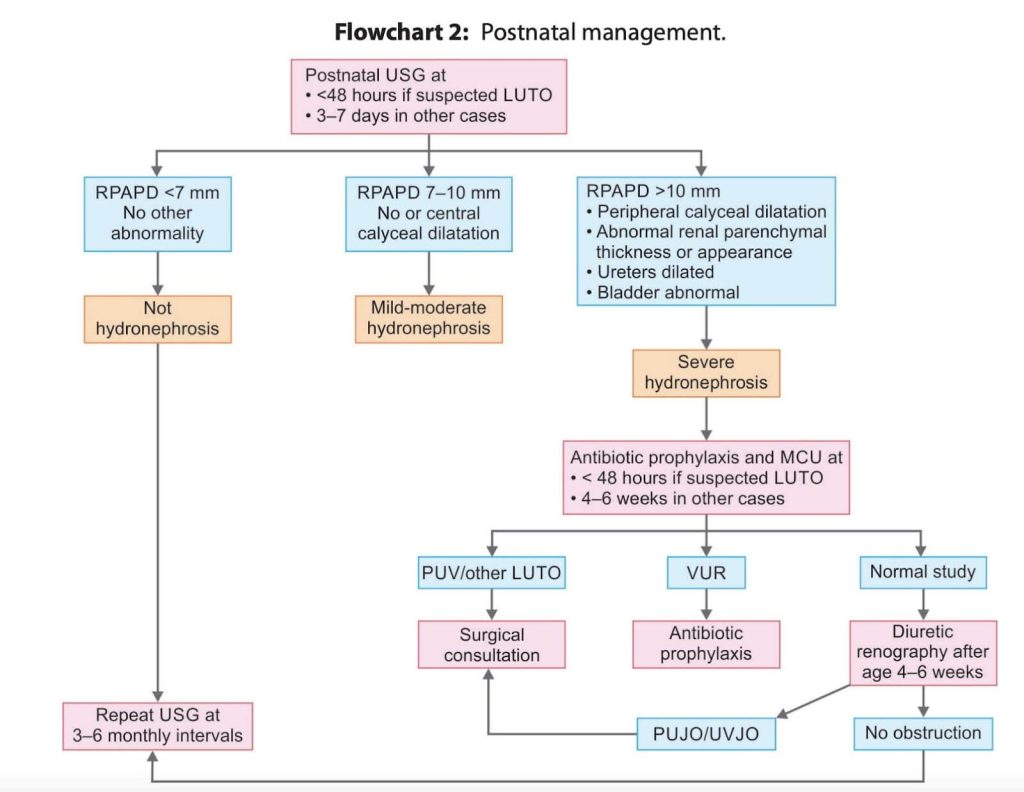
Post-natal management approach:
The main concept behind post-natal management is that:
- The most common cause of ANH is transient hydronephrosis of fetal development; it usually subsides within 48 hours and does not require any intervention
- So as a surgical resident when you get a call for ANH post natally we should not order USG within 48 hours as these will show hydronephrosis
- So, the major recommendation is to order an USG only after 48 hours of life and grade the degree of hydronephrosis
IAP 2022 approach:
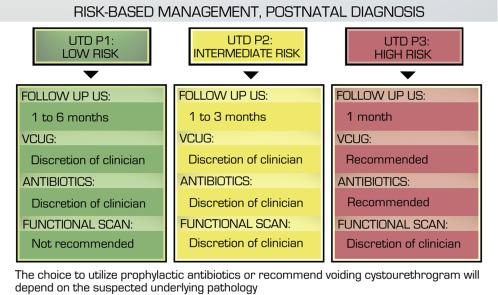
UTD approach:
Key recommendations:
- USG should be performed only after 48 hours of life
- Then grading of Hydronephrosis is done and managed according to above mentioned flow charts
- The VCUG/MCUG and nuclear scans should only be performed after 4-6 weeks as there will be transient VUR in newborn in first month of life and if these scans are performed earlier then it will overestimate the grades of VUR.
- CT scans are usually not done in children due to risks of radiation exposure; moreover, USG has an excellent resolution image comparable to CT; also, the cause of obstruction in neonates/child is not stone
- Management of underlying cause in accordance with the above investigations
The concepts about VCUG and nuclear scans will be further explored in next coming urology series.
References:
1. Campbell-Walsh Urology – 11th edition
2. Holocomb and Ashcraft’s pediatric surgery – 7th edition
3. IAP guidelines, 2022
4. Nelson’s textbook of pediatrics

He is an avid reader, guitar player, melodious singer and old songs lover. He has a passion for making medical knowledge accessible and comprehensive.