The incidence of THA dislocation is:
- Primary THA: 1-2%
- Revision THA: 5-7%
Mnemonic: WHAT caused the total hip arthroplasty dislocation?
Wear
Types:
- Volumetric wear: proportional to r2 (diameter of head)
- Linear wear (related to penetration of femoral head into liner): smaller heads have higher linear wear
- Adhesive wear (most important): PE particles pulled off from liner during gait cycle
- Abrasive wear: Rough femoral head scratches and damages PE liner
- Third body wear: Debris between 2 bearing surfaces scratches the weaker one
- Back-side wear: Between the liner and cup
- Run-in wear: Higher wear rate within 1st 1 million cycles of THA use (decreases thereafter)
- Stripe wear (ceramic head; vertical cup): Crescent-shaped line on femoral head and corresponding on cup, near edge (occurs from lift off separation when femoral head contacts the rim of the shell as it separates from the socket)
- Hip edge loading (over-abducted cup): stress concentrate on edge of acetabular shell
Mechanisms: Submicron sized wear particles are disseminated into effective joint space and are phagocytosed by macrophages; activated macrophages secrete osteolytic factors.
- Leverage: Eccentric wear of a polyethylene acetabular cup brings the implant neck closer to the acetabular rim, promoting leverage.
- Implant loosening
Head–neck ratio
Primary arc motion: It is the motion of artificial hip within the socket before any neck/liner or bony impingment occurs.
- Increased head-neck ratio = Increased primary arc motion
- Additions to acetabulum or neck decreases head-neck ration:
- Constrained acetabulum/acetabular hoods
- Neck skirt (femoral head collar on femoral stem)
Lever range or Excursion distance (Jump distance): Distance from the start of impingement to complete dislocation
- Larger heads have higher excursion distance (equal to radius of head)
Alignment
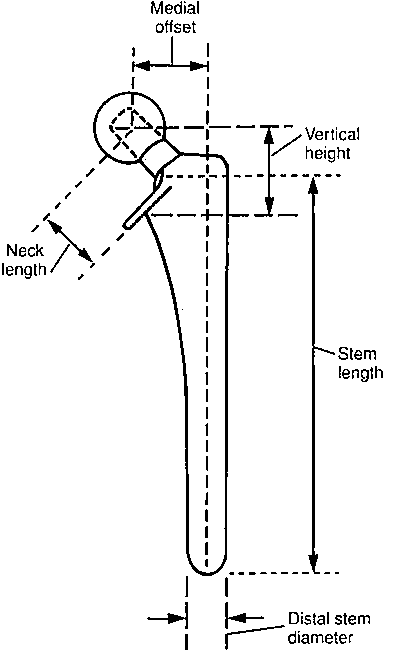
Offset determines static stability –
Vertical offset: Lesser trochanter to Center of femoral head (essential for correction of leg length)
Horizontal offset (Head-stem offset): Center of femoral head to the line through the axis of distal part of stem
- If reduced: Decreased abductor lever arm (weak abductor and increased joint reaction force) leading to increased risk of dislocation
- If excessive: Increases stress (stress fracture or loosening)
Neck length: Center of femoral head to base of collar
- If reduced: Shortens abductor muscle length and decrease hip offset (both lead to abductor weakness) and allows bony impingement of greater trochanter against pelvis during ROM
- Neck skirts and long neck: To compensate short femoral neck cut, decreases head/neck ratio and primary arc range
Implant positioning: determines static stability
- Acetabular cup anteversion: 15-30 degrees
- Retroversion: posterior dislocation
- Excessive anteversion: anterior dislocation
- Acetabular cup abduction (θ angle): 35-45 degrees
- High (vertical cup): postero-superior escape
- Low (horizontal cup): inferior dislocation
- Femoral stem anteversion: 10-15 degrees
- Retroversion: posterior dislocation
- Excessive anteversion: anterior dislocation
Tension
Tension refers to adequate abductor function (determines dynamic stability)
Weakness of abductors may be caused by:
- Posterior surgical approach
- CNS or neuromuscular diseases
- Decreased femoral offset
Besides, these the patient’s risk factors for dislocation are:
- Female
- THA for osteonecrosis
- Obesity
- Alcoholism
- Age >70 years
- Greater trochanteric non-union
Management of THA dislocation
1. Initial: Closed reduction and Immobilization (spica brace/cast and knee immobilizer) X6 weeks + Hip precautions/physiotherapy
2. Any component malposition: Revision (may need complete hip revision)
3. Normal component alignment with incompetent but intact abductor function: Greater trochanter advancement (Charnley tensioning)
4. Normal component alignment with abduction dysfunction: Revision to constrained liner (socket)
- Forces are transmitted to the cup/bone interface – catastrophic failure of the cup can occur instead of dislocation
5. Greater trochanteric escape: Greater trochanter pulls away from proximal femur
- Causes:
- Failed trochanteric fixation after revision THA
- Trauma with associated osteolysis
- Problems: Increased risk of dislocation due to –
- Abductor dysfunction leading to loss of hip compression
- Increased rotation (loss of restriction by greater trochanter)
- Greater trochanter fragment can impinge between hip and pelvis
- Treatment:
- Maximize head/neck ration
- Resect greater trochanter fragment
- Constrained cup (last resort)
References:
1. Crozier-Shaw G, Magill P. WHAT causes dislocation of a total hip arthroplasty; a simple mnemonic for the orthopaedic resident. Int Orthop. 2015 Mar;39(3):605-6. doi: 10.1007/s00264-014-2661-y. Epub 2015 Jan 21. PMID: 25720360.
2. Miller’s Review of Orthopedics – 7th Edition