Synonyms: Paradoxical pulse, Paradoxic pulse, Reversed Bernheim sign
Definition of Pulsus Paradoxus
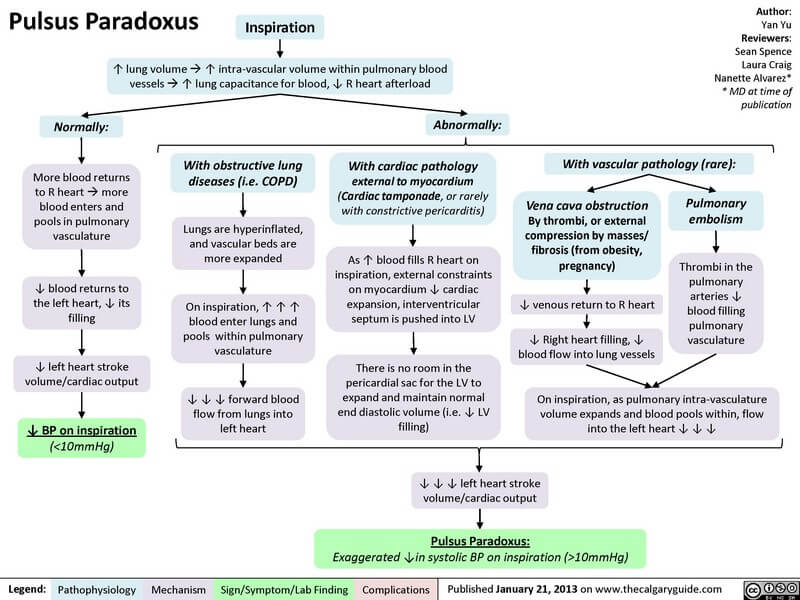
There is normal physiological fall in Blood pressure upto 10 mmHg during inspiration. Pulsus paradoxus is the exaggeration of this normal decline in blood pressure more than 10 mmHg during inspiration. The “paradox” refers to the fact that heart sounds may be heard over the precordium when the radial pulse is not felt.
Physiology of pulsus paradoxus
A) Normal physiology:
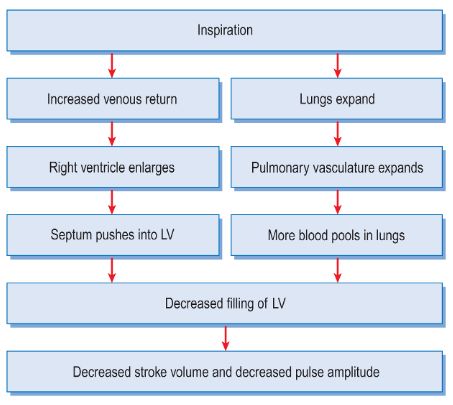
During inspiration there is fall in stroke volume and blood pressure due to following reasons:
1. Decrease in intra-thoracic pressure leads to increased venous return into the right atrium and subsequently into the right ventricle. Thus, the right ventricle enlarges and pushes the interventricular septum towards left, leading to decrease in the left ventricular volume.
2. As the lung expands, there is pooling of blood in the expanded pulmonary vasculature. As a result, the venous return to the left atrium and consequently on the left ventricle decreases.
B) Physiology of pulsus paradoxus:
The reasons behind exaggeration of this normal physiology in pulsus paradoxus may be one or more of the following:
- Limitation in increase in inspiratory blood flow to the right ventricle and pulmonary artery
- Greater than normal pooling of blood in the pulmonary circulation
- Wide excursions in the intrathoracic pressure during inspiration and expiration
- Interference with venous return to either atrium especially during inspiration
Causes of Pulsus paradoxus
1. Physiological:
- Pregnancy
- Extreme obesity
- Student’s paradox (exaggerated inspiration voluntarily)
2. Cardiovascular:
- Cardiac tamponade
- Effusive constrictive pericarditis
- Massive pulmonary embolism
- Severe hypovolemic shock (due to hemorrhagic or septic shock)
- Restrictive cardiomyopathy
3. Pulmonary:
- Chronic Obstructive Pulmonary Disease: Severe emphysema, Upper airway obstruction
- Acute severe bronchial asthma
Mechanism of pulsus paradoxus
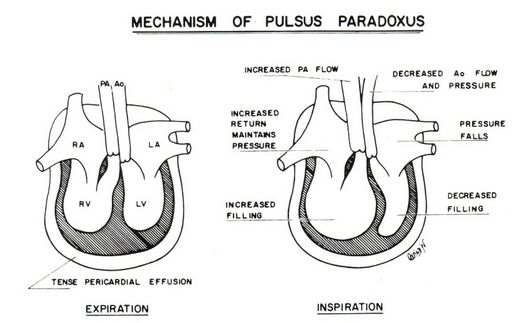
1. In cardiac tamponade:
There is decreased stroke volume due to:
- Impaired left ventricular filling
- Impaired right ventricular dilation resulting in bulging of interventricular septum into left ventricle
- Impaired decrease in intra-pericardial pressure while there is normal decrease in pressure of extra-cardiac vessels along with the decresase in intra-thoracic pressure. As a result, pressure in pulmonary vein is less compared to the left atrium resulting in sucking up of blood into the pulmonary vein from the left atrium which mean less filling of left ventricle.
2. In massive pulmonary embolism:
Right ventricular dysfunction or failure leads to decreased venous return to the left atrium and then to the left ventricle.
3. In respiratory disorders:
Increased airway resistance: There is wide excursion of intrathoracic pressure during inspiration and expiration. During inspiration, the introthoracic pressure falls more than normal and during expiration, the intrathoracic pressure rises more than normal.
Hyperinflation: Increased expansion of pulmonary vasculature leads to increased pulmonary pooling of blood during the phase of inspiration.
Pulsus paradoxus may be absent in Cardiac tamponade if associated with:
- Atrial Septal Defect
- Ventricular Septal Defect
- Aortic Regurgitation
- Pericardial adhesions
- Isolated right cardiac tamponade
- Conditions causing reverse pulsus paradoxus
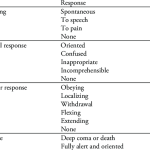
Bedside Measurement of Pulsus paradoxus using Sphygmomanometer
1. Find the systolic blood pressure during expiration:
- Inflate the sphygmomanometer to a level 20 mmHg greater than the patient’s systolic pressure.
- Slowly deflate the cuff (2 mmHg/s) and listen for appearance of the first Korotkoff sound.
- If the pressure is held at that level (i.e., if you stop deflating the cuff) in a patient with pulsus paradoxus, the Korotkoff sounds will drift in and out, audible with expiration, and absent with inspiration (systolic pressure falls below cuff pressure during inspiration).
2. Find the systolic blood pressure during inspiration:
- Now, slowly deflate the cuff until the sounds are first audible throughout the respiratory cycle (audible during both inspiration and expiration) i.e. the korotkoff sound changes from intermittent to constant.
3. Calculate the difference:
- Calculate the difference between the systolic blood pressure in expiration and inspiration.
4. Interpret:
- If the difference is > 10 mmHg, pulsus paradoxus is present.
Video showing correct technique for measurement of pulsus paradoxus
Other methods of measuring pulsus paradoxus:
- Invasive: Arterial wave form analysis
- Non-invasive: Pulse oximetry wave form analysis
Reverse pulsus paradoxus
Reverse pulsus paradoxus refers to inspiratory rise in the arterial pressure. It is seen in conditions like:
- Hypertrophic cardiomyopathy (Mechanism not known)
- Intermittent positive pressure ventilation (Intrathoracic pressure is higher during inspiration and lower during expiration)
- Atrioventricular dissociation (Presence of atrial activity in inspiration increases the stroke volume and its absence during expiration decreases the stroke volume)
Pulsus paradoxus as an indicator of severity of Acute Asthma
- Mild: 10 mmHg
- Moderate: 10-20 mmHg
- Severe: >10 mmHg




very good presentation loved it thank uuu
This is amazing, I understood everything perfectly, thanks a lot!
Thanks a lot.
I think the last part on using pulsus paradoxus to assess severeity of acute asthma in the severe form the fall in arterial pressure should be >20mmHg
Wao….nicely nd easily presented…specially the flow chart was very useful…thanku✌🖒☺
Good explanations …