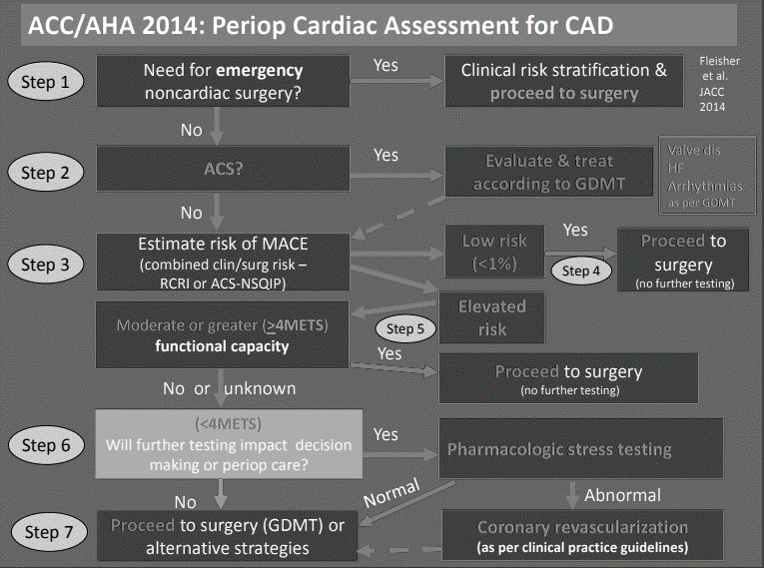
Besides, for the emergency/urgent surgeries, one needs to evaluate 4 variables in the preoperative cardiac evaluation of the patient for the non-cardiac surgery. We have elaborated the mnemonics used by CasesBlog. These variables can be remembered by the mnemonic PAST.
- Patient risk
- Activity level (METs)
- Surgical risk
- Test (Stress test) or Treat (Beta blockers)
1. Patient risk for Major Adverse Cardiac Events (MACE):
MACE can be calculated by variety of methods but the most commonly used is the Revised Cardiac Risk Index (RCRI). RCRI comprises of 6 variables each scored 1 which can be remembered using the mnemonic 4CHD.
- CAD (Coronary artery disease)
- CHF (Congestive heart failure)
- CVA (Cerebrovascular disease)
- CKD (Creatinine >2 mg/dl)
- High risk surgery (Discussed in point number 3)
- DM requiring insulin
RCRI score predicts risk of MACE as follows:
- 0 – 0.4%
- 1 – 1%
- 2 – 2.4%
- 3 or more – 5.4%
With MACE <1% (considered low risk), one can proceed to surgery. If MACE is 1% or more, i.e. more than 1 clinical risk factors (elevated risk), one needs to determine functional capacity with Metabolic Equivalent Tasks (METs).
2. Activity level (METs):
The determining level for surgery or testing is the 4 METs. If a patient can walk 4 mph or faster on level ground, climb a flight of stairs, walk up a hill, run a short distance, do heavy work around house, involve in recreational sports activities, the functional capacity of patient is 4 or more METs.
- 4 or more METs: Proceed to surgery
- <4 METs: Test (Stress test)
3. Surgical risk:
a. High risk (>5% risk of cardiac death or nonfatal MI): Aortic or major vascular surgery, Intraperitoneal surgery, Intrathoracic surgery
b. Intermediate risk (1-5% risk of cardiac death or nonfatal MI): Carotid endarterectomy, Head/neck surgery, Orthopedic surgery, Prostate surgery
c. Low risk (<1% risk of cardiac death or nonfatal MI): Ambulatory surgery, Endoscopic procedures, Superficial procedure, Cataract surgery, Breast surgery
4. Test (Stress test) or Treat (Beta blockers):
If RCRI >1% with <4 METs, pharmacological stress testing (using dobutamine, adenosine, etc.) is recommended.
Revascularization before noncardiac surgery is recommended in cases where revascularization would otherwise be indicated according to existing clinical practice guidelines; not recommended exclusively to reduce perioperative cardiac events.
Beta blockers should be continued in patients using them chronically. If there is ischemia on stress test of if ≥3 or more RCRI risk factors are present, it may be reasonable to begin perioperative beta blockers. When starting beta blockers before surgery, do so ≥1 day before (recommended ≥1 wk to 2 wks before; do not start on day of surgery – harmful in POISE study). More cardioselective beta blockers may be better.
Reference: 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery
2016 Canadian Cardiac Society (CCS) guideline emphasizes the use of biomarkers.
Send NT-proBNP or BNP if any 1 of CAR:
- Cardiovascular disease in 45-64 years aged
- Age 65 years or more
- RCRI 1 or more
Risk of death or MI based on NT-prBNP and BNP:
- NT-proBNP <300 ng/L or BNP <92 mg/L: ~5%
- No additional routine postoperative monitoring required
- NT-proBNP 300 ng/L or more or BNP 92 mg/L or more: ~22%
- Postoperative monitoring: Measure troponin daily X 48-72 hours, Obtain ECG in PACU
Reference: 2016 CCS guideline on perioperative cardiac risk assessment and management of patients undergoing noncardiac surgery