Cause of radiation cystitis: Bladder in the radiation field (treatment of pelvic malignancies like prostate, cervical, colorectal)
Epidemiology of radiation cystitis:
Incidence: 23% to 80% (variability due to variability in type and dosing of radiotherapy among different medical subspecialities)
- Incidence of severe hematuria: 5-8%
Mean duration for developing radiation cystitis: ~ 32 months after treatment
Gender: Males to female ratio of 2.8 : 1 (frequent use of radiotherapy in the treatment of prostate cancer)
Mean frequency of radiation cystitis 1 year after radiotherapy:
- Following treatment of prostate cancer: ~14%
- Following treatment of cervical cancer: ~5%
- Following treatment of bladder cancer: ~18%
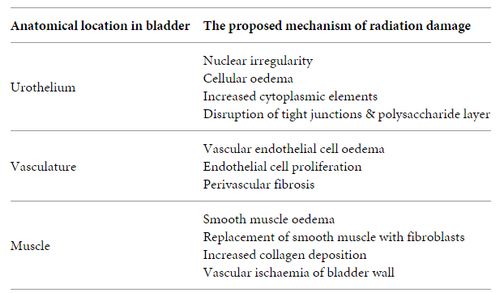
Pathophysiology of radiation cystitis:
The surface layer of urothelium is made of large polyploid cells connected by tight junctions and covered by a monomolecular film of sulfonated polysaccharides or glycosaminoglycan that serves the need for internal impermeability of the bladder. The tolerance dose for whole bladder has been estimated to be 65 Gy and for the 2/3rd bladder to be 80 Gy. Complication rate is dependent upon whole bladder dose and total radiation dose.
1. Mechanism of DNA damage by radiation:
- Indirect: Production of free oxygen radicals by interaction with intracellular water
- Direct: Point mutation of DNA (rare)
2. Bladder mucosa (Urothelium) is relatively sensitive to radiation as it divides rapidly.
3. Acute injury:
- Loss of tight junctions with resultant exposure of underlying tissues to hypertonic urine
- This leads to increase in immature and atypical cells
- Associated with onset of self-limited LUTS (Lower Urinary Tract Symptoms)
4. 3 months following radiotherapy:
- Intermediate and basal urothelial cells display nuclear irregularity, cellular edema and increased cytoplasmic elements
5. 6-12 months following radiotherapy:
- Urothelial proliferative activity and perivascular fibrosis is increased
- This leads to ischemic insult that can impact bladder urothelium and smooth muscle
- Replacement of bladder wall smooth muscle by fibrosis leading to loss of bladder compliance
6. Late toxicity (variable from 3 months to 3 years):
- Vascular endothelial cells and connective tissues that had sustained injury at the time of treatment begin to replicate but fail to regenerate adequately
- Resultant submucosal fibrosis and inflammation can lead to further ischemia with necrosis and ulceration
- This leads to neovascularization giving rise to superficial, fragile vessels responsible for bleeding in hemorrhagic cystitis
Microscopic pathology of radiation cystitis:
- Hemorrhage and hemosiderin, fibrin deposition, acute and chronic inflammation, edema and thickened mucosal folds, vascular ectasia, swollen endothelial cells, microvessel thrombi, atypical fibroblasts
- Degenerative type epithelial changes resembling carcinoma in situ but more bizarre including cytoplasmic ballooning, smudged chromatin, nuclear and cytoplasmic vacuoles, karyorrhectic cellular debris; these changes may persist for longer intervals in von Brunn’s nest
- May have pseudoinvasive urothelial nests wrapping around the vessels associated with fibrin deposition and hemorrhage – so called pseudocarcinomatous epithelial hyperplasia
- Late changes are blood vessels with myointimal proliferation and hyalinization, scattered atypical fibroblasts, intramural fibrosis with replacement of smooth muscle by collagen
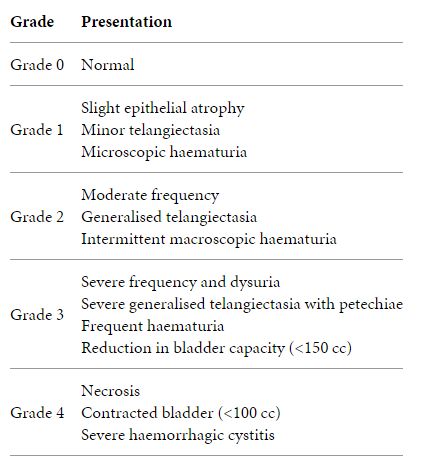
Diagnosis of radiation cystitis:
Aim: Exclusion of other causes of patient’s symptoms
- History and Physical examination:
- History of pelvic radiotherapy with or without chemotherapy that may aggravate cystitis e.g. cyclophosphamide
- Acute radiation cystitis occurs during or soon after radiation treatment. It is usually self-limiting, and is generally managed conservatively. Late radiation cystitis, on the other hand, can develop from 6 months to 20 years after radiation therapy.
- Acute sequelae (following >20 Gy): frequency and dysuria; resolution of symptoms in 2-3 weeks follpwing completion of radiotherapy
- Long-term sequelae: persistent dysuria, severe pain, contracted bladder, vesicovaginal fistula, and varrying degrees of hematuria
- Urinalysis and urine culture: to rule out UTI
- Urine cytology: In patients with high risk of bladder cancer
- CBC: to determine hemoglobin level, hematocrit and platelet level
- RFT and electrolytes: to determine renal function
- PT and aPTT: to rule out bleeding disorders
- Urodynamic studies:
- In acute cases: detrusor instability, decreased peak flow rate, decreased bladder complince, decreased bladder volume
- Cystoscopy:
- To rule out other possible bladder causes like stone or malignancy
- Pale, frosted bladder mucosa with scattered telangiectasias and sometimes well defined torpid ulcerations
- Therapeutic: If pathologically small bladder is found, hydrodistension can provide symptomatic relief
- Imaging modalities (IVP, CT urography, renal USG): To rule out other causes of hematuria and also in cases of suspected fistula
Prevention of Radiation Cystitis:
1. Accurately tailoring the irradiation field and limiting the radiation dose to the bladder
2. Unless medically contraindicated, provision of sufficient hydration to maintain adequate high urine flow should be a component of all prophylactic regimens.
3. Sodium hyaluronate 40 mg/50 ml is proposed as an option for patients considered at increased risk of Hemorrhagic Cystitis (e.g. patients receiving external beam radiation therapy and brachytherapy for cervical or endometrial cancer).
4. Treatment should be initiated with weekly instillations for six weeks, potentially followed by two fortnightly instillations, then maintained using monthly instillations whilst the patient is responding.
5. Drinking one large daily glass of cranberry juice may help to reduce the risk of HC. Cranberry juice tablets can also be used.
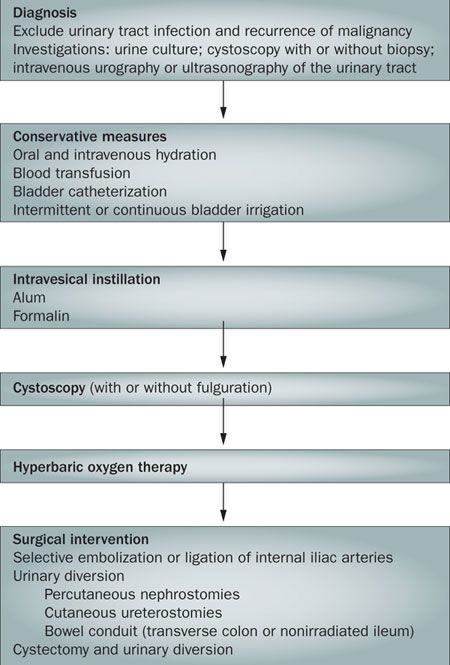
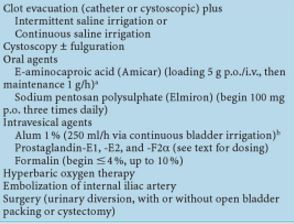
Treatment of Radiation cystitis:
1. Symptomatic relief:
- Analgesic: Phenazopyridine hydrochloride
- Antispasmodic: Oxybutynin chloride
2. Definite management:
References: 1. Radiation complications of the pelvis - Greven, Paunesku 2. Radiation therapy for pelvic malignancy and its consequences - Ehrenpreis, Marsh, Small 3. Radiation cystitis - Medscapr 4. A narrative review on the pathophysiology and management for radiation cystitis - Browne, Davis 5. Emergencies in Urology - Hohenfellner, Santucci



Hey dude, Iam absolutely loving articles on your blog. They are structured properly, easy to read and understand, in spite of English being my third language. Greetings.