Named after: German Surgeon August Bier (first introduced the block in 1908)
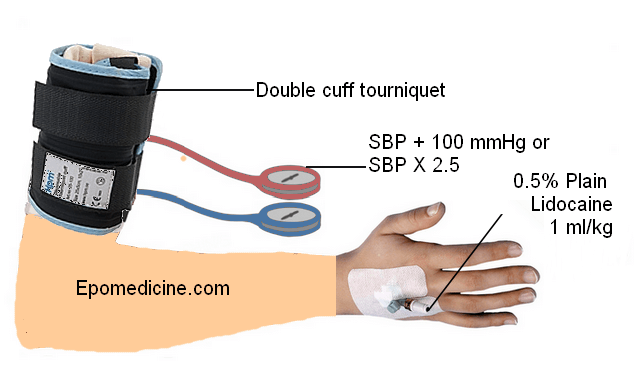
Definition: It is a peripheral intravenous local anesthetic block (IVRA; Intravenous Regional Anesthesia) of the upper limb using a pneumatic cuff technique
Mechanism of action: Local anesthesia diffuses into the small veins surrounding the nerves and then into the vasa vasorum and capillary plexus of the nerves, leading to centrifugal conduction block in the nerves involved. Local anesthetic then diffuses into the small nerves in the skin, blocking their conduction. The tourniquet produces ischemia, which contributes to the analgesic action of the local anesthetic by blocking nerve conduction and motor endplate function. 20 minutes after tourniquet application alone there will be analgesia to pinprick without the injection of any local anesthetic. However, the speed of onset and the density of anesthesia are greater with injection of local anesthetic.
Indications: Surgery of arm below the level of the cuff, usually at or below the elbow (duration: not to exceed 90 minutes); the same technique can be used for lower extremity surgery below the knee.
Minimum requirements for conducting Bier’s block:
- A well-lit, fully equipped area with resuscitation equipment
- Cardiac and blood pressure monitors, Pulse oximeters and Intravenous catheters
- Esmarch rubber or Ace elastic bandage
- A minimum of 2 practitioners present throughout, with 1 solely responsible for airway and resuscitative measure
- A double pneumatic tourniquet cuff is available and inflated and tested for 5 minutes prior to the procedure
- The cuff should be inflated for a minimum of 20 minutes and maximum of 45 minutes with clear documentation
Procedure:
a. Patient position: Supine with extremity to be blocked supported on a side table extension
b. Needle size: 20 or 22-gauge intravenous cannula in dorsum of hand away from surgical site.
c. Dose:
- Traditional: Lidocaine without adrenaline 3-5 mg/kg (0.5% plain Lidocaine 1 ml/kg upto 60 ml)
- Mini-dose: Lidocaine without adrenaline 1-1.5 mg/kg
- Prilocaine: 3 mg/kg (high margin of safety)
Bupivacaine should never be used due to its cardiotoxic profile.
d. Technique:
- Insert and tape IV catheter on the dorsum of the hand in the arm to be blocked. Insert large bore IV catheter in spare hand for emergency access.
- Apply appropriate sized pneumatic double cuff to the upper arm. The lower end of the distal cuff is secured with foam tape 10 cm to prevent migration. Check the integrity of both cuffs by sequential inflation and deflation.
- Elevate the arm and exsanguinate from distal to proximal direction using Esmarch bandage.
- Sequence for initial tourniquet management:
- Tourniquet pressure: 100 mmHg above the systolic blood pressure or at-least 250 mmHg
- Inflate distal cuff
- Inflate proximal cuff
- Deflate distal cuff
- Absence of brachial and distal pulses indicates correct function
- Bring the arm back to horizontal position and slowly inject appropriate dose of local anesthetic (20 ml/min). The forearm discolors and the patient perceives a transient ‘pins and needles’ sensation and warmth as anesthesia ensues over the following 5 minutes.
- For short procedures, the cannula can be removed. if surgery may extend beyond 1 hour, the cannula can be left in place and reinjected after 45 minutes.
- When the tourniquet pain is reported about 25 to 30 minutes after the beginning of anesthesia, inflate the distal cuff and deflate the proximal cuff (upto an additional 30 minutes). If the surgery is completed in <20 minutes, do not deflate the cuffs. To prevent local anesthetic toxicity reactions, the tourniquet should remain in place for at least 40-45 minutes. Be vigilant for signs of systemic absorption during tourniquet release.
References:
- Clinical Anesthesia 6th Edition – Paul G Barash
- Anesthesia key – Bier Block
- Rockwood and Wilkin’s Fractures in Children
- Challenging Concepts in Emergency Medicine: Cases with Expert Commentary edited by Fleur Cantle, Sam Thenabadu, Chris Lacy
- Peripheral nerve blocks – A Color Atlas by Jacques E Chelly