SIEVE triage system
Mnemonic: ABC-30-2 Can Do
- Can walk to called area (Green): Delayed Priority 3
- Airway not open (Red): Immediate Priority 1
- Breathing (RR):
- No (after airway repositioning): Dead (Black) – Priority 4
- <10 or >30: Red
- 10-30:
- Circulation (CRT):
- <2 sec: Yellow (Urgent Priority 2)
- >2 sec (Red)
- Circulation (CRT):
Approach to assessment and initial management
Mnemonic: ARM
- Awareness (history and accident mechanism to predict likely injuries)
- Recognition (examine systematically in sequence of look-listen-feel in ‘ABC’ of trauma assessment)
- Management:
- ABCDE approach
- Catastrophic hemorrhage: C-ABCDE approach
Adjuncts to Primary Survey
Reflects the adequacy of resuscitation.
Mnemonic: PEA COVER
- Pulse oximetry
- EtCO2
- ABG
- Catheter (NG tube and Urethral)
- Output (urinary)
- Vital signs
- ECG
- Radiographs (Trauma series) and FAST
Primary Survey
Follow the look, listen, feel approach –
Mnemonic: ABCDE
1. Airway and C-spine protection:
- Chin lift: not performed if C-spine injury suspected
- Jaw thrust: performed if C-spine injury suspected or those with small jaw or thick neck
- Oropharyngeal airway (only used in obtunded patients without gag reflex): length measured from corner of mouth to external auditory canal
- Nasopharyngeal airway (approximately size of the casualty’s little finger): do not attempt if suspected cribiform plate fracture
- LMA: size –
- small women #3, large women and smaller men #4, large men #5
- volume for air for cuff inflation: (LMA size – 1) X 10 ml
- Tracheal intubation: Indicated in 6 “A” –
- Apnea
- Airway not maintained by other means
- Aspiration risk
- Airway obstruction impending (inhalational burn, expanding neck hematoma, facial fractures)
- Airway can’t be maintained by brain (GCS </=8)
- Adequate oxygenation and ventilation not maintained
- Drug assisted intubation (previously known as RSI):
- In patients with intact gag reflexes
- Etomidate or Succinylcholine
- Can’t intubate, Can’t ventilate (go for surgical airway):
- Needle cricothyroidotomy
- Surgical cricothyroidotomy (intubation or tracheostomy through cricothyroid membrane) – not recommended for <12 years (risk of cricoid damage)
2. Breathing:
- Identify life-threatening chest injuries (ATOM-FC)
- Look for signs of pneumothorax if intubated and ventilated (simple can worsen to tension one)
- Tension pneumothorax:
- Triad
- Absent breath sounds on affected side
- Trachea deviated away
- Hyper-resonance on affected side
- Immediate management: Needle decompression –
- Adults: 4th/5th ICS in MAL (mid-axillary line)
- Children: 2nd ICS in MCL (mid-clavicular line)
- Place chest drain as soon as possible
- Triad
- Open pneumothorax:
- “flap valve effect” will sequentially lead to tension pneumothorax
- Immediate management: occlusive dressing; place chest drain as soon as possible
- Massive hemothorax:
- Surgical referral and thoracotomy
- Cardiac tamponade:
- Beck’s triad:
- Distended neck veins (elevated JVP)
- Muffled heart sounds
- Hypotension
- Needle pericardiocentesis (subxiphoid approach): 18-22 G needle attached to syringe is inserted between xiphisternum and left costal margin, directed towards left mid-clavicle (shoulder) in 30-45 degrees angle to skin
- Beck’s triad:
- Flail chest:
- >/= 3 ribs broken at 2 places = floating segment in ‘paradoxical’ respiration
- Management: Oxygen, analgesia (epidurals may be required), ventilation (for profound hypoxia)
- Airway (tracheobronchial tree) disruption:
- Deceleration injuries
- Persistent pneumothorax, pneumomediastinum, pneumopericardium, air below deep fascia of neck
- Immediate management: Intubation of opposite lung or bronchial blocker
3. Circulation and control of hemorrhage
- 1 mm depth of edema across body surface = 1.5 L fluid loss (third space)
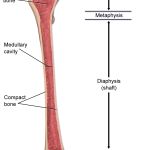
- Look for “bleeding onto the floor, and four more”: external bleeding, chest, abdomen, pelvis/retroperitoneum, long bones
- eFAST or CT
- To control hemorrhage: 2 tourniquets should be applied to lower limbs and 1 to the arm
- Open IV line with 2 large bore cannulas (atleast 18G) into large peripheral veins, preferably antecubital fossa
- Consider IO or central lines if peripheral IV access cannot be obtained.
- “One person, one try, one minute.”
- Consider IO or central lines if peripheral IV access cannot be obtained.
- Tranexamic acid 1 gm over 10 min stat and 1 gm 8 hrly for active/suspected active bleeding (given within 3 hour of trauma)
- Initial bolus of 1L warm isotonic fluid (adults) or 20 ml/kg for children </= 40 kg
- Primary indicator of response to fluid therapy: Urine output
- 0.5 ml/kg/hr: adults
- 1 ml/kg/hr: children
- 2 ml/kg/hr: children <1 year age
- Massive transfusion:
- Defined as >4 units in 1 hour or > 10 units in the first 24 hours.
- Balanced/hemostatic/damage-control resuscitation = administration of pRBCs, plasma, and platelets in a balanced ratio
- For Stage 4 Hemorrhagic shock
4. Disability (neurological status)
- GCS or AVPU scale
- Mild head injury (80%): GCS 13-15
- Moderate head injury (10%): GCS 9-12
- Severe head injury (10%): GCS 3-8
- Signs of basal skull fractures:
- Periorbital ecchymosis (raccoon or panda eyes)
- Retroauricular ecchymosis (battle sign)
- Otorhinorrhea (CSF leak from nose and ears)
- VIIth and VIIIth cranial nerve palsy
- ICP reduction: IV mannitol 0.5 mg/kg or hypertonic saline
- Expanding intracerebral hematoma: Evacuate within 4 hours
5. Exposure and Environment
Secondary Survey
History
Mnemonic: AMPLE
- Allergies
- Medications
- Past illness
- Last meal
- Events surrounding the injury
Head to toe examination
Following history, perform a sequential head to toe examination (extremities/musculoskeletal and neurological assessment is done towards the end).
- Head
- Maxillofacial
- C-spine
- Chest
- Abdomen
- Pelvis
- Perineum
- Orifices (PV/PR)
- Musculoskeletal
- Neurologic
Adjuncts to secondary survey
Mnemonic: ABCDE
- Angiography
- Bronchoscopy
- CT: head, chest, abdomen, spine
- Contrast urography
- Double E:
- Esophagoscopy
- Esophageal ultrasound (transesophageal USG)
Life threatening chest injuries (Primary survey)
Mnemonic: ATOM-FC in Airway and Breathing assessment
- Airway obstruction or disruption
- Tension pneumothorax
- Open pneumothorax (sucking chest wound)
- Massive hemothorax
- Flail chest
- Cardiac tamponade (FAST is 90-95% accurate)
- Circulatory arrest
Potentially life-threatening chest injuries (Secondary survey)
Mnemonic: ABCDEFS in Breathing assessment
- Aortic disruption
- Blunt cardiac injury
- Contusion of heart or lungs
- Diaphragmatic rupture
- Esophageal rupture
- Fistula (bronchopleural) and other tracheobronchial injury
- Simple pneumothorax or hemothorax
Handover protocol
Mnemonic: MIST
- Mechanism and time of injury
- Injuries found and suspected
- Symptoms and signs
- Treatment initiated
Massive hemothorax
Rule of “3”
Massive hemothorax is defined by the need for thoracotomy guided by volume drained after thoracostomy –
- Initial drainage > 1/3rd of blood volume (>1,500 ml)
- Drainage >3 ml/kg/hr of blood volume over 3 consecutive hours (>200 ml/hr for 3 consecutive hours)
ATLS 80/70/60 rule for palpable blood pressure
NEXUS criteria and Canadian C-spine rule for C-spine clearance
Indications of CT head
As per Royal College of Surgeons (RCS):
Mnemonic: VAGABONDS
- Vomiting >1 episode
- Amnesia of events >30 minutes before impact
- GCS <15 for >2 hours after initial assessment
- Amnesia post-injury if: ABC
- Age >65 years
- Bad injury, i.e., dangerous mechanism (pedestrian vs motor vehicle, motor vehicle ejection, fall from height >1 m)
- Coagulopathy
- Basal skull fracture
- Open skull fracture
- Neurological deficit (focal)
- Depressed skull fracture
- Seizure (post-traumatic)
Hemorrhagic Shock Stages
Think of the scores in a game of tennis: Love – 15 – 30 – 40 — game over (>40)
Remember: In stage 2, CRT is more than 2 sec.
- Stage 1: <15% blood loss (<750 ml, considering adult blood volume of 5 L)
- Stage 2: 15-30% blood loss (750-1500 ml)
- Stage 3: 30-40% blood loss (1500-2000 ml)
- Stage 4: >40% blood loss (>2000 ml)
| Stage | Pulse | Pulse pressure | SBP | RR | Mental status | Treatment |
| 1 | <100 | Normal | Normal | 14-20 | Normal | Crystalloid |
| 2 | 100-120 | Narrow | Normal | 20-30 | Anxious | Crystalloid |
| 3 | 120-140 | Narrow | Decreased | >30 | Confused | Crystalloid + Blood |
| 4 | >140 | Narrow | Decreased | >30 | Obtunded | Crystalloid + Blood |
Normal children blood volume: 8-9% body weight
Abdomen and Pelvic Injuries – Adjuncts
Mnemonic: CDEFG
1. CT: hemodynamically stable and no indication of emergency laparotomy
2. DPL (requires gastric and urinary decompression prior): Go to laparotomy if:
- Aspiration of GI contents, vegetable fibers, or bile
- Aspiration of 10 ml or more of blood
3. Emergency exploratory laparotomy:
- Positive CT, DPL or FAST
- Hypotension with an abdominal wound that penetrates the anterior fascia
- GSW that traverses the peritoneal cavity
- Evisceration
- Bleeding from the stomach, rectum, or GU tract following penetrating trauma
- Peritonitis
- Free air, retroperitoneal air, or rupture of the hemidiaphragm
4. FAST: Pericardial sac, Hepatorenal fossa, Splenorenal fossa, Pouch of Douglas
Fat Embolism Syndrome – Gurd’s criteria
Mnemonic: CPR RFT FAT EJR
A. Major criteria: CPR
- Cerebral involvement
- Petechial rashes
- Respiratory insufficiency
B. Minor criteria: RFT FAT EJR
- Retinal involvement
- Fever >38.5 C
- Tachycardia (>110/min)
- Fat macroglobulinemia
- Anemia
- Thrombocytopenia
- ESR increased
- Jaundice
- Renal signs
Definitive diagnosis = 1 Major + 4 Minor criteria
Damage Control Orthopedics (DCO) – Indications
Mnemonic: ABCDEFGH
a. Acidosis: base deficit >/= 8
b. Blood transfusion: >10 Units of packed cells
c. Cold temperature: <35 c
d. Damage: ABC
- Abdominal and/or pelvic trauma with hemorrhagic shock
- Bilateral lung contusions
- Chest trauma with ISS >20 or ISS >40 without Chest trauma
e. Extremis (ongoing uncontrolled blood loss despite resuscitation) or Unstable (hemodynamically unstable despite initial intervention)
f. Femoral fractures: Bilateral
g. Geriatric patients: >65 years
h. Hours: >90 minutes operative time
Revised Trauma Score (RTS)
Mnemonic: Three “B”s
The “SORT” triage system uses the same 3 categories.
- Brain injury (GCS)
- Blood pressure (SBP)
- Breathing rate (RR)
RTS = 0.93 X GCS + 0.73 X SBP + 0.3 X RR
RTS <4: Transfer to trauma center
Predicted mortality with RTS:
- 0: >99%
- 6: 36%
- 10: 10%
- 12: <1%
Injury Severity Score (ISS)
3 most severe injuries (out of maximum score 6) in 3 body systems (out of 6) if designated as A, B and C respectively.
ISS = A² + B² + C² (maximum 75)
- If any of the system scores “6”, ISS is automatically 75.
6 Body systems:
- Head and neck
- Face
- Chest
- Abdomen
- Extremities (including pelvis)
- External injuries
| Severity | AIS (Abbreviated Injury Scale) | ISS |
| No injury | 0 | |
| Minor | 1 | 0-8 |
| Moderate | 2 | 9-15 |
| Serious (Non-life threatening) | 3 | 16-24 |
| Severe (Life threatening) | 4 | 25-49 |
| Critical | 5 | 50-74 |
| Unsurvivable | 6 | 75 |
Trauma Score and Injury Severity Score (TRISS)
Mnemonic: T-R-ISS-A
- Trauma type: Blunt or Penetrating
- RTS
- ISS
- Age
Formula for calculation of TRISS is complex.
SIRS criteria
Acute Respiratory Distress Syndrome (ARDS) Definition
Berlin’s criteria –
Mnemonic: ARDS
- Acute (within 1 week of clinical insult or worsening respiratory symptom)
- Ratio (PaO2/FiO2) with PEEP or CPAP >/=5 cm H2O:
- Mild: 200-300
- Moderate: 100-200
- Severe: <100
- Diffuse bilateral chest x-ray infiltrates (not explained by effusion, collapse or nodules)
- Swan-Ganz catheter (PCWP) <18 mmHg

He is the section editor of Orthopedics in Epomedicine. He searches for and share simpler ways to make complicated medical topics simple. He also loves writing poetry, listening and playing music.