HISTORY AND EXAMINATION
Mnemonic: LIMPINGS
1. Limping definition and onset
- Any deviation in walking pattern away from the expected normal pattern for the child’s age
- Limping is never normal
- Acute
- Acute infections
- Trauma
- Leukemia
- Unstable SCFE
- Epidural abscess
- Chronic
- SCFE
- DDH
- Neoplasm
- Child abuse
- Neuromuscular conditions
- Leukemia
2. Injury
Mnemonic: Traumatic causes can be remembered using FAST
Trauma is the most common cause of limping in any age.
- Fractures and Foreign body:
- Acute fractures
- Stress fractures
- Vertebral end plate fracture
- Foreign body
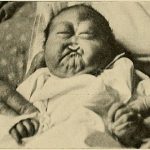
- Abuse (Nonaccidental injury)
- Slipped capital femoral epiphysis (SCFE)
- Soft tissue injuries (strains and contusions)
- Toddler’s fracture (tibia, calcaneus, cuboid)
3. Mechanical symptoms and Milestones
Mechanical symptoms like popping, clicking, locking –
- Osteochondritis dissecans (OCD)
- Discoid meniscus
- Meniscal injuries
A failure to achieve appropriate developmental milestones warrants a neuromuscular and/or metabolic workup.
4. Pain:
| Age | Painful limp | Pain-less limp |
| In all patients | Trauma (fracture, hemarthrosis, soft tissue) Infection (septic arthritis, osteomyelitis, discitis) Primary or metastatic neoplasm Juvenile Idiopathic Arthritis (JIA) | Developmental dysplasia of hip (DDH) Neuromuscular disorders Limb length discrepancy |
| 0-3 years | Transient synovitis Toddler’s fracture Non-accidental injuries Discoid lateral meniscus | |
| 4-10 years | Transient synovitis Rheumatic fever Perthe’s disease Discoid lateral meniscus Leukemia Sever’s apophysitis Accessory tarsal navicular Foreign body in foot | |
| >11 years | Stress fracture Slipped capital femoral epiphysis (SCFE) Osgood-Schlatter disease Sinding-Larsen-Johanssen syndrome Osteochondritis dissecans (knee/ankle) Chondromalacia patellae Accessory tarsal navicular Tarsal coalition |
Night pains:
- Growing pain
- Malignancies
Morning pains: Inflammatory disorders and overuse injury (stress fracture)
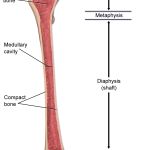
Constant, unremitting pain: Intramedullary process such as tumor or infection
5. Inflammatory symptoms: Morning stiffness, improvement with activity
- Juvenile idiopathic arthritis
- Seronegative spondyloarthropathies
- Stress fracture
6. Neurological symptoms: Weakness, altered sensation
- Cerebral palsy
- Spina bifida
- Duchenne muscular dystrophy
- Spinal cord tumor
- Hereditary sensory motor neuropathies
- Friedrich ataxia
- Tethered spinal cord
7. Gait and Gower’s sign
- Children do not achieve a mature gait until the age of 3 and an adult gait until the age of 7
- Toddlers walk with a wide-based gait, increased flexion of the hips and knees, and spend an increased amount of time in double stance phase to maintain balance
- 5 common types of limping gait have been listed below –
| Antalgic | Equinus (toe walking) | Trendelenburg | Circumduction | Steppage |
| Causes of painful limp | Idiopathic | Perthe’s disease | Limb-length discrepancy | Cerebral palsy |
| Clubfoot | DDH | Cerebral palsy | Myelodysplasia | |
| Cerebral palsy | SCFE | Any cause of knee or ankle stiffness | Charcot-Marie-Tooth disease (“marionette gait) | |
| Limb-length discrepancy | Hemiplegic cerebral palsy | Friedrich’s ataxia |
Gower’s sign: Child uses the hands to climb up the thighs (proximal compensation for distal weakness) when asked to get up from the floor. It can be seen in any condition that is associated with weakness of the pelvic girdle or proximal muscles of lower extremities:
- Duchenne muscular dystrophy and other muscle dystrophies
- Spinal muscular atrophy
- Discitis
- Juvenile idiopathic arthritis
8. Systemic symptoms: Fever, irritability, weight loss, anorexia
- Infective causes
- Tuberculosis of bone
- Bone malignancies
- Systemic causes: Appendicitis, Testicular/ovarian torsion, Pyelonephritis
WORKUP
1. First step: Orthogonal X-ray views of affected limb +/- Oblique views (especially in foot)
- Factures and Perthe’s disease are 2 most common conditions diagnosed on plain X-rays
- May identify osseous lesions or joint space widening consistent with effusion
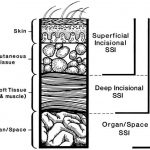
2. Suspected musculoskeletal infection or malignancy: MRI with and without contrast
3. Screening the entire skeleton in child abuse, suspected discitis, pelvic osteomyelitis, and osteoid osteoma or detecting overuse injuries and stress fractures: Bone scan
4. Detecting effusion: USG (cannot differentiate sterile effusion from septic effusion)
5. Acute, non-traumatic limp and systemic features or localized complaints:
- Initial testing: CBC, ESR, CRP, ANA, RF
- ESR rises within 24-48 hours and returns to normal over 3 weeks
- CRP rises within 6 hours and returns to normal over 6-10 days
- In suspected septic arthritis: Joint aspiration and Blood cultures (positive in only 40-50% cases)
- In suspected childhood leukemia: Peripheral blood smear
TREATMENT
Treatment depends upon the diagnosis of the cause of limping.
1. Non-operative
- Most causes are amenable to non-operative treatment
- Transient synovitis: With bed rest and anti-inflammatory medication, the child may be markedly improved by the next morning and complete resolution is seen in 1-2 weeks
- Routine joint aspiration is not recommended
2. Operative
- Septic hip arthritis, Epidural abscess and Unstable SCFE
Transient synovitis vs Septic Arthritis
References:
1. Elzouki, A. Y., Harfi, H. A., Nazer, H. M., Stapleton, F. B., Oh, W., & Whitley, R. J. (Eds.). (2012). Textbook of Clinical Pediatrics. doi:10.1007/978-3-642-02202-9
2. Staying Out Of Trouble With A Limping Child

He is the section editor of Orthopedics in Epomedicine. He searches for and share simpler ways to make complicated medical topics simple. He also loves writing poetry, listening and playing music.