Synonyms: Oedema, Swelling
Definition of Edema
Accumulation of excessive amount of fluid in the extravascular interstitial space of the body. Interstitial space is the extravascular compartment of the extracellular fluid and surrounds the cells of a given tissue. Anasarca is a severe and generalized edema with profound subcutaneous tissue swelling. Further reading about basics of fluid compartment and fluid therapy: Basics of fluid therapy.
Some related terms:
- Swelling: Transient abnormal enlargement of a body part or area not due to cell proliferation (not necessarily edema).
- Effusion: Accumulation of excessive fluid in the body cavities.
Pathophysiology of Edema
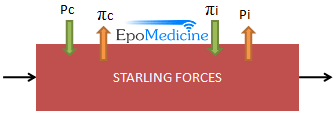 Starling forces determine fluid movement through capillary membranes:
Starling forces determine fluid movement through capillary membranes:
- Pc = capillary hydrostatic pressure
- Pi = interstitial fluid hydrostatic pressure
- πc = plasma oncotic pressure
- πi = interstitial fluid oncotic pressure
Note: The hydrostatic pressure pushes fluid out and the oncotic pressure pulls fluid into the respective compartments.
Thus, net fluid flow = Pnet = Kf [(Pc − Pi) − (πc − πi)].
Kf = filtration constant (capillary permeability).Edema—excess fluid outflow into interstitium commonly caused by:
- ↑ capillary hydrostatic pressure (↑ Pc; heart failure)
- ↓ plasma proteins (↓ πc; nephrotic syndrome, liver failure)
- ↑ capillary permeability (↑ Kf; toxins, infections, burns)
- ↑ interstitial fluid oncotic pressure (↑ πi; lymphatic blockage)
Demonstration of edema clinically
A. Inspection:
- The overlying skin may be smooth, shiny, taut and even hairless.
- There may be loss of normal small skin wrinkles, obliteration of dorsal finger joint creases, obscurity of metacarpal head definition and of the dorsal finger extensor tendons.
- There may be loss of normally distinct appearing edges of medial malleoli.
- Observe for puffiness of eyelids and face and also the scrotal edema.
- Observe for signs of inflammation if any.
B. Palpation:
Press with your right thumb over the following bony backgrounds for 5-10 seconds (different on different books!):
- Medial malleouls
- 5 cm above medial malleolus
- Shin of tibia
- Sacrum (in case of non-ambulatory patients) – ask patient to sit fo
- Rib or sternum
- Forehead (In case of anasacra)

Demonstrating slight edema:
- Press on a skin over bony area for 10 seconds with atleast 3 fingers spread slightly apart
- Feel for “valleys between hills” after release
Pit recovery time (PRT):
- Press down firmly all the way to the bone. Start the stopwatch.
- Shine a light at a tangent across the pit and do not call the pit recovery time until there is no shadow remaining anywhere in the area of the pit.
- Interpretation:
- Hypoalbuminemia: PRT is < 40 seconds (fast edema)
- Normo-albuminemia with increased venous pressure or increased capillary permeability: PRT is >40 seconds (slow edema)
How much body fluid may collect in tissue before pitting occurs ?
Ans: Atleast 10 lb (4.5 kg)
C. Examine for parietal edema: Press over or pinch the skin of abdominal wall for atleast 5 seconds and look for pitting edema.
D. Test for Lymphedema (Stemmer’s Sign):
Attempt to pinch and lift skinfold at the base of the second toe (or middle finger) – the test is negative if you are able to pinch skin and positive if you are unable to pinch skin.
- Negative: Suggestive of other cause of edema
- No swelling at base of digit: suggestive of chronic Venous Insufficiency
- Pitting swelling of the base of digit: suggestive of CHF, Nephrotic Syndrome, Cirrhosis, etc.
- Positive: Lymphedema
E. Percussion (For Ascites):
- Puddle sign: 120-250 ml (Mild ascites)
- Fullness of flanks: > 500 ml fluid
- Shifting dullness: > 1000-1500 ml fluid (Moderate ascites)
- Fluid thrill: >2000 ml fluid (Tense ascites)
Quantitative Assessment of Edema
1. Circumferential or girth measurement – remember to use same tape, same bony reference point, same measurement technique and if possible the same time of the day.
2. Volumetric water displacement – use same time of the day and same temperature of water; volume of the extremity can be determined by the volume of water displaced from the volumeter when the extremity is submerged.
3. Functional performance limited by edema
Grading of Edema
A) Pitting edema scale:
1+ : ≤ 2mm pitting that disappears rapidly
2+ : 2-4 mm pitting that disappears in 10-15 seconds
3+ : 4-6 mm pitting that may last more than 1 minute; dependent extremity looks fuller
4+ : 6-8 mm pitting that may last more than 2 minute; dependent extremity is grossly distorted
B) Severity of Bilateral pitting edema:
1+ (mild): Both feet/ankles
2+ (moderate): Both feet + lower legs, hands or lower arms
3+ (severe): Generalized bilateral pitting edema, including both feet, legs, arms and face
Types of Edema fluid
| Transudate | Exudate | Lymph |
| Protein-poor (< 3 g/dl) Cell-poor | Protein-rich (>3 g/dl) Cell-rich | Protein-rich |
| Pitting edema | Non-pitting edema | Non-pitting edema |
Classification and Causes of Edema
1) Non-pitting/Solid/Brawny Edema
- Myxedema: Generalized (Hypothyroidism) and Pretibial (Grave’s disease)
- Lymphedema: Primary or secondary
- Angioneurotic/Qincke’s edema and urticaria
- Scleroderma
Note: Non-pitting edema are usually localized type of edema but generalized type may be seen in cases of generalized myxedema and generalized urticaria (hypersensitivity to drugs).
Differentials for Lymphedema
By etiology:
- Primary lymphedema: Alteration or deficiency with lymphatic collection or transportation system
- Milroy disease (Hereditary lymphedema type I): Appears at or soon after birth
- Meige disease (Hereditary lymphedema type II): Develops later
- Lymphedema parecox: Another term for 2 syndromes described above, has an early onset upto 35 years
- Lymphedema tardum: Similar to lymphedema parecox but has an onset after 35 years
- Lymphangioms
- Secondary lymphedema:
- Infection: Filariasis, Reccurent cellulitis, Lymphogranuloma venereum, Scrofula (TB lymph node)
- Inflammation: SLE, Rheumatoid arthritis, Psoriatic arthritis, Retroperitoneal fibrosis, Chronic dermatitis
- Malignancies
- Surgeries: Lymphadenectomy, Surgery of prostate, uterus or cervix, Reconstructive arterial surgeries
- Irradiation
By age:
- At Birth: Prematurity, amniotic bands, Milroy’s disease
- In childhood (Upto 10 years): Meige disease, Turner syndrome
- 10-30 years: Meige disease, rarely infection
- 30-50 years: Primary idiopathic lymphedema (Kinmonth)
- After 50 years: Malignancies
By site:
- Upper limbs: Breast cancer, surgery/irradiation for breast cancer, newborn baby, turner syndrome
- Lower limbs: Congenital lymphedema, parecox, tarda, other secondary causes of lymphedema
Stages of lymphedema:
0 – No edema but presence of lymphatic impairment
1 – Mild edema reversible with appropriate limb position (may PIT)
2 – Moderate edema that is not reversible with limb elevation (Pitting present except in late stage due to fibrosis)
3 – Lymphostatic elephatiasis with trophic skin changes
| Lymphedema | Lipedema |
| Males and females affected | Exclusively females affected |
| Due to failure of lymphatics | Due to abnormal fat deposition |
| No increased bruising | Easy bruising |
| Brawny skin texture | Normal skin texture |
| Involvement of feet | Sparing of feet |
| Kaposi-Stemmer’s sign positive | Kaposi-Stemmer’s sign negative |
Why these edema do no pit on pressure (Mechanism underlying “non-pitting” of certain edema)?
Non-pitting edema usually reflects a condition in which plasma proteins have accumulated in the tissue spaces and coagulated. This usually occurs in high protein edema following increased permeability (infection or trauma) or lymphedema.
Besides, if edema persists for a long duration, it tends to get organized with proliferation of fibroblasts. At this stage, the edema doesn’t pit.
2) Pitting Edema:
Mnemonic: CHILD
- Cardiac failure
- Hypoalbuminemia
- Insufficency (venous), Idiopathic
- Liver disease
- Drugs (Vasodilators, Androgenic)
a. Localized:
- Venous obstruction: Pregnancy, SVC syndrome, IVC syndrome, Varicose veins, Deep vein thrombosis, Prolonged recumbency, Neoplasm (pelvic tumor, lymphoma)
- Infection or inflammation: Cellulitis, Osteomyelitis, Gout
- Local trauma or injury: Bruise, sprain, fracture, insect bite, snake bite, frost bite, burn
b. Generalized:
- Hypoproteinemia:
- Decreased intake: Malnutrition (Kwashiorkor)
- Decreased absorption: Protein losing enteropathy
- Decreased synthesis: Hepatic cirrhosis
- Increased loss via: Skin (Burns), Urine (Nephrotic syndrome), Fecal (Bowel disease)
- Systemic venous hypertension:
- Congestive heart failure
- Pericardial diseases
- Tricuspid valve diseases
- Some special types of generalized edema:
- Cyclic edema of women (varies with menstrual cycle)
- Vasodilators (Minoxidil and Hydralazine causes sodium retention while Nifedipine alters capillary permeability)
- Other drugs: Corticosteroids, Estrogens
- Edema of pregnancy
- Capillary leak syndrome (In critically ill patients who are septic)
The 4 common causes of Anasarca are:
- Congestive cardiac failure
- Nephrotic syndrome
- Liver cirrhosis
- Malnutrition
Why there is pitting of edema?
Pitting edema occurs when the accumulation of interstitial fluid exceeds the absorptive capacity of the tissue gel. The tissue water becomes mobile and can be translocated with the pressure exerted by a finger.

B. Ascites in Liver cirrhosis
C. Pitting pedal edema in Congestive heart failure
D. Unilateral edema of lymphedema
| Cardiac edema | Hepatic edema | Renal edema | |
| Dependent edema | ++++ | +++ | ++ |
| Facial edema | – | – | + |
| Ascites | + | ++++ | + |
| Evolution | Legs → Face → Ascites | Ascites → Legs → Face | Face → Legs → Ascites |
| Dyspnea | Precedes edema | Follows ascites | |
| Clinical features | Of cardiac failure Raised JVP | Hepatomegaly may be present Stigmata of Chronic liver diseases | Pale and waxy look |
| Hypoalbuminemia | – | ++ | ++++ |
| Proteinuria | 0-trace | 0-trace | ++++ |
Edema with sudden onset (<72 hours): DVT, Cellulitis, Trauma, Acute nephritis, Allergic reactions
Dependent edema:
- Improves with limb elevation (Venous insufficiency)
- Doesn’t improve with limb elevation (Malnutrition, Cirrhosis, CHF, Nephrotic syndrome)
Asymmetrical/Unilateral edema
- Deep vein thrombosis (DVT)
- Postphlebitic syndrome
- Baker cyst rupture
- Gastrocnemius rupture
- Cellulitis
- Trauma
- Insect stings
- Venous insufficiency
- Varicosities
- Lymphatic obstructions
Most cases of unilateral edema must be considered for venous doppler assessment for presence of DVT regardless of whether it is associated with pain.
Causes of Edema in Newborns:
A) Generalized:
- Hemolytic disease of newborn
- Congestive cardiac failure
- Cold injury
- Electrolyte imbalance (Overhydration, Hypernatremia, Hypokalemia)
- Nutritional edema (Anemia with hypoproteinemia, Vitamin E deficiency)
- Renal edema (Congenital nephrosis)
- Maternal diabetes
B) Localized:
- Head: Caput succedaneum (not to be confused with cephalhematoma)
- Face: Excessive crying, conjunctivitis, drug sensitivity
- Limbs: Arm presentation, cold, Milroy’s disease, Turner syndrome
- Genitalia: Physiological, Allergic, Insect bite, Cellulitis
- Abdominal wall: Peritonitis, Necrotizing enterocolitis, Appendicitis
General physical examination in Patient with Edema
- Built and nourishment: Poor in nutritional deficiency
- Pallor: Cardiac or Gastrointestinal cause
- Icterus: Hepatic cirrhosis
- Cyanosis and clubbing: Cardiac edema
- Lymphadenopathy: Filariasis
Clinical Tips:
- Minimally 10-15% increase in body weight is necessary for demonstrable pitting edema.
- Most reliable index of progression of treatment of edema is daily alteration of body weight.
- Bilateral pitting edema can occur in hyperthyroidism as a result of heart failure. However, cases with unilateral pitting edema have also been seen, the mechanism of which is not clearly understood but is responsive to the treatment.
- Complications of peripheral edema include cellulitis, venous thrombosis, impaired vision (periorbital edema), pain
- Complications of ascites include impaired intestinal absorption, esophageal reflux, dyspnea, umbilical and inguinal hernias, spontaneous bacterial peritonitis
- General measures for treatment of edema include management of primary disease, bed rest, Na+ restriction and Diuretic administration.

This is the best summary of edema I have found on the web. Thanks for the high quality information.
Very nyc
Amazing learning aid. Edema well explained
Its really best info about the edema that I got on internet thank u so much for this
Very helping best info about enema
very important
Best ever read on edema .
thanks for the info, can the reference be added in this?
I conquer with the above
Thanks for this comprehensive article.
Thanks for your bank of information
its help me so the best info of pitting edema
This post provides a clear and concise overview of the physical examination of edema. I especially appreciated the step-by-step approach to assessing the different types of edema. It’s helpful to have the clinical pearls highlighted, as they really clarify the key points. Looking forward to more in-depth discussions on related topics!