Synonyms: Jaundice
Definition of Icterus
Icterus is the yellowish discoloration of skin and mucous membrane and body fluids (CSF, joint fluid, cysts) evident as a result of hyperbilirubinemia with subsequent deposition of bile pigments in tissue which is rich in elastin. The Greeks claimed the sight of an oriole would cure jaundice, thus they got a name i.e. icterus (Greek- Ikteros). Usually, jaundice becomes apparent clinically as icterus at serum bilirubin levels exceeding 2-3 mg/dl in older children and adults and at more than 5 mg/dl in neonates.
Icterus and Hyperbilirubinemia
Icterus is a sign that the hyperbilirubinemia exists. The degree of jaundice is directly related to the level of serum bilirubin and the amount of bilirubin deposited in the extravascular tissues.
Sites to look for Icterus
Pre-requisite: Preferably natural daylight (may not be detected in artificial light). Use transcutaneous bilirubinometer in infants if natural light is not available.
Sites:
- Upper bulbar conjunctiva (scleral icterus is a misnomer!!)
- Palate
- Under surface of tongue
- Palms and soles
- General skin surface
Why disappearance of icterus often lags behind the resolution of elevated serum bilirubin concentrations? This is because conjugated bilirubin binds to tissue protein and is only slowly degraded.
Icteric coloring is hardly or not at all evident on paralyzed body parts suggesting that the bilirubin concentration is dependent also upon normal nerve function.
As a rule, jaundice is not detected in the region of edema.
It is important not to misinterpret normal brownish color of bulbar conjunctiva in dark-skinned individuals resulting from sunlight exposure. If in confusion, inspect the inferior conjunctival recess which should be entirely white in anicteric individuals.
Assessment of icterus in Upper bulbar conjunctiva
How (technique)? Retract both the upper eyelids simultaneously upward and ask the patient to look downwards.
Why (reason)? Scleral icterus is a term commonly used in the textbooks; however, from a histopathologic perspective, it is a misnomer. Bilirubin has a high affinity for elastin which is an abundant protein in the conjunctivae as well as the superficial, fibrovascular episclerae, but not the sclerae proper. One actually is observing icterus of the bulbar conjunctiva against the white background provided by sclera. Hence, authors have recommended for the use of term “conjunctival icterus” instead of “scleral icterus”. Due to the same reason, i.e. high elastin content – conjunctival icterus is often the first sign of hyperbilirubinemia.
Assessment of icterus in Neonates
How? Press the skin against bony surface for 5 seconds to blanch the skin and observe the skin color. Gently press over forehead or chest.

Why? To press out the normal pink or brown color so that the yellowish blanching can be noted.
 Kramer’s rule: Kramer recognised the cephalocaudal progression of jaundice with increasing total serum bilirubin levels and divided the baby into 5 zones, with an estimated total serum bilirubin level measurement associated with each zone.
Kramer’s rule: Kramer recognised the cephalocaudal progression of jaundice with increasing total serum bilirubin levels and divided the baby into 5 zones, with an estimated total serum bilirubin level measurement associated with each zone.
- Grade 1 (Face and neck only): 10 mg/dl
- Grade 2 (Upper trunk upto umbilicus): 15 mg/dl
- Grade 3 (Lower trunk below umbilicus to knee): 20 mg/dl
- Grade 4 (Arms and lower legs below knee): 25 mg/dl
- Grade 5 (Palms and soles): >25 mg/dl
Shades/Colors of Jaundice
- Reddish shade (Rubin jaundice): Hepatitis
- Lemon yellow with a reddish hue (Flavin jaundice): Hemolysis
- Greenish yellow (Verdin jaundice): Obstructive jaundice
- Grayish or blackish green (Melas jaundice): Prolonged obstructive jaundice
Differential diagnosis of Jaundice
Jaundice is the only condition causing yellow sclerae. Other causes of yellow discoloration of the skin, but where the sclera remain normal are:
- Carotenaemia/Xanthoderma: Usually due to excessive consumption of carotene – carrots or hypothyroidism
- Lycopenaemia: Excessive consumption of tomatoes
- Acriflavine
- Fluorescein
- Picric acid ingestion
- Drugs: Quinarcine (Atabrine, Mepacrine), Busulfan
Tips for aid of Diagnosis
Look for other signs that helps in diagnosis.
General examination
Pallor: Hemolysis, Chronic liver disease or malignancy
Pedal edema: Chronic liver disease, IVC obstruction, Severe anemia with volume overload, hypoproteinemia due to nutritional deficiency or malabsorption
Lymphadenopathy:
- Generalized: Lymphoma
- Supracalvicular (Virchow’s) node: Abdominal malignancy
Evidence of pneumonia: Liver may be involved in pneumococcal pneumonia
Evidence of congestive heart failure: Chronic passive congestion of liver
Kayer-Fleischer ring and extrapyramidal neurological features: Wilson’s disease
Xanthomas: Primary biliary cirrhosis
Migratory thrombophlebitis: Carcinoma body of pancreas (Trosseau syndrome)
Abdominal Examination
Dilated abdominal veins: Portal hypertension i.e. Caput medusae (direction of flow in infraumbilical veins is towards leg), IVC obstruction (direction of flow in infraumbilical veins is towards head)
Murphy’s sign: Acute cholecystitis, Ascending cholangitis
Ascites: Cirrhosis, Malignancy, Infections (TB, malignancy, SBP, Acute pancreatitis)
Liver:
- Shrunken: Cirrhosis, Fulminant hepatic failure
- Hard liver: Malignancy
- Massive hepatomegaly (>10 cm below costal margins): Malignancy, Congestive liver, Alcoholic liver disease, Primary biliary cirrhosis, Prolonged extrahepatic cholestasis, Infiltrative disease of liver (amyloidosis, myelofibrosis), Chronic myeloid leukemia (CML)
- Tender liver: Congestion, Infection, Bile stasis
- Bruit: Acute alcoholic hepatitis, Hepatocellular carcinoma, Hepatic artery aneurysm, Hepatic arterio-venous fistula
- Friction rub (friction between roughened peritoneal surfaces): Neoplasm, Liver infarction, Liver abscess, Hematoma around puncture site (recent liver biopsy)
- Venous hum (increased blood flow in umbilical and paraumbilical veins in falciform ligament): Intrahepatic portal obstruction
Palpable non-tender gallbladder: Periampullary carcinoma (Courvoisier’s law)
Peripheral stigmata of Chronic liver disease
- Alopecia
- Eye signs mimicking hyperthyroidism
- Parotid enlargement
- Fetor hepaticus
- Palmar erythema
- Dupuytren contracture
- Leukonychia
- Paucity of axillary and pubic hair
- Spider angiomata (Usually found in SVC distribution): >12 in number indicate portal hypertension
- Gynecomastia
- Testicular atrophy
Triad of parotid enlargement, dupuytren contracture and gynecomastia suggest chronic alcoholism.
Signs suggestive of decompensated hepatic failure
- Ascites
- Oliguric hepatic failure
- Hepatic encephalopathy
- Altered behaviour
- Fetor hepaticus
- Asterexis
Source: Schiff’s Diseases of the Liver
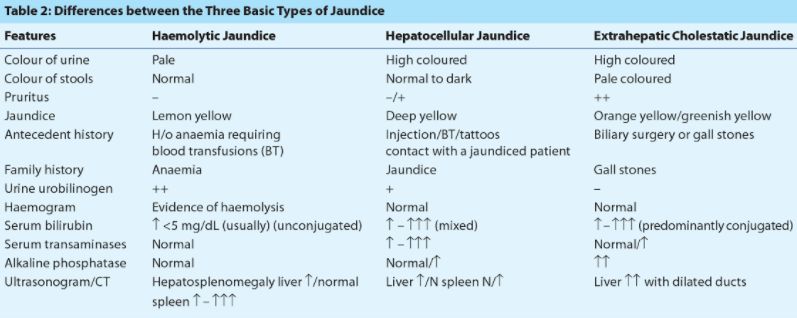
Differentiating 3 broad causes of Icterus or Jaundice
Difference between Icterus and Jaundice
The text below is directly quoted from 1000 questions and answers from Kumar and Clark’s Clinical Medicine.
“Are ‘jaundice’ and ‘icterus’ one and the same? I was taught that icterus is yellowing of the sclera, while jaundice is yellowing of the skin and the mucous membranes. As a result, carotenaemia can produce jaundice but not icterus: is this so? I would be grateful if you would clarify this for me.”
The question has been answered –
‘Jaundice’ and ‘icterus’ are the same. In the main, people use the word ‘jaundice’ most of the time. ‘Anicteric’ is sometimes used to describe a person who is not jaundiced.

Grades of icterus in adults