Synonyms: Morbus coeruleus, Blue disease
Definition of Cyanosis
Cyanosis is the bluish discoloration of the skin, mucous membrane and nail bed usually owing to atleast 5 gm/dl of reduced hemoglobin/deoxyhemoglobin or abnormal hemoglobin derivatives (eg. methemoglobin, sulfhemoglobin, etc.) circulating within the superficial dermal capillaries and subpapillary venous plexus (not, as commonly taught, the deeper arteries and veins). Normally, cyanosis is evident when the Oxygen saturation (SaO2) is < 85%. However, in a neonate cyanosis is observed when the oxygen saturation is < 70% (at lower oxygen saturation due to higher hematocrit level in neonates).
Types of Cyanosis and Difference between them
| Features | Central cyanosis | Peripheral cyanosis |
| Mechanism | Inadequate oxygenation of systemic arterial blood (Hypoxic hypoxia) | Sluggish peripheral circulation (Stagnant hypoxia) |
| Sites to look | Tongue and oral mucosa – Tongue, inner aspect of lips, gum, soft palate, buccal mucosa, lower palpebral conjunctiva and sites of peripheral cyanosis | Acral – Nose tip, ear lobules, outer aspect of lips, finger tips, nail bed, extremities |
| Associations | Clubbing Polycythemia | |
| Extremities | Warm | Cold |
| Warming extremities | No change | Disappears |
| Oxygen inhalation | Slight improvement | No change |
| ABG PaO2 | Low <85% | Normal 85-100% |
| Pulse volume | May be high | Usually low |
| Dyspnea | Often present | Usually absent |
Cyanosis and Hemoglobin level
Cyanosis results from atleast 5 gm/dl of absolute concentration of reduced hemoglobin. The increased amount of deoxygenated hemoglobin is due to either an increased amount of venous admixture (due to vasodilatory effects on the venous plexi) or by reduced arterial oxygen tension in the capillaries. Atleast 15-20 gm/L of deoxygenated hemoglobin concentration is required in artery to reach 50 gm/L in the tissue microcirculation needed to produce cyanosis.
It is the absolute, not relative, quantity of deoxygenated hemoglobin that matters; this means that for a given patient, the level of SaO2 at which cyanosis becomes apparent depends on their total hemoglobin concentration. Because of this, severely anemic patients with marked arterial desaturation might not be cyanosed, yet polycythemic patients develop obvious cyanosis at much higher SaO2.
Method of Cyanosis Examination
1. Adequate lighting is needed (cyanosis is better detected in fluorescent light than daylight). The detection is said to be more difficult if the patient’s bed is surrounded by cheerful pink curtains.
2. Cyanosis is best appreciated in areas of the body where the overlying epidermis is thin, melanotic pigment is minimal and the blood vessel supply abundant, such as lips, malar prominences (nose and cheeks), ears, and oral mucous membranes (buccal, sublingual).
3. Lewis test (Central vs Peripheral cyanosis): After massaging the ear lobules (until there is capillary pulse), the ear lobules remain cyanotic in central cyanosis and the blue discoloration disappears in peripheral cyanosis.
4. Hyperoxia test (Cardiac vs Pulmonary cyanosis): After placing an infant on 100% oxygen for 10 minutes, a repeat ABG is done and if PaO2 is < 150 mmHg then the cause is cardiac and if the PaO2 improves to > 200 mmHg, the cause is respiratory. The test is not very accurate.
5. Rapid test to detect enterogenous cyanosis: Place 1 drop of blood on a swab and compare color with another drop of met-Hb free blood after 1 minute and a brown coloration that doesn’t disappear when air is mixed suggest metHb > 20 gm/dl.
Causes and Classification of cyanosis
A) Central cyanosis
1. Cardiac (Admixture cyanosis):
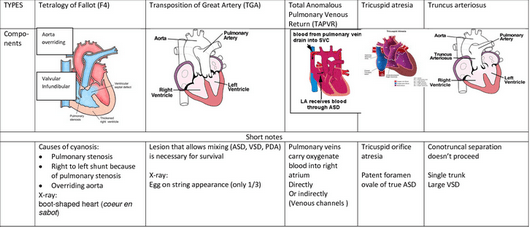
- Congenital cyanotic heart diseases (Remember 6 ‘T’s)
- Transposition of great arteries
- Tetralogy of Fallot
- Truncus arteriosus
- Tricuspid valve abnormalities
- Total Anomalous Pulmonary Venous Return (TAPVR)
- Tons of others: Pulmonary atresia, Hypoplastic left heart, Coarctation of aorta (Preductal type), Eisenmenger’s syndrome
- Acute pulmonary edema (due to left sided heart failure)
Eisenmenger’s syndrome (Cyanosis tardive): Conversion of acyanotic heart disease (left to right shunt) to cyanotic heart disease (right to left shunt) due to pulmonary hypertension.
2. Pulmonary (Anoxemic cyanosis):
- Acute severe asthma
- COPD, Cor pulmonale, Respiratory failure, Respiratory depression
- Lobar pneumonia
- Fibrosing alveolitis
- Tension pneumothorax
- Acute laryngeal edema – Acute epiglottitis, Croup
- Acute pulmonary embolism
- Pulmonary arterio-venous fistula – congenital or acquired due to hepatic cirrhosis
3. High altitude (due to low partial pressure of oxygen)
4. Polycythemia
5. Enterogenous or Pigment cyanosis (Replacement cyanosis): It is a special type of central cyanosis due to presence of excessive sulfhemoglobin (>0.5 gm/dl) or methemoglobin (>1.5 gm/dl) in blood. Diagnosis is confirmed by spectroscopic examination of blood. It’s causes are:
- Methemoglobinemia – Bluish (iron is in the ferric form instead of ferrous form):
- Congenital: Hereditary hemoglobin M disease, Deficiency of metHb reductase I, G6PD deficiency
- Acquired: Medications (Sulfonamides, Phenacetin, Nitro- compunds like nitroglycerin, sodium nitroprusside, amylnitrate, etc.), Nitrite in well water
- Sulfhemoglobinemia – Grayish: Sulfonamides, Phenacetin
6. Carboxyhemoglobinemia (not true cyanosis, “chocolate cyanosis”)
3 common causes of central cyanosis are cardiac disease, pulmonary disease and central nervous system (CNS) depression. The most common cause of central cyanosis in the adult is pulmonary disease, especially chronic obstructive airway disease.
B) Peripheral cyanosis
- Low cardiac output: Congestive heart failure
- Local vasoconstriction: Cold, Frost bite, Raynaud’s phenomenon, Shock
- Arterial obstruction: Peripheral vascular diseases (Atherosclerosis, Buerger’s disease, Atheroembolism)
- Venous obstruction: SVC syndrome
- Hyperviscosity syndrome: Multiple myeloma, polycythemia, macroglobulinemia
- Others: Cryoglobulinemia, Mitral stenosis
All causes of central cyanosis can cause peripheral cyanosis.
C) Mixed cyanosis (Central + Peripheral)
- Cardiogenic shock with pulmonary edema
- Corpulmonale
- Polycythemia (rarely)
Mnemonics
Peripheral cyanosis: COLD
- C: Cold
- O: Obstruction
- L: LVF and shock
- D: Decreased cardiac output
Central cyanosis: CLAMPS
- C: Congenital heart disease
- L: Lung disease
- A: Altitude
- M: Methaemoglobinaemia, sulphaemoglobinaemia
- P: Polycythemia
- S: Shock
Differential diagnosis of cyanosis in Newborns
- Pulmonary: Respiratory distress syndrome, Sepsis, Meconium aspiration pneumonia, Diaphragmatic hernia, Transient tachypnea of newborn, Pleural effusion
- Cardiovascular: 6 ‘T’s of cyanotic congenital heart disease
- CNS: Maternal sedative drugs, Asphyxia, Intracranial hemorrhage, Neuromuscular disease, Seizure
- Hematologic: Acute or chronic blood loss, Cyanosis, Methemoglobinemia
- Metabolic: Hypoglycemia, Adrenogenital syndrome
- Anatomic: Choanal atresia, Malacia of larynx/trachea /bronchus
Onset of cyanosis in newborns:
- At birth: Probably respiratory in origin
- After a few hours of birth: May be cardiac (Transposition of great arteries likely)
- After 24 hours: Most ductal-dependent lesions present at this time as the PDA starts closing, cyanosis becomes apparent. Likely lesions are pulmonary atresia, critical pulmonary stenosis, tetralogy of fallot
Why polycythemia can be attributed as the cause of both central and peripheral cyanosis?
- It causes peripheral cyanosis due to hyperviscosity of blood.
- Primary polycythemia (polycythemia rubra vera) can cause central cyanosis resulting from pulmonary hypertension due to increased viscosity of the blood which interferes with pulmonary perfusion.
- Seconday polycythemia arising from the cause of hypoxia are often also the causes of central cyanosis.
Differential diagnosis for bluish discoloration
1. Cyanosis
2. Pseudocyanosis (Bluish tinge of skin or mucous membrane in the absence of hypoxemia or peripheral vasoconstriction): Pseudocyanosis can mimic peripheral cyanosis, however, there is no response to attempted “blanching” of the skin by applying pressure. It can be caused by –
- Metals: Silver (Argyrosis), Lead
- Medications: Amiodarone, Phenothiazines (Chlorpromazine)
3. Osteogenesis imperfecta (Only the sclera is blue)
Some other types of cyanosis
1) Differential cyanosis: Often cyanosis is associated with clubbing
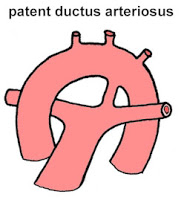
Cyanosis only in lower limbs: PDA with reversal of shunt (Eisenmenger PDA or reverse PDA)
Mechanism: Desaturated blood from the ductus enters the aorta distal to the left subclavian artery, sparing the brachiocephalic circulation. The oral mucosa and tongue receive saturated blood and are not cyanotic.
Cyanosis only in upper limbs (reverse differential cyanosis): Coarctation of aorta (ductal type) with transposition of great arteries
Mechanism: Desaturated blood enters the ascending aorta from the right ventricle and the saturated left ventricular blood enters the descending aorta via the patent ductus.
Cyanosis in left upper limb and both lower limbs: PDA with reversal of shunt and preductal coarctation of aorta
Mechanism: Ductus enters the aorta distal to the coarctation and perfuses the lower limbs via descending aorta and left upper limb via left subclavian artery with desaturated blood.
Intermmitent cyanosis: Ebstein’s anomaly
Cyclical cyanosis: Bilateral choanal atresia
2) Orthocyanosis:
- Development of cyanosis only in upright position due to hypoxia occuring in erect posture
- Seen in: Pulmonary arterio-venous malformation
Mechanism: As shown in the figure above, in supine position the AV malformation comes to lie somewhere near zone 2 and near zone 3 in upright position where hydrostatic pressure is higher but resistance is lower. This leads to an increased amount of shunting of blood manifesting as cyanosis.
3) Acrocyanosis:
- Persistent blue or cyanotic discoloration of the extremities, most commonly occurring in the hands, although it also occurs in the feet and distal parts of face.
- Vasospasms in the cutaneous arteries and arterioles produce cyanotic discoloration, while compensatory dilatation in the postcapillary venules causes sweating.
- May be primary (idiopathic) or secondary (eg. anorexia nervosa, antiphospholipid antibody syndrome, cryoglobulinemia, tricyclic antidepressants, etc.)
- Usually normal in newborns
Absence of Cyanosis when Expected
Despite of sufficient reduced hemoglobin, cyanosis may be absent in some conditions:
- Severe anemia: When the hemoglobin concentration falls < 5 gm/dl, relative amount of reduced hemoglobin may be large but the absolute amount of reduced hemoglobin is less. Always remember that not the relative but absolute quantity of reduced hemoglobin is responsible for producing cyanosis. (Also, note that the patients with polycythemia can develop cyanosis more easily for the same reason)
- Carbon monoxide poisoning: Carboxyhemoglobin prevents reduction of oxyhemoglobin and has cherry red color
Aids in the diagnosis of cause of cyanosis
1) History: Onset (If since birth – probably congenital heart disease); Drugs (Enterogenous cyanosis)
2) Examination: Central vs Peripheral cyanosis; Clubbing with cyanosis (Congenital heart diseases, pulmonary abscess, pulmonary AV malformation)
Note: Peripheral cyanosis or acutely developing central cyanosis is not associated with clubbing.