A 15 year girl started complaining of strange feelings 3 weeks back. She started behaving weirdly and complained her mother that she could hear inanimate objects talking to her- like bangles, rings, glasses. She rapidly had a deterioration with change in personality. She starting acting bizarre and doing abnormal things.
Soon she started seeing things that were not there. She looked at empty streets and talked to people who were not there. She had episodes of stiffening of body, losing orientation and cognition and blast of irrelevant and incoherent speeches lasting for hours. She used to attain weird posture for hours.
There was no history of documented fever, headache, vomiting, frothing from mouth or stool and urine incontinence.There was no history of toxic ingestion or exposure, no history of recent illness preceding the incident or head trauma.
The symptoms were intermittent with some improvement in between.
Appetite was decreased. Urine /Stool were normal. There was no significant weight loss.
She was taken to a local hospital, where investigations were carried out:
- Her CBC ,Urine, Renal functions, Liver functions were Normal
- CT Scan of the head was normal.
She was started on Anti-psychotic drugs for Schizophrenia – Olanzapine and Haloperidol. After a week of medication , her symptoms deteriorated. Her cognition deteriorated and her body started stiffening episodically. There was no seizure in the hospital. Parents, dissatisfied with the treatment took her home against medical advice.
Next:
- She was projected to Traditional healer- Dhami , a form of exorcism but with no help.
- She had fever of high grade, rigid stiffening limbs episodically and GCS deteriorated, thus was rush to our ER room.
At Presentation:
General examination: She was delirious, disoriented, restless – tossing in bed, limbs were flexed and stiff. There was no obvious respiratory distress. Her general examination revealed no pallor, icterus, edema, lymphadenopathy, cyanosis . She was mildly dehydrated.
Vitals: Her Blood Pressure was 150/100 mmHg, Pulse rate 140/min, Temperature 103F, Respiratory rate 34/min with mild Subcostal recession, SpO2 92% without Oxygen.
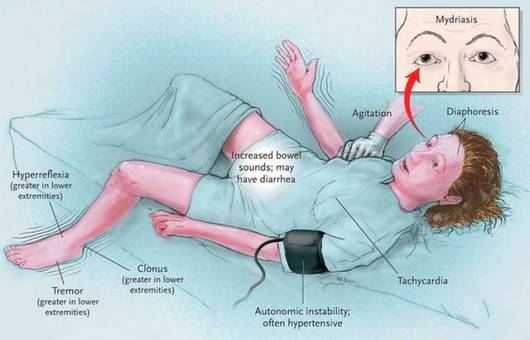
Neurological examination revealed: Generalized increase in tone, with exaggerated jerks and clonus. Stiffness was catatonic type rather than dysonic. Other examination of CNS that could be assessed were normal.
Chest examination was normal.
Per abdomen examination: there was mild distension,flanks full, no organomegaly, Bowel sounds were present. SD+
Reviewing the history:
- It revealed that that she had relationship issues which was causing stress for a month. She had fear that family members would punish her.
- She had left her medication 5 days back and gone to traditional healer for treatment.
Diagnostic clues:
- Change in behavior
- Irrelevant talks
- Auditory hallucinations
- Visual hallucinations
- Muscle stiffness
- Delayed onset fever
We had some idea about the diagnosis by now.
1. Neuroleptic Malignant Syndrome: history of drug intake for schizophrenia , high fever, muscle rigidity , deterioration of GCS. Point against it was- she was already off the anti-psychotic medications
2. Catatonic Schizophrenia: She attained a catatonic posture, had hallucinations -auditory and visual, along with bizarre behaviour. CT scan was normal.
3. Conversion disorder: Adolescent female, history of precipitating stress, sudden onset bizzare behavious, stiffenning, tossing with improvement in between.
4. CNS tumors and Menigoencephalitis: frontal or temporal tumors might cause change in personality and similar manifestation but CT scan was normal. encephalitis needed to be ruled out.
5. Endocrinopathy: no features matching endocrine disorders.
6. Connective tissue: SLE – Psychosis- CNS manifestation, ? ascites-serositis, fever but there was no history of joint pain, rashes or other symptoms.
7. Wilson’s Disease: rare but neurological manifestation of Wilsons sought to be rules out.
We sent following Investiagations:
- CBC: showed Leukocytosis.
- RFT: Urea was high- 120 mg/dl , Creatinine was normal
- Na+: 155 K+- 4.6
- SGOT: 2 fold of higher normal value.
- Serum CPK: was raised 2200.
- USG abdomen: revealed mild ascites. No organomegaly.
- Urine pregnancy test: was negative.
- ANA was sent: Negative
- CSF: was normal.
- Urine Myoglobulin was planned, Toxic screening for drugs.
[hr]
ROUND DISCUSSIONS
Neuroleptic malignant syndrome is the rarest and the most serious of the neuroleptic induced movement disorders. Potent neuroleptics are more frequently associated with NMS however the atypical antipsychotic drugs are known cause of NMS. (1) 90% of those who develop NMS do so with in 10 days of starting therapy.(3)
Presentation of olanzapine-induced NMS varies widely. Onset from within 8 hours of starting olanzapine to after 2½ years of stable olanzapine dosing has been reported. Our patient had history of starting olanzapine 9 days back which she stopped 5 days back. Some cases have featured a typical NMS presentation.(2)
Proposed Pathophysiology for Neuroleptic Malignant Syndrome:
Diagnostic Criteria (3):
| Diagnostic Criteria | Priority Score |
| Exposure to dopamine antagonist or dopamine agonist withdrawal within past 72 h | 20 |
| Hyperthermia (>100.4 º F or >38 º C on at least 2 occasions, measured orally) | 18 |
| Rigidity | 17 |
| Mental status alteration (reduced of fluctuating level of consciousness) | 13 |
| Creatinine kinase elevation (at least 4 times the upper limit of normal) | 10 |
Sympathetic nervous system lability, defined as at least 2 of the following:
| 10 |
| Hypermetabolism defined as heart rate increase (≥ 25% above baseline) AND respiratory rate increase (≥ 50% above baseline) | 5 |
| Negative work-up for infections, toxic, metabolic or neurologic causes | 7 |
| Total | 100 |
In Our patient:
She had history of exposure to Drug – 20 , Hyperthermia – 18, Rigidity – 17, Mental status alteration – 13, Elevated CPK -10, High BP and diaphoresis – 10, Tachypnea and tachycardia – 5. So, the total was 93/100 which was in favor of diagnosis of Neuroleptic Malignant Syndrome.
Sometimes, atypical presentations can occur with presence of these features:
- Extremely elevated serum Na+
- Absence of rigidity
- Normal CPK
- Generalized tonic-clonic seizures preceding NMS onset
- Anterograde amnesia
- Deficits in learning verbal information.
Have we missed something? We rechecked for differential diagnosis:
1. CNS infection ( meningitis, encephalitis): Unlikely; CSF normal
2. Systemic infections (eg, pneumonia, sepsis): Still possible; Leukocytosis with X ray infiltrates
3. Seizures: Unlikely
4. Acute hydrocephalus: CT normal, no features of raised ICP
5. Acute spinal cord injury: no h/o fall or trauma
6. Heat stroke (neuroleptics predispose to heat stroke by impairing thermoregulation): no exposure to adverse conditions
7. Acute dystonia: patient had rigidity rather than dystonia
8. Tetanus: Immunized, no risk factors, symptoms were improving in between, no opisthotonus posture
9. CNS vasculitis: Less likely
10. Thyrotoxicosis: no features of hyperthyroidism
11. Pheochromocytoma: USG normal; still urine catacholamines and further investigations were planned in this line.
12. Drug abuse: no exposure
One Prominent Differential that stood before us was:
Fatal Catatonia: The fatal catatonia is abrupt on set hyperthermia and rigidity leading to death usually in psychiatric patients with unclear realtion with antipsychotics. If there are prodormal symptoms before onset of rigidity, its more likely NMS than catatonia. It has been suspected to be associated with viral infection of Brain-particularly Limbic systems. Enough Literatures were not available on this consition.
Management:
- The patient was given antipyretics.
- IV fluids and oxygen was started.
- ECG and Vitals monitoring under Wall monitor.
- Arrangement for ICU care.
- Inj Lorazepam was started.
- Other treatment include: Hydration and alkalinization for rhabdomyolysis and Electroconvulsive therapy (ECT)
[hr]
References:
Olanzapine induced neuroleptic malignant syndrome–a case review. Kogoj A, Velikonja I.Hum Psychopharmacol. 2003 Jun;18(4):301-9.
Neuroleptic malignant syndrome-http://www.nmsis.org/pages/nms_guarddown2.asp

MD Pediatrics and Fellowship Neonatology, he chooses to stay anonymous. He often writes his views online as well as share few important topics for medical students, doctors and specially parents. He does research in pediatrics.