Before proceeding to this topic, it would be wise to go through the topics listed below:
Tile/AO Classification
Tile classification divides pelvic fractures into three basic types according to stability based on the integrity of the posterior sacroiliac complex. Here is a mnemonic that can be used to remember tile classification.
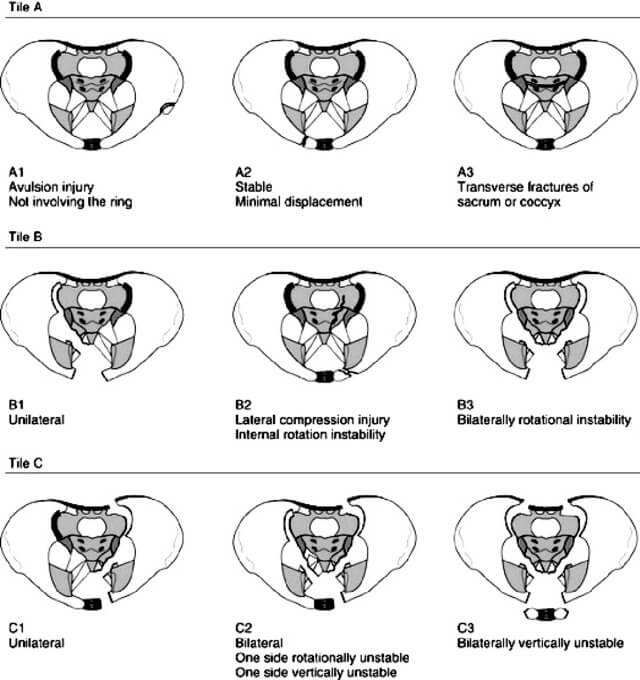
Tile A: Anterior arch only (Posterior arch intact)
- Avulsion injury (3 spines – ASIS, AIIS or pubic spine)
- Anterior arch or Ala of ilium (Iliac wing)
- Across (transverse fracture) the Ala of sacrum or coccyx
Tile B: Borderline stable (Posterior arch – incomplete disruption)
- Book (Open): External rotation – Pubic diastasis > 2.5 cm +/- SI joint widening
- Book (Closed): Internal rotation – Lateral compression injury
- Book – Bilateral B injuries
Type C: Completely unstable (Complete disruption of posterior arch)
- One side C
- One side B, One side C
- Both side C
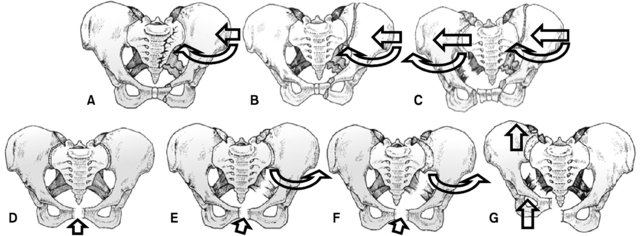
Young Burgess Classification
It is based on injury mechanism.
| Type | Fracture characteristics | Ligaments disrupted | Treatment | Key concepts |
| Anterior-Posterior Compression (APC) | ||||
| APC1 | Pubic diastasis <2.5 cm | Stretched anterior SI, sacrospinous, sacrotuberous ligaments | Nonsurgical Protected WB | Tile A |
| APC2 | Pubic diastasis >2.5 cm with widening of anterior SI joint | Disrupted anterior SI, sacrospinous, sacrotuberous ligaments | ORIF anterior pelvis (symphyseal plate) | Tile B |
| APC3 | Pubic diastasis with widening of both anterior and posterior SI joint | + Posterior SI ligament disruption | Urgent pelvic sheet or binder to stabilize the pelvis ORIF of anterior pelvis with posterior fixation (SI screws or plate/screws) | Tile C Highest rate of blood loss and GU injury |
| Lateral compression (LC) | ||||
| LC1 | Transverse pubic rami fractures Sacral impaction fracture on side of impact | Nonsurgical Proteced WB (Complete, comminuted sacral component) WBAT (Simple, incomplete sacral fractures) | Tile A | |
| LC2 | Transverse public rami fractures Crescent fracture of ilium on side of impact | Variable disruption of posterior ligamentous structures | ORIF of ilium | Tile B |
| LC3 | LC1/2 + APC on other side (Windswept pelvis) | ORIF anterior and posterior pelvis | Tile C Windswept pelvis Associated with head, chest and abdominal trauma Most common cause of death is closed head injury | |
| Vertical Shear (VS) | ||||
| VS | Vertical displacement of hemipelvis (malgaigne fracture) | SI ligaments, sacrotuberous ligament, sacrospinous ligaments, symphyseal ligament | Traction initially ORIF anterior and posterior pelvis | Tile C Associated with intrapelvic hemorrhage and neurologic injury |
| CM | Combined |
WSES (World Society of Emergency Surgery) Classification
It uses Young-Burgess classification and hemodynamic stability to classify and guide pelvic fracture management. Hemodynamic stability is the condition in which the patient achieve a constant or an amelioration of blood pressure after fluids with a blood pressure >90 mmHg and heart rate <100 bpm.
Hemodynamic instability:
- Admission systolic blood pressure <90 mmHg, or > 90 mmHg but requiring bolus infusions/transfusions and/or vasopressor drugs OR
- Admission base deficit (BD) >6 mmol/l OR
- Shock index (Pulse rate/Systolic BP) > 1 OR
- Transfusion requirement of at least 4–6 Units of packed red blood cells within the first 24 h
| WSES grade | Young-Burgess classification | Hemodynamic | Mechanic | CT-scan | First-line Treatment | |
| MINOR | I | APC I – LC I | Stable | Stable | Yes | Conservative |
| MODERATE | II | LC II/III – APC II/III | Stable | Unstable | Yes | Pelvic Binder in the field ± Angioembolization (if blush at CT-scan) Operative – Anterior External Fixation |
| III | VS – CM | Stable | Unstable | Yes | Pelvic Binder in the field ± Angioembolization (if blush at CT-scan) Operative – C-Clamp | |
| SEVERE | IV | Any | Unstable | Any | No | Pelvic Binder in the field Preperitoneal Pelvic Packing ± Mechanical fixation ± REBOA (Resuscitative Endo-aortic balloon) ± Angioembolization |
Further reading: Coccolini, F., Stahel, P.F., Montori, G. et al. Pelvic trauma: WSES classification and guidelines. World J Emerg Surg 12, 5 (2017). https://doi.org/10.1186/s13017-017-0117-6
Faringer classification for Open pelvic fractures
Denis classification for Sacral fractures
| Denis type | Fracture description | Neurologic injury | Remarks |
| Zone 1 | Lateral to foramina (Alar) | L5 root; 5% | Commonest (50%) |
| Zone 2 | Through foramina (Transforaminal) | L5/S1/S2 root; 30% | Stable vs Unstable |
| Zone 3 | Medial to foramina (Spinal canal) | 60% | Bowel, bladder & sexual dysfunction Includes “H” or “U” type fractures |
Letournel Judet classification for Acetabulum fractures
Associated patterns: Posterior column/posterior wall, Transverse with posterior wall, T type, Anterior column/posterior hemitransverse, Both column
Indications for surgery:
- >2 mm displacement
- Posterior wall fracture >/= 20% of wall (20-40% and unstable under stress EUA)
- Roof arc angle <45 degrees
- Incongruity of hip joint (absence of secondary congruence)
- Incarcerated fragments/loose bodies
- Marginal impaction
- Irreducible fracture-dislocations
Roof arc angle of Matta: It is the estimation of amount of weight bearing dome (WBD) involved. It is the angle measured between a line from dome to geometric center of femoral head and another line from fracture to the geometric center in following 3 views:
a. AP view: Medial roof arc angle
b. Obturator oblique view: Anterior roof arc angle
c. Iliac oblique view: Posterior roof arc angle
Roof arc angle <45 degrees in any view (Matta et.al.) signifies unstable fracture requiring fixation.
Roof arc angle <45 degrees in AP, <25 degrees in obturator oblique and <70 degrees in iliac oblique view (Varhas et.al.) signifies unstable fracture requiring fixation.
It is not applicable to isolated posterior wall fracture and both column fractures.
Important points on management of pelvic ring fractures
1. Pelvic binder/sheet: Applied at the level of greater trochanter (GT)
2. Anterior stabilization with external fixator (Ganz): Decreases pelvic volume; Consider partial closed reduction 1st
- High route: Iliac crest (3-5 cm posterior to ASIS); Place atleast 2 pins on each side
- Place at junction of lateral 2/3rd and medial 1/3rd of iliac crest
- Aim: 30-45 degrees from lateral to medial (towards the hip joint)
- Fluoroscopy: Outlet-oblique view
- Low route: Supra-acetabular (AIIS); Single pin
- Fluoroscopy:
- 30/30 outlet/obturator oblique view (to confirm entry location and direction)
- Iliac oblique (to confirm location above sciatic notch)
- Inlet/obturator oblique (to confirm depth)
- Direction: 30 degrees cephalad (towards SIJ) to avoid greater sciatic notch
- Provides better stabilization than high route
- Risk: lateral femoral cutaneous nerve
- Fluoroscopy:
3. Posterior stabilization with C-clamp:
- Entry point: Intersection of femoral axis line and a perpendicular line dropped from ASIS to bed
4. Pre-peritoneal pelvic packing:
- 6-8 cm midline longitudinal incision from pubic symphysis
- Divide midline fascia, leave peritoneum intact
- Retract bladder
- Place 3 lap pads on each side of bladder, into true pelvis below the pelvic brim
- Close fascia and skin
- Pack removal 24-48 hours later
5. Traction for vertical shear fractures:
- Bilateral upper tibial skeletal traction
- A heavy weight (upto 20 kg) may be required to achieve reduction
- After 3 weeks, weight is reduced to 10 kg
- Traction is removed after 6-8 weeks
6. Percutaneous ilio-sacral screws:
- Safe zone: S1 vertebral body
- Inlet view: guides antero-posterior screw placement
- Outlet view: guides superior-inferior screw placement
- Complication: L5 nerve root injury
7. Surgical approaches:
| Approach | Interval | Access | Acetabular fracture indications | Risks |
| Ilioinguinal | 1. Medial window: Medial to external iliac vessels 2. Middle window: Between external iliac vessels and iliopsoas muscle 3. Lateral window: Lateral to iliopsoas muscle | 1. Pubic rami, iliac fossa, anterior SIJ 2. Pelvic brim, quadrilateral plate 3. Quadrilateral plate, SIJ, Iliac wing | Both column Anterior wall Anterior column Anterior column-posterior hemi transverse Some T-type and transverse types | Obturator artery/nerve Corona mortis Femoral nerve/vessels Lateral femoral cutaneous nerve Spermatic cord, round ligament |
| Kocher-Langenbeck | Split gluteus maximus; detach short external rotators 1 cm from insertion Quadratus femoris left intact to protect femoral head blood supply | Outer table of ilium Sciatic notch Ischium Posterior wall | Posterior wall Posterior column Transverse | Sciatic nerve Superior gluteal artery Medial femoral circumflex artery Heterotopic ossification |
| Iliofemoral | Extensile approach | Posterior and anterior acetabulum Inner and outer table of ilium | High anterior column Both column T-type Fractures >3 weeks old | Heterotopic ossification High complication rates |
| Stoppa | Behind iliopectineal fascia to enter true pelvis Can use “lateral” window of ilioinguinal approach | Pubic symphysis Pelvic brim Quadrilateral plate | Anterior column Anterior wall Transverse T-type Both column Anterior column-posterior hemitransverse | Corona mortis Obturator nerve |
Cause of hemorrhage:
- Stable pelvic fractures: ~70% due to associated injuries and 30% due to pelvic fracture
- Unstable pelvic fracture: ~70% due to pelvic fractures and 30% due to associated injuries
Superior gluteal artery is the most common artery to be damaged. Internal pudendal artery yields the most symptomatic bleeds.
Further reading: Montmany S, Rebasa P, Luna A, Hidalgo JM, Cánovas G, Navarro S. Source of bleeding in trauma patients with pelvic fracture and haemodynamic instability. Cir Esp. 2015 Aug-Sep;93(7):450-4. English, Spanish. doi: 10.1016/j.ciresp.2015.01.011. Epub 2015 Mar 21. PMID: 25804517.

He is the section editor of Orthopedics in Epomedicine. He searches for and share simpler ways to make complicated medical topics simple. He also loves writing poetry, listening and playing music.