Synonyms: Hippocratic fingers, Acropachy, Dysacromelia, Drumstick fingers, Watch glass nails, Parrot beak fingers, Serpent head nails, Lovibond’s sign
Definition
Focal and bulbous enlargement of the distal phalanges due to proliferation of connective tissue between the fingernail and the bone with increase in both the longitudinal and transverse curvatures of the nail plate and obliteration of onychodermal or lovibond’s angle (angle between the nail base and the adjacent skin fold). It affects both the finger and toe nails.
Pathophysiology
Clubbing is characterized by an increase in the pulp tissue due to proliferation of subungual connective tissue, interstitial edema and dilation of arterioles and capillaries. Multiple theories have been put forward as an explanation it, however the most accepted theory currently is “Platelet hypothesis”.
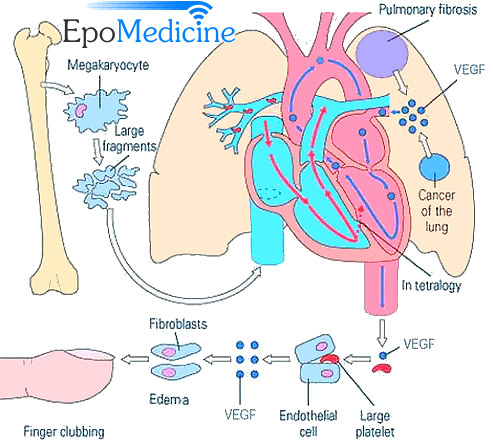
Megakaryocytes would normally break up in the pulmonary capillaries to the platelets but in the presence shunts or abnormal circulation within a neoplasm, these megakaryocytes bypass the pulmonary capillaries and reach the systemic circulation to preferentially lodge in the tips of the digits. These cells locally release Platelet Derived Growth Factor (PDGF) and VEGF along with other mediators that increase endothelial permeability and activate connective tissue cells including fibroblasts. Though widely accepted, this theory is unable to explain clubbing attributed to other several causes. Some of the other hypotheses are:
- Humoral: Unknown humoral substances dilate vessels in the fingertip (e.g. Acromegaly)
- Persistent hypoxia: Causes opening of deep AV fistula in fingers (e.g. Tetralogy of Fallot)
- Reduced ferritin in systemic circulation: Causes dilation of AV anastomoses and hypertrophy of terminal phalanx
- Vagal theory: Persistent vagal stimulation causes vasodilation and clubbing (e.g. Bronchiogenic carcinoma)
- Toxic: e.g. Subacute Bacterial Endocarditis (SABE)
- Metabolic: e.g. Thyorotoxicosis
Eliciting the Signs of Clubbing
1. Lovibond’s profile sign: Bring the patient’s fingertip at the level of your eye and look tangentially for the onychodermal or lovibond’s angle.
- Normal: less than or equal to 160º
- Clubbing: more than or equal to 180º
2. Curth’s modified profile sign: Similarly, you can measure the angle between the middle and distal phalanx.
- Normal: 180º
- Clubbing: less than 160º
3. Fluctuation test: The patients fingertip is placed on the pulp of examiner’s two thumbs and held in this position by gentle pressure with the tips of examiner’s middle fingers applied on the patient’s proximal interphalangeal joint. The patient’s finger is then palpated over the base of the nail by the tips of examiner’s index fingers. There is increased fluctuation of the nail bed in clubbing due to softening of the nail-bed.
4. Schamroth’s window test: The sign is elicited by placing the dorsal surfaces of terminal phalanges on opposing fingers together. The normally formed diamond shaped window is obliterated in the presence of clubbing. This sign is also known as diamond sign.
5. Digital index: Ratio of circumference of finger at nail-bed (NB) to distal interphalangeal joint (DIP) i.e. NB:DIP is calculated for all the 10 fingers and summed up. The final value is divided by 10 and the resulting value is digital index (>1 in clubbing).
6. Phalangeal depth ratio: Ratio of distal phalangeal depth (DPD) to interphalangeal joint depth (IPD) i.e. DPD:IPD of index finger measured using calipers (should touch the skin but not compress it) if >1 indicates clubbing.
Grades of clubbing
Various grading have been proposed for Clubbing but non has prognostic significance and is regarded as an utility of communication between the examiners. “Lung India” has proposed a grading based on the stages of clubbing:
- 1: Fluctuation and softening of nail-beds
- 2: Obliteration of the onychodermal angle (>160º)
- 3: Accentuated convexity of nail
- 4: Clubbed appearance of the fingertip
- 5: Development of a shiny or glossy change in nail and adjacent skin with longitudinal striations
Causes of Clubbing
A) Bilateral Clubbing:
Mnemonic: CLUBbING with ABCDEF extension of “L”
1. Cardiovascular: Cyanotic congenital heart disease (Fallot’s tetralogy), Subacute Bacterial Endocarditis (SABE), Atrial myxoma, Eisenmenger’s syndrome
2. Lung and pleural: Abscess, Bronchiectasis, Carcinoma, Cystic fibrosis, “Don’t say COPD”, Empyema thoracis, Fibrosis (Chronic interstitial lung disease)
3. Liver: Chronic active hepatitis, Cirrhosis
4. Ulcerative colitis
5. Biliary cirrhosis
6. Intestinal: Inflammatory Bowel Disease, Celiac disease, Lymphoma, Carcinoma, Ascariasis, Amebiasis
7. Normal: Idiopathic
8. Genetic: Pachydermoperiostitis (a syndrome that combines hyper-trophic osteoarthropathy and acromegalic features)
9. Other: Thyrotoxicosis (Thyroid acropathy), Occupational (Jackhammer operators)
Clubbing in COPD: Chronic emphysema and bronchitis doesn’t cause clubbing. The presence of clubbing in a patient with COPD should prompt a search for an underlying (lung) cancer, bronchiectasis or interstitial lung disease. In lung diseases, clubbing is seen either due to impaired lung function where PGE2 destruction by lungs is impaired or destruction of pulmonary capillaries resulting in escape of megakaryocytes into systemic circulation or excessive PGE2 or VEGF production by tumors.
According to some references, clubbing may be seen in chronic bronchitis but never in pure emphysema.
B) Unilateral Clubbing:
Asymmetrical clubbing usually indicates impaired regional blood flow caused by localized vascular disease or hemiplegia.
- Hemiplegia
- Aneurysm of subclavian artery, brachio-cephalic trunk, aortic arch, axillary artery, palmer arch
- Presubclavian coarctation of aorta (left sided clubbing)
- Pancoast tumor
- Unilateral erythromelalgia (a rare neurovascular peripheral pain disorder commonly associated with myeloproliferative disorders in which blood vessels, usually in the lower extremities, are episodically blocked, then become hyperemic and inflamed)
- AV fistula used for hemodialysis
- Infected arterial graft
Treatment for clubbing: There is no specific treatment for clubbing. The treatment is for the underlying primary condition.
Aids for diagnosis of cause of clubbing
- Drumstick type clubbing: Bronchiectasis, Congenital cyanotic heart disease (Mnemonic: BCD)
- Parrot-beak type clubbing: Bronchiogenic carcinoma
- Painful clubbing: Bronchiogenic carcinoma, SABE, Lung abscess
- Reversible clubbing: Lung abscess, Empyema thoracis
- Uni-digital clubbing: Hereditary, Repeated local trauma, Median nerve injury, Sarcoidosis
- Clubbing with cyanosis: Cyanotic heart disease, Pulmonary AV shunt, Pulmonary disease like lung abscess, bronchiectasis, cystic fibrosis
- Acute clubbing (Clubbing within 2 weeks after onset of illness): Lung abscess, Empyema thoracis
- Recurrent clubbing: May occur in pregnancy in otherwise healthy females
Differential clubbing
This type of clubbing is limited to upper or lower limbs alone and is often associated with cyanosis.
- Clubbing limited to upper extremity: Chronic obstruction of veins of the upper extremity (i.v drug users)
- Clubbing limited to lower extremity: PDA With reversal of shunt (Eisenmenger PDA), Infected abdominal aortic aneurysm
Pseudoclubbing
Pseudoclubbing is characterized clinically by asymmetrical involvement of fingers and radiographically by resorption of the terminal tufts (acro-osteolysis).
a. Subungual tumor or cyst
b. Subperiosteal bone resorption :
- Scleroderma
- Acromegaly
- Hyperparathyroidism
- Leprosy
- People working with vinyl choride


Hello,
which is the type of doctor to consult in case of suspect of initial or mild nail clubbing?
Is it the rehumatologist??
Thank you,
Edoardo Artioli
It’s best to consult to a family medicine or internal medicine. They’d evaluate if the finding is significant and also workup for the underlying cause if it’s significant.
Sir I’ve consult with the doctor for finger clubbing all test are good and normal what’s should I do now.
Son has had severe allergies and asthma all his life. Long term use of Benadryl and Prednisone. I have noticed over the years his fingernails are clubbed. Nails growing over the fingertips. Could it be the Benadryl. Or more serious medical condition?
Sir what is DIP and PIP method of grading clubbing?
Never heard of DIP and PIP grading for clubbing and couldn’t find anything on the web as well.
A profile angle (onychodermal angle) that approaches a straight line (180°) or phalangeal depth ratio that exceeds 1.0 (Distal phalangeal depth or DPD > Internphalangeal depth or IPD) indicate clubbing. If the angle is greater than 180°, definitive clubbing exists. An angle between 160-180° falls in a gray area and may indicate early stages of clubbing or a pseudoclubbing phenomenon.
YOU ARE GREAT