Osteomyelitis is defined as an inflammation of the bone (single portion or numerous regions, like marrow, cortex, periosteum and surrounding soft tissue) caused by an infecting organism (usually monomicrobial but polymicrobial can occur, especially in diabetic foot). Definitions, Criteria and Classifications of different types of Osteomyelitis have been discussed in the link below.
Arbitarily, acute osteomyelitis has been defined as those with duration of less than 2 weeks, subacute as those with duration of 2-6 weeks and chronic as those with duration more than 6 weeks. A more accurate definition is that the osteomyelitis is acute as long as the predominant histological and clinical picture is that of acute infection. When chronic inflammation and the secondary changes due to dysvascularity and scarring begin, the disease is defined as chronic.1
Common causative organisms of Acute Osteomyelitis:
| Organism | Comments |
| Staphylococcus aureus | Commonest in all types of osteomyelitis |
| Coagulase negative staphylococci or Propionibacterium | Foreign-body associated infection |
| Pseudomonas | IV drug users and Nosocomial infection |
| Streptococci or Anaerobic | Bite injuries, Diabetic foot lesion, Decubitus ulcer |
| Salmonella | Sickle cell disease |
| Bartonella henslae | HIV |
| Pasturella or Eikenella | Human or animal bites |
| Fungal | Immunocompromised patients |
| Mycobacterium tuberculosis | TB endemic regions |
| Group B streptococci | 2-4 weeks age (neonates) |
| H. influenzae | 6 months to 4 years age |
| Kingella kingae | <4 years age |
Predilection of Metaphysis for Osteomyelitis
- Vascular loops in metaphysis that take sharp bends and empty into venous lakes (hair-pin arrangement)
- Stasis and accumulation of pathogens
- Relative hypoxia (oxygen tensions <30 mmHg impairs phagocytic function)
- Relative absence of tissue macrophages (immature cells due to high turnover)
- Degenerating cartilage cells act as good culture medium
- Gaps in endothelium of growing metaphyseal vessels
- Allow passage of bacteria that may adhere to type I collagen in hypertrophic zone of physis
Biofilm
1. Planktonic (free floating) bacteria:
- Easily eradicated by host defenses
- Metabolically active and reproductive (antibiotic works against it)
- Forms irreversible cross-links with the inert surfaces (dead or necrotic tissue, foreign bodies, avascular body parts by direct contamination, contiguous spread or hematogenous seeding)
- ‘Race for the surface’:
- Host cells try to sequester non-viable material/tissue with neocapsule which is resistant to bacterial adhesion
- However, if bacteria encounter the surface and develop mature colonies, tissue integration by the host may be impaired and the process of infection may proceed
2. Stationary state bacteria:
- Following adhesion to surface, bacteria create a mucopolysaccharide layer called biofilm or slime and develop into colonies
- Pseudo-resistance to antibiotics:
- Insulated with a natural barrier of glycocalyx (slime)
- Decreased metabolic rate and phenotypic changes
- Body identifies these colonies as foreign and local inflammatory reactions also cause host tissue damage leading to more surface substrate for bacteria
- Release of bacteria and compromised host factors (immunosuppression, trauma, etc.) can lead to active infections
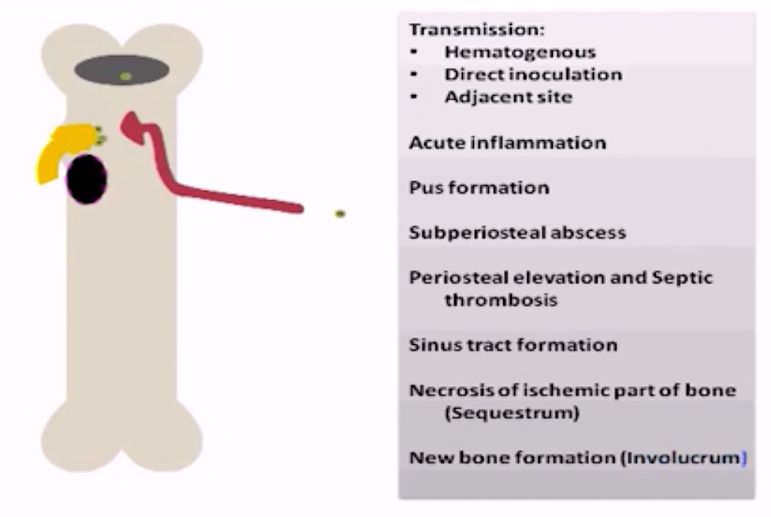
3 Routes of Infection
- Hematogenous (from distant septic foci)
- Direct inoculation (open fracture or surgery)
- Spread from adjacent sites (odontogenic infections leading to osteomyelitis of jaw)
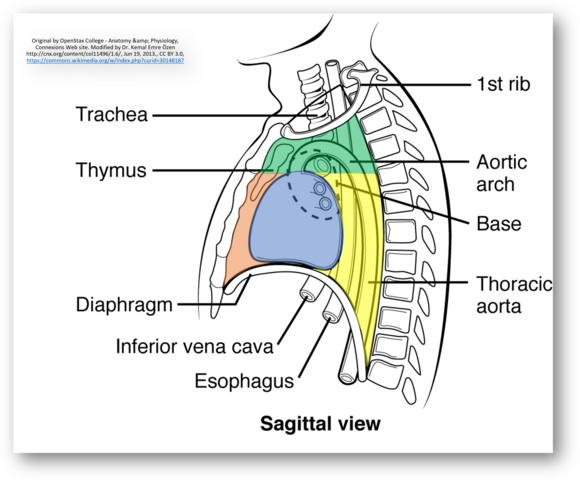
Progression of Osteomyelitis:
- Inflammation
- Bacteria multiply
- Production of IL-1 and PGE2 leading to bone resorption (within 12-18 hours)
- Before development of ossific nucleus: Common blood supply to the metaphysis and cartilaginous epiphysis may lead to infection of epiphysis and septic arthritis
- Suppuration
- Thrombosis of medullary vessels, further reducing host’s ability to fight infection
- Purulent exudate
- Increased intramedullary pressure
- Spread of pus:
- Children (thick and loosely adherent periosteum):
- Periosteum detached from cortex and subperiosteal abscess formed (further compromises bone’s vascular supply contributing to it’s ischemic necrosis)
- Spread along subperiosteal planes into adjacent joints (4 sites of intra-articular metaphysis)
- Proximal femur
- Proximal humerus
- Distal lateral tibia
- Proximal radius
- Adults: Dissect through periosteum and can generate sinus tracts in skin
- Children (thick and loosely adherent periosteum):
- Bone necrosis
- Causes: Increased intramedullary pressure by inflammation, thrombosis of medullary vessels and subperiosteal abscess
- Sequestrum: Dead and detached piece of bone with an inner smooth (facing lake of pus) and outer rough (towards granulation tissue) surface surrounded by infected granulation tissue trying to eat it.
- Types:
- Ring: External fixator
- Tubular/match stick: Sickle cell disease
- Coke and rice grain: TB
- Feathery: Syphilis
- Colored: Fungal
- Annular: Amputation stumps
- Types:
- Reactive new bone formation
- Periosteum however retains blood supply, remains viable and produces osteoid
- Involucrum: Sheath of reactive, new, immature, subperiosteal bone that forms around the sequestrum, effectively sealing it off the blood stream just like a wall of abscess
- Resolution and healing
Salmonella osteomyelitis is common in sickle cell disease due to hyposplenism, complement deficiency and bowel infarction leading to translocation of salmonella.

He is the section editor of Orthopedics in Epomedicine. He searches for and share simpler ways to make complicated medical topics simple. He also loves writing poetry, listening and playing music. He is currently pursuing Fellowship in Hip, Pelvi-acetabulum and Arthroplasty at B&B Hospital.