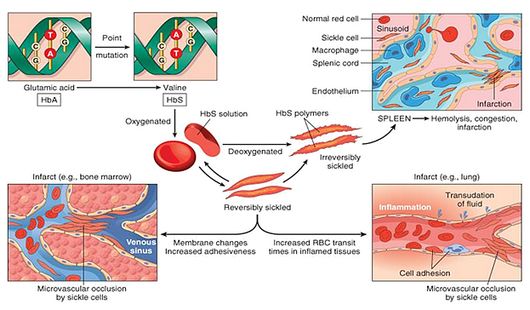
Sickle Cell Disease (SCD) is a hereditary disorder of hemoglobin synthesis caused by a mutation in the globin gene that changes the sixth amino acid from glutamic acid to valine resulting in abnormal sickling (rigid, inflexibled and sickle-shaped) of Red Blood Cells (RBCs) under low oxygen conditions. Sickle cell anemia is the homozygous state for Hb-S gene, while the heterozygous state is known as Sickle cell trait. The orthopedic manifestations of SCD are mainly attributable to the impairment of local circulation due to the clumping of sickle cells.
Acute orthopedic problems of Sickle Cell Disease
- Painful (vaso-occlusive) crisis
- Osteomyelitis
- Septic arthritis
- Bone infarcts
- Dactylitis (Hand-foot disease)
Chronic orthopedic problems of Sickle Cell Disease
- Osteonecrosis or Avascular necrosis of Femoral or Humeral head
- Chronic arthritis
- Osteoporosis
- Growth retardation/Skeletal immaturity
Why are infections so common in Sickle Cell Disease?
- Functional asplenia with decreased clearance of bacteria
- Tissue damaged by crisis
- Decreased neutrophil functions at lower oxygen tensions
- Decreased complement activity and opsonization
- Decreased IFN-ϒ production
- Increased risk of nosocomial infection
Why are Sickle Cell Disease patients susceptible to Salmonella infections?
1. Poor sanitation: exposes infants and young children to frequent gastrointestinal infection with salmonella.
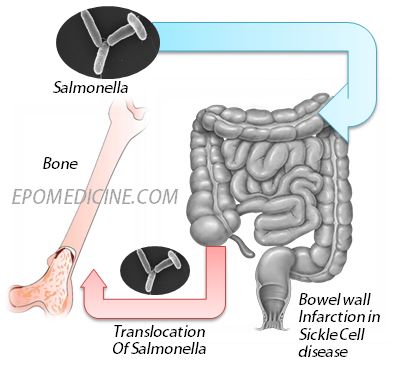
2. Bowel infarction: Blood stream invasion by salmonella is facilitated by devitalisation of areas of bowel wall due to intravascular sickling in the intestinal blood vessels. Areas of infracted bone are then infected by these blood borne organisms.
3. Bone marrow infarction: Expanded marrow in sicklers with its increased oxygen demand and metabolic activity and sluggish circulation is vulnerable to infarction. Devitalised infarcted areas are prone to infection with salmonella which characteristically tend to linger in bone marrow after other sites have become sterile.
4. RES dysfunction: Normally macrophages of the reticuloendothelial system eliminate salmonella from the body. In patients with sickle cell haemoglobinopathy macrophages are loaded with the breakdown products of the RBCs reducing their capacity to ingest and kill salmonella.
5. Hepatic dysfunction: and chronic haemolysis provide favourable conditions for salmonella to flourish.
Common organisms causing osteomyelitis in Sickle Cell Disease
- Salmonella typhimurium
- Salmonealla enteritidis
- Salmonella choleraesuis
- Salmonella paratyphi B
- Staphylococcus aureus
- Hemophilus influenzae
- Escherichia coli
- Enterobacter spp.
Note: While a lot of debate had been going about the commonest etiology of osteomyelitis in SCD (Salmonella or Staphylococcus aureus), many recent studies confirm Salmonella as the winner.
Salmonella Osteomyelitis
Usually affects children
Typically, involves diaphysis of long bones
Common sites: femur, humerus
Differential diagnosis: Difficult to differentiate from severe bone pain of vaso-occlusive crisis which is atleast 50 times more common than osteomyelitis in SCD (Ultrasonography, Radionucleide scanning and MRI may be helpful in differentiating as blood culture is usually negative in the 1st 1-2 weeks and the X-ray findings are also non-specific)
Confirmation of diagnosis: Growth of salmonella on culture
Treatment approach:
- Firstly, treated for Sickle cell crisis with hydration, analgesics and oxygen.
- If no improvement is seen in 24-48 hours, all septic foci is aspirated and empirical antibiotic covering both S.aureus and Salmonella is started.
- If no improvement is seen after 48 hours of initiation of antibiotics, surgical debridement is considered.
Thank you so much
What a clear and simple explaination
I’m still unclear on WHY salmonella specifically? Why not e coli? If the breakdown of the intestinal protection allows the bacteria through, why not the abundant e coli as opposed to Salmonella?
Thank you for the logical question.
“Salmonella normally do not cause sustained bacteremia because they are rapidly taken up by the phagocytic cell system and are effectively killed. Exceptions to this rule include some serovars (Typhimurium, Enteritidis, and Dublin) that spread systemically more often than the others and frequently cause focal systemic infections. Clinical conditions like sickle cell anemia, AIDS, leukemia, diabetes, etc that impair mononuclear cells enhance susceptibility to Salmonella bacteremia.” – Schaechter’s Mechanisms of Microbial Disease
“Interestingly, people with sickle cell anemia tend to develop Salmonella osteomyelitis, presumably because phagocytosis of the products of hemolysis prevents further cellular ingestion of the Salmonella organism and allows their dissemination through the bloodstream.” – Rubin’s pathology
Also, due to asplenia (due to repeated infarction) and defect in complement in patients with sickle cell anemia, they do not control encapsulated organisms well, so they have a very high rate of osteomyelitis. Salmonella is encapsulated while S.aureus and intestinal strains of E.coli are not capsulated (meningeal strains are encaspulated). This might be another reason why Salmonella osteomyelitis is more common than any other in sickle cell anemia.
I hope this will answer your doubt.
Thanks a lot. This was just perfect.
Am a bit confused, I wanna why does salmonella target sickle cell anaemia and not other types of anaemia?
In sickle cell anemia, the probable site for entry of Salmonella is intestinal wall where microinfarctions (caused due to microvascular occlusion by sickle cells) allow the organism to enter circulation. This is not the case in other common types of anemia. Also, there is reduction in complement-mediated serum opsonizing activity for salmonella, in association with other consequences of abnormal reticulonendothelial system function, which may predispose to salmonella bacteremia in sickle cell anemia.
Pathophysiology is briefly depicted in the first figure.