Definition: Glaucoma is a group of disorders characterized by a progressive optic neuropathy resulting in a characterstic appearance of the optic disc and a specific pattern of irreversible visual field defects that are associated frequently but not invariably with raised intraocular pressure (IOP). It is one of the commonest cause of irreversible
blindness in the world. Open-angle glaucoma has been referred to as the “thief of sight.”
Classification of Glacuoma:
Glaucoma can be classified in a number of ways based on:
- Absence or presence of causative factors: primary or secondary
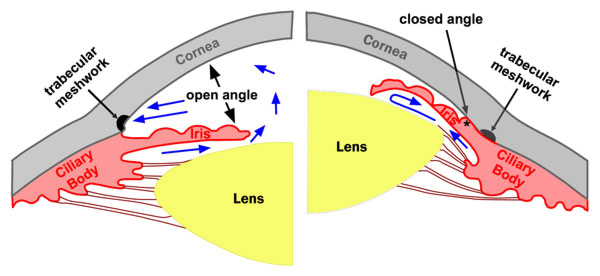
- Anatomy of the drainage angle: open angle or angle closure.
- Speed of onset:
- Acute: sudden elevation of IOP with features like ocular pain and redness
- Chronic: gradual elevation of IOP
- Age of onset:
- Congenital: At birth or before birth
- Infantile: Birth until 3 years of life
- Juvenile: 3 years to adulthood
- Adult: Adulthood
- Level of IOP: normal tension glaucoma (characteristic glaucomatous optic neuropathy with IOP in the normal range) or ocular hypertension (IOP above the normal range but no glaucomatous optic neuropathy).
| Form of glaucoma | Angle (anatomic) | Angle (gonioscopy) | Outflow impediment |
| Primary Open Angle Glaucoma (90%) | Open | Completely open. Structures appear normal. | In the trabecular meshwork (Idiopathic). |
| Secondary Open Angle Glaucoma (2-4%) | Open | Completely open. Trabecular meshwork and secondary occluding cells visible. | Erythrocytes, pigment and inflammatory cells occlude trabecular meshwork. |
| Primary Angle Closure Glaucoma (5%) | Blocked | Occluded. No angle structures visible. | Iris tissue occludes trabecular meshwork. |
| Secondary Angle Closure Glaucoma (2-4%) | Blocked | Occluded. No angle structures visible. Occluding structures visible. | Displacement of trabecular meshwork produces anterior synechiae, scarring and neovascularisation. |
| Congenital and Developmental Glaucoma (1%) | Undifferentiated | Open. Occluding embryonic tissue and lack of differentiation visible. | In the trabecular meshwork which is not fully developed or is occluded by embryonic tissue (Barkan membrane). |
| Absolute Glaucoma | Not a separate form of glaucoma but rather describes an often painful eye, blinded by glaucoma. | ||
Congenital (Buphthalmos) and Developmental Glaucoma:
- Primary:
- Congenital glaucoma (before or at birth)
- Infantile glaucoma (birth to 3 years)
- Juvenile glaucoma (3 years to adulthood)
- Glaucoma associated with developmental abnormalities:
- High insertion of peripheral iris: Axenfeld-Rieger syndrome, Peter’s anomaly
- Fine strands that contract to close angle: Aniridia
Secondary Open Angle Glacuoma:
A. Pre-trabecular (Membrane covering trabeculum):
- Fibrovascular tissue: Neovascular glaucoma
- Endothelial cellular membranous proliferation: ICE syndrome
- Epithelial cellular membranous proliferation: Epithelial ingrowth
B. Trabecular (Clogging up or Alteration of meshwork):
- Pigment particles (pigmentary glaucoma, malignant glaucoma)
- Red blood cells (red cell glaucoma)
- Degenerate red cells (ghost cell glaucoma)
- Macrophages and lens proteins (phacolytic glaucoma)
- Proteins (lens induced glaucoma and hypertensive uveitis)
- Pseudoexfoliative material (pseudoexfoliation glaucoma)
- Drugs (Steroid induced glaucoma)
- Edema (herpes zoster iritis/trabeculitis)
- Scarring (post-traumatic angle recession glaucoma)
C. Post-trabecular (Increased episcleral venous pressure):
- Carotid-cavernous fistula
- Cavernous sinus thrombosis
- Idiopathic episcleral venous pressure elevation
- Mediastinal tumors
- Infiltrative ophthalmopathy (thyrotropic exophthalmos)
- Retrobulbar tumors
- Sturge-Weber syndrome
- Superior vena cava (SVC) obstruction
Secondary Closed Angle Glaucoma:
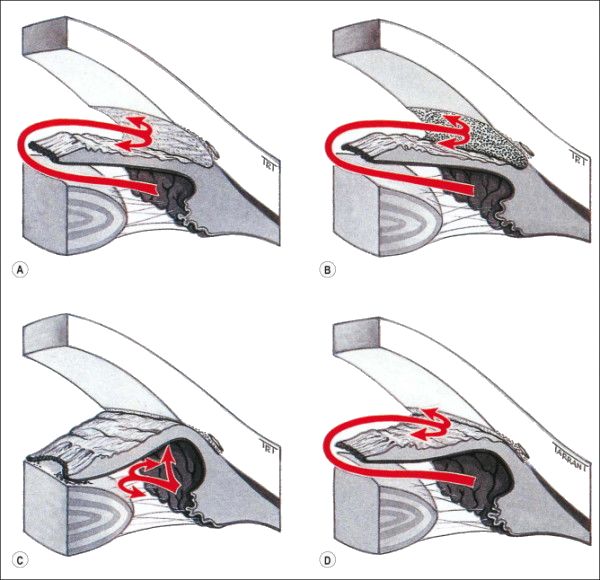
A. Anterior (Iris pulling mechanism):
- Contracture of membranes: ICE syndrome, Neovascular glaucoma, Trauma
- Contracture of inflammatory precipitates
- Inflammatory membrane: Fuch’s heterochromic iridocyclitis, Luetic inerstitial keratitis
B. Posterior (Iris pushing mechanism):
1. With pupillary block:
- Lens-induced: Intumescent lens, Lens subluxation
- Posterior synechiae: Iris-vitreous block in aphakia, Pseudophakia, Uveitis
- Pupillary block glaucoma
2. Without pupillary block:
- Ciliary block (malignant glaucoma)
- Cysts of iris and ciliary body
- Forward vitreous shift after lens extraction
- Intraocular tumors (malignant melanoma, retinoblastoma)
- Lens-induced (intumescent lens, lens subluxation)
- Plateau iris syndrome
- Uveal edema (scleral buckling, panretinal photocoagulation, central retinal vein occlusion)
- Retrolenticular tissue contracture (persistent hyperplastic primary viterous, retinopathy of prematurity)
The ISGEO classification of Glaucoma for Epidemiological Surveys:
A. Primary Open-angle Glaucoma (POAG)
Glaucomatous optic neuropathy in the presence of an open-angle and no other ocular abnormality to account for a secondary mechanism.
B. Primary Angle Closure Glaucoma (PACG)
1. Primary angle-closure suspect (PACS)
- Occludable angle: Appositional contact between the peripheral iris and posterior trabecular meshwork deemed possible
2. Primary angle-closure (PAC)
- Occludable angle plus
- Signs of trabecular meshwork obstruction: Peripheral anterior synechiae, elevated IOP, excessive pigment deposition on surface of trabecular meshwork or ischemic sequelae such as glaucomflecken or iris whirling
3. Primary angle-closure glaucoma (PACG)
- PAC plus
- Glaucomatous optic neuropathy
C. Secondary Glaucomas
Glaucomatous optic neuropathy together with signs of other pathological processes.
Rotterdam Study (2000 criteria) for Primary Open Angle Glaucoma or Chronic Simple Glaucoma:
If present in at least 1 eye with open angle and no history or sign of secondary glaucoma. No IOP criteria.
1. Definite Opena Angle Glaucoma (OAG):
- Glaucomatous Visual Field Defect (GVFD) plus
- Possible Glaucomatous Optic Neuropathy (GON):
- Vertical Cup to Disc Ratio (VCDR) ≥ 0.7, OR
- Asymmetry between both eyes ≥ 0.2, OR
- Minimal rim width < 0.1.
2. Probable OAG:
- GVFD without possible GON, OR
- Absence of GVFD or with probable GON
- VCDR ≥ 0.9, OR
- Asymmetry ≥ 0.3, OR
- Minimal rim width < 0.05
3. Possible OAG: Possible GON and no GVFD.