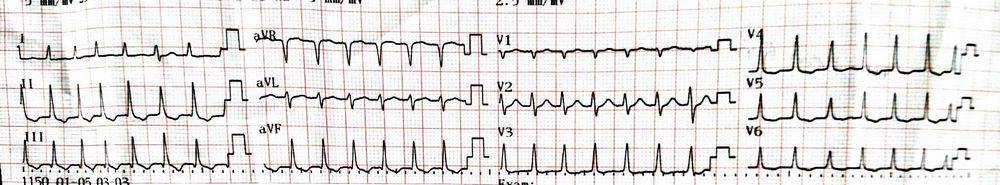
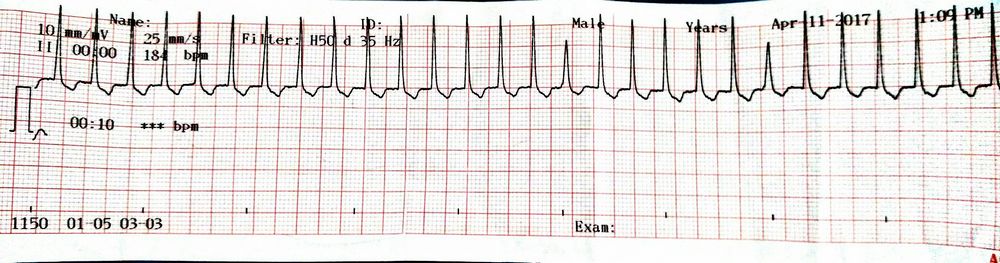
This is an ECG from a patient who came with a complaint of palpitation:
Analyze the ECG:
- Rhythm: Regular
- Heart rate: Around 170/min
- QRS: Around 0.08 s i.e. ≤0.1 s (narrow QRS complex)
ECG diagnosis: Regular Supraventricular Tachycardia (SVT)
Now, look for P waves – There are no P waves
In a regular SVT, absent P wave indicate junctional or AV nodal origin of SVT.
Normal P waves in regular SVT would indicate SA nodal origin of SVT like sinus tachycardia.
Flutter waves in regular SVT are characteristic of Atrial flutter.
AV nodal SVT can be:
- Atrioventricular re-entrant tachycardia (AVRT) – consists of anatomical re-entry circuit (Bundle of kent)
- Atrioventricular nodal re-entry tachycardia (AVNRT) – consists of functional re-entry circuit in AV node
- Automatic junctional tachycardia
AVNRT is the commonest cause of palpitation in patients with structurally normal heart.
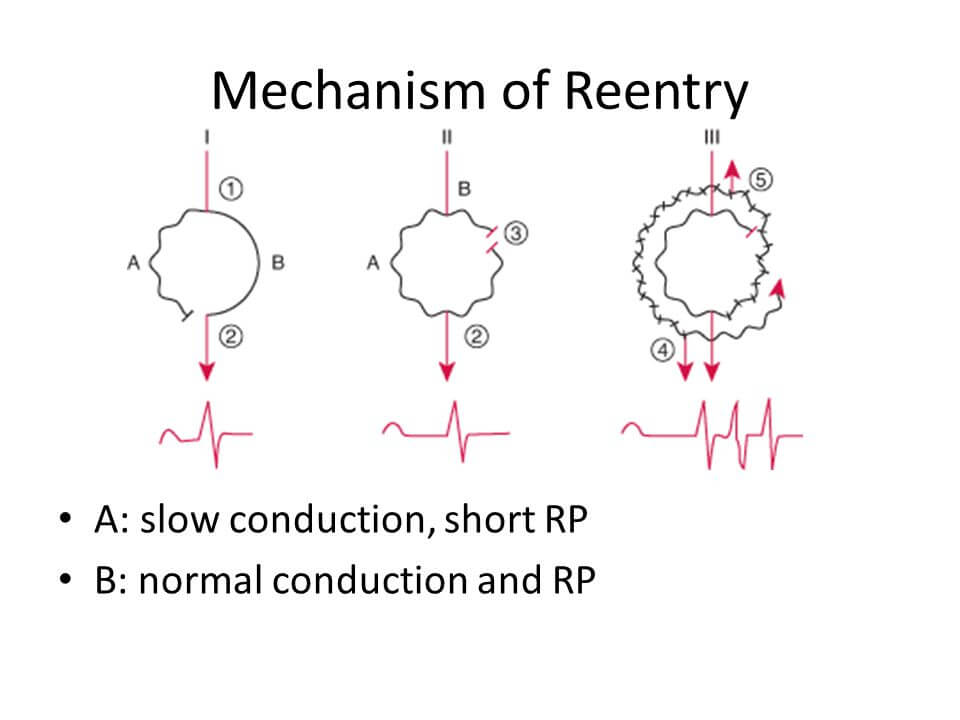
In the above figure:
I – Normal sinus rhythm: Impulse is transmitted via normal (fast) pathway and impulse through slow pathway meets the refractory period of fast pathway – hence, the impulse in slow pathway is not conducted.
II – Premature atrial contraction: Normal (fast) pathway has longer refractory period. When premature atrial contraction occurs when the normal pathway is in refractory period – the impulse is solely transmitted through the slow pathway. By the time, impulse through the slow pathway reaches the end of slow pathway, the refractory period of the normal (fast) pathway has ended.
III – Now, the impulse throught the slow pathway travels retrogradely in normal pathway creating a re-entry loop. In this continuous loop:
- Anterogradely – Bundle of His is activated
- Retrogradely – Atria is activated (this is the reason P waves are retrograde if seen in AVNRT)
- Slow pathway has short refractive period – Tachycardia
This is the mechanism for typical AVNRT (slow-fast AVNRT) which accounts for 80-90% of AVNRT.
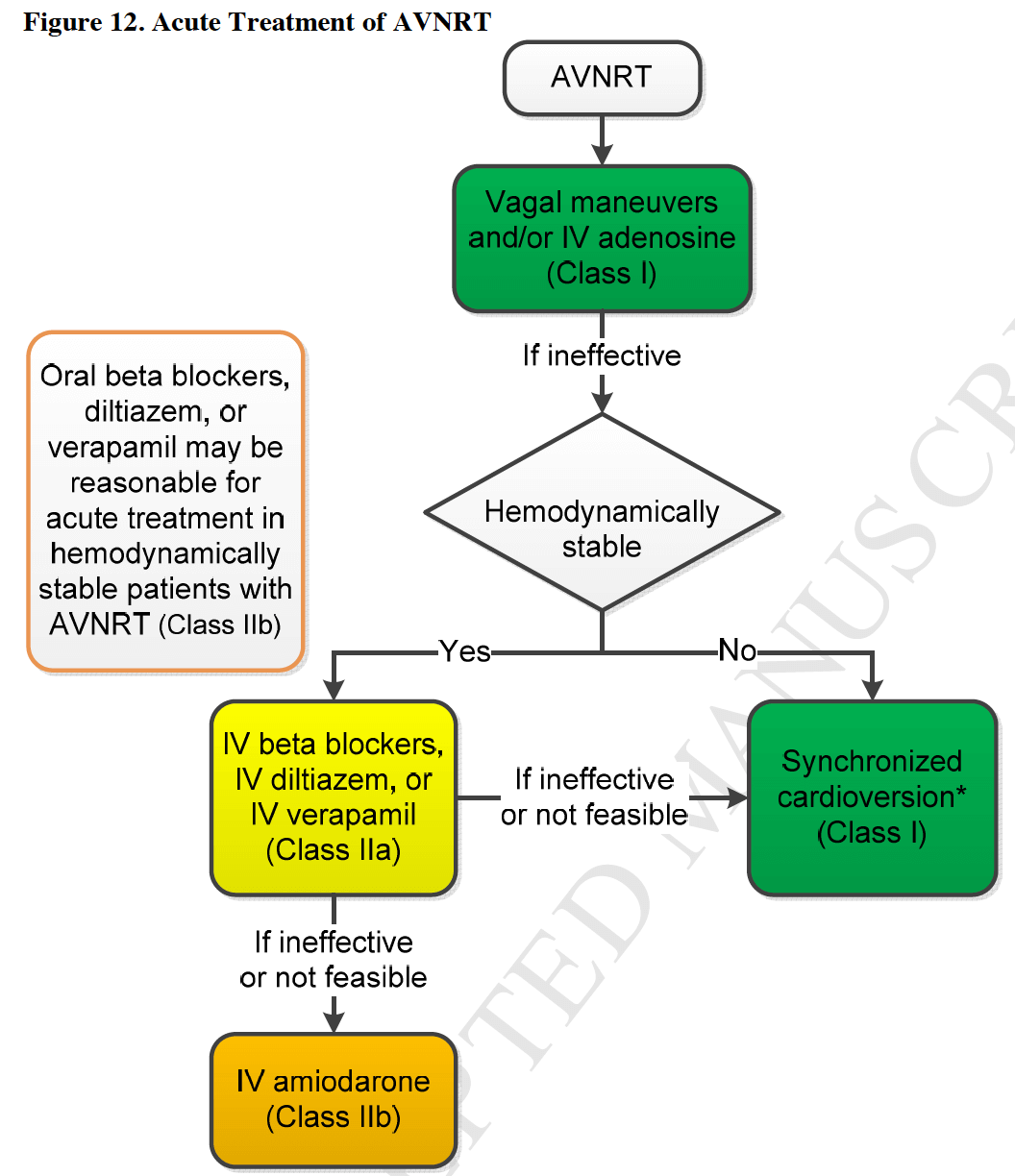
Acute Treatment of AVNRT as per ACC guidelines
Adenosine
Note: For any iv medication, infusion should be stopped as soon as the arrhythmia is terminated or in the event of sustained or non-sustained VT or marked prolongation of QTc. Patients should be observed for atleast 4 hours after infusion or until QTc has returned to baseline.
Initial dose: 6 mg rapid IV bolus (injected into IV as proximal or as close to the heart as possible), administered over 1-2 s, followed by rapid saline flush.
Subsequent or maintenance dose: If no result within 1-2 minutes, 12 mg rapid IV bolus; can repeat 12 mg dose 1 time. The safe use of 18 mg bolus doses have been reported.
Mechanism of adenosine in AVNRT
Activation of adenosine A1 receptor results in activation of outward potassium current. This effect of adenosine hyperpolarizes the cell membrane to a value approaching Ek (Equilibrium potential of K+). Because atrial and ventricular tissue already rests near Ek, adenosine has little or no effect in these tissues. However, in SA and AV nodal tissue, adenosine hyperpolarizes the cell, reducing the likelihood of firing an action potential, thus slowing or blocking conduction. Adenosine also slows nodal conduction by inhibiting ICa through reducing 3′,5′-cAMP. 1
It has been reported to precipitate severe bronchospasm in patients with pulmonary disease. The drug is therefore contraindicated in asthmatic subjects and should be used with caution in patients with chronic obstructive pulmonary disease. Nevertheless, true bronchospasm is rare and should be distinguished from the much more common occurrence of dyspnea, only as a symptom and without respiratory compromise, which is benign and transient. Aminophylline (an adenosine antagonist) can be used to revert the bronchospasm caused due to aminophylline.
Caution has to be exercised when using adenosine due to a potential proarrhythmic effect stemming from a transient increase in vulnerability for AF.
If hypotension is a consideration, a slow infusion of diltiazem (2.5mg/min) or verapamil (1mg/min) for upto 20 minutes may lessen the potential for hypotension.
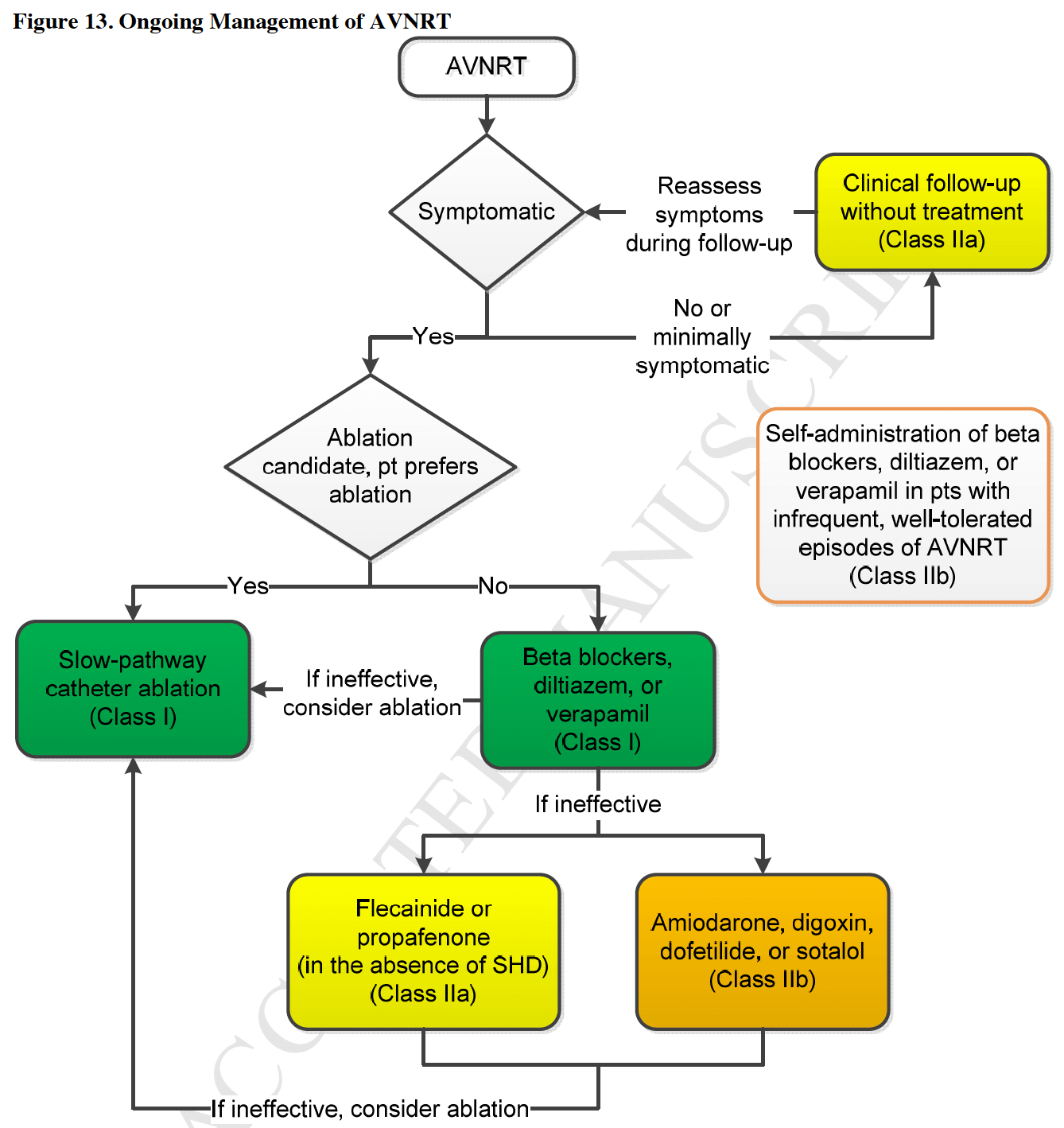
Chronic Treatment of AVNRT as per ACC Guidelines
Finally, let’s go back to the previous ECG. There are T wave inversions in lead II, III, aVF and V4-V6. The T wave inversions are not deep and asymmetrical which are not in favor of pathologic T wave inversions. The cardiac enzymes were also normal in this patient.
Can these inverted T waves be associated with AVNRT?
In a study of patients greater than 45 years of age with PSVT, 21 of 39 patients had atleast 1 mm of ST depression. Of these 21 patients, only 7 had significant coronary artery stenosis on coronary angiography.
In a study of 63 patients with PSVT, 25 patients had new T inversions within 6 hours. Of these only 2 had confirmed CAD.2

He is the section editor of Orthopedics in Epomedicine. He searches for and share simpler ways to make complicated medical topics simple. He also loves writing poetry, listening and playing music.