Synonyms: Paleness
Definition of Pallor
Pallor is the paleness of skin and mucous membranes, due to the reduced amount of oxyhemoglobin or decreased peripheral perfusion.
Sites to look for pallor
- Lower palpebral conjunctiva
- Tip and dorsum of the tongue
- Soft palate
- Nail beds
- Palmar or plantar creases
- General body skin
Pallor in lower palpebral conjunctiva:
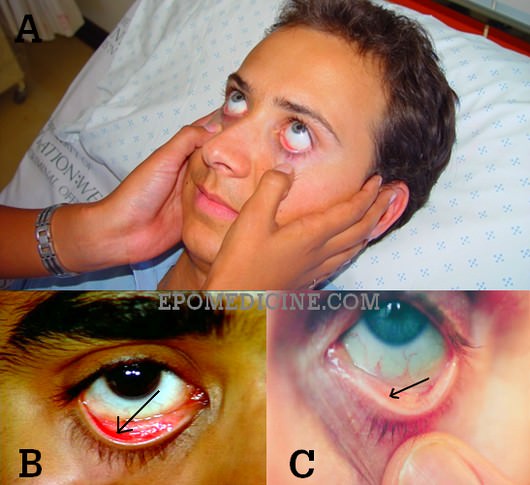
B. Normal conjunctiva (Note the demarcation shown by arrow)
C. Pale conjunctiva (Loss of demarcation)
How (Technique)? Pull the lower eyelid down and compare the color of anterior part of the palpebral conjunctiva (attached to the inner surface of the eyelid) with the posterior part where it reflects off the sclera. There is usually a marked difference between the distinctly red anterior and pearly white posterior parts. This difference is absent when significant anemia is present. 1
Use both your thumb to retract eyelids downward on both the sides simultaneously and as you do so, ask the patient to look upwards.
Why(Reason)? The mucosa over this region is very thin and the underlying vessels are clearly seen and the pallor can be judged.
Pallor in palms:
How? As the patient to hyper-extend the fingers. Compare the color of palmar crease with that of the adjacent skin of palm. Pallor is said to be present if both are of same color.
Different studies showed that palmar crease pallor has high specificity for severe anemia, but sensitivity of it is low. Possibility of palmar creases to be as pale as the surrounding skin is high in fair skinned western population. In darker/more pigmented race, palmar crease pallor may be less effective as a marker of severe anemia.
Pallor in nailbeds:
How? Press the nail and note the color of nailbed after releasing the digital pressure.
Mechanism of Pallor in Anemia
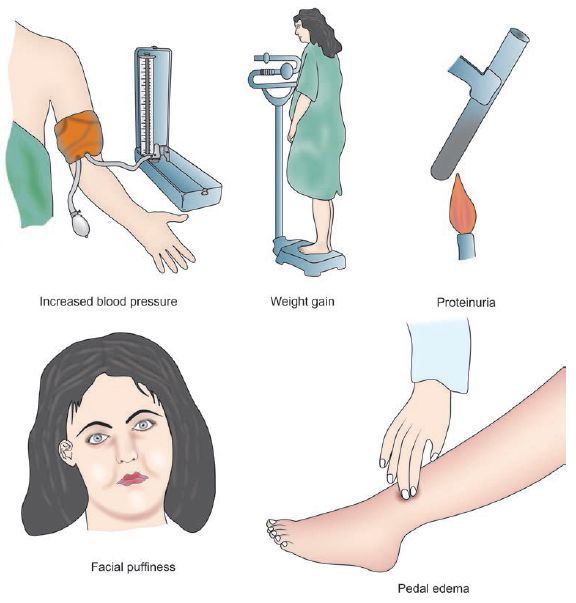
Causes of pallor
1) Anemia (can be appreciated clinically when hemoglobin <8-9 g/dl)
2) Pallor without anemia:
- Physiologic (“fair skinned”)
- Shock
- Hypoglycemia and other metabolic derangements
- Respiratory distress
- Skin edema
- Pheochromocytoma
Pallor and Anemia
Although often used as synonyms, presence of pallor doesn’t always indicate anemia. Pallor is a sign, while anemia is a diagnosis based on laboratory results. Anemia is the qualitative or quantitative dimunition of RBC and/or hemoglobin concentration in relation to standard age and sex.
Clinical grading of anemia:
- Mild: Pallor of conjunctiva and/or mucous membrane
- Moderate: Above + Pallor of skin
- Severe: Above + Pallor of palmar creases
A study revealed that the presence of pallor can modestly raise the probability of severe anaemia while its absence can rule out severe anaemia. Neither presence nor absence of pallor, regardless of its severity, can accurately rule in or rule out moderate anaemia. Absence of conjunctival pallor and tongue pallor completely ruled out the probability of haemoglobin <7 g/dL. 3
WHO grading of anemia:
- Mild: 10 g/dl to cut off point for ages
- Moderate: 7-10 g/dl
- Severe: <7 g/dl
Hemoglobin thresholds used to define anemia:
- Men (>15 years): 13 g/dl
- Teens (12-15 years): 12 g/dl
- Women, non-pregnant (>15 years): 12 g/dl
- Women, pregnant: 11 g/dl
- Children (5-12 years): 11.5 g/dl
- Children (0.5-5 years): 11 g/dl
Variations
When assessing for pallor in darkly pigmented patients, you might experience difficulty because the underlying red tones are absent. This is significant because these red tones are responsible for giving brown or black skin its luster. The brown-skinned individual will manifest with a more yellowish brown color, and the black-skinned person will appear ashen or gray. 4
Tips to aid assessment
Look for the coexistence of other signs, which may help to aid the diagnosis of the etiology of anemia.
- Tachycardia (Congestive Heart Failure/CHF)
- Edema (CHF, nephritic syndrome)
- Pulse volume (shock)
- Nail changes (koilonychia and paltyonychia in Iron Deficiency Anemia; splinter hemorrhages in associated thrombocytopenia)
- Skin changes (hyperpigmentation in megaloblastic anemia; petechiae in malignancies, aplastic anemia)
- Lymphadenopathy and hepatosplenomegaly (malignancy)
- Icterus (hemolytic anemia)
Special features of Anemia
Iron deficiency anemia:
- Koilonychia
- Angular stomatitis
- Glossitis
- Dysphagia
Megaloblastic anemia – Vitamin B12 deficiency:
- Subacute combined degeneration
- Peripheral neuropathy
- Severe glossitis
- Beefy-red tongue
Hemolytic anemia:
- Icterus
- Lemon-yellow color of skin
- Leg ulcers
- Splenomegaly
Thalassemia:
- Chipmunk facies
- Retarded growth
- Splenomegaly
Sickle cell anemia:
- Tower shaped skull
- Small trunk
- Long arms
- Leg ulcers
- Bony tenderness
- Osteomyelitis
- Poor growth
- Auto-splenectomy in adults
It’s anemia. I’ve got the blood test from the hosiptal today.I had to be in a hosiptal to receive this diagnosis!:)It’s sad but we have to laugh otherwise we lose our minds.Tomorrow I’ll go to a GP who “hates physicians!”:)I told him I hate physicians on the first time we met and he reply: “Me too. My mother went to a doctor and when I arrived home she was having a drug that she can’t because of the other drug she takes. I almost prosecuted this…. !” -You’re right. Same of my colleagues are not supposed to medicate.”
What does rcdw mean, how it aid in diagnosis?
Red cell distribution width (RDW) is a measure of anisocytosis (variability in RBC size) i.e. standard deviation of MCV.
RDW = (Standard deviation of red cell volume X 100)/Mean cell volume
Normal range = 11 to 15%
For more details on red cell indices and RDW: http://epomedicine.com/medical-students/understanding-red-cell-indices/
Its red cell distribution width. It actually measures the degree of anisocytosis among red cells in perpheral smear. More the variation in sizes among RBCs more is the rcdw.
This part shown by arrow, if its white, then im anemic?
The arrow shows the demarcation line between red anterior part and pale posterior part. If this demarcation line is unclear, it may be a sign of anemia.
could you please give me the reference of the book from which can get the following text
wondering the same thing. where did he get all those info. not written in classic textbooks?
Why should we check lower palpebral conjuctiva for pallor and upper palpebral conjunctiva for icterus?
We don’t check palpebral conjunctiva for icterus. It is the upper bulbar conjunctiva. Bulbar conjunctiva is transparent and window to the sclera which is rich in elastin which readily binds the bilirubin. For more information: http://epomedicine.com/clinical-medicine/clinical-examination-icterus/
Pallor is to be looked for in palpebral conjunctiva. We look for in lower palpebral conjunctiva because it is easier to retract compared to the upper one which requires eversion. The answer to why we look for pallor in palpebral conjunctiva has been mentioned in the article. The mucosa over this region is very thin and the underlying vessels are clearly seen and the pallor can be judged.
excellent article on anemia. I have not found most of it on macleod’s, clinical exam. or hutchinson clinical methods or Bate’s physical exam.. So may i ask ur references please?
Hello Shahriar,
The text presented are derived from various sources. The classic textbooks don’t answer most of the reasoning questions` – however, they provide concise and “must know” information and are to be “referenced” for exam purposes. You can find most of the texts in books. Here, for examination of conjunctival pallor, comparison with the anterior and posterior part is recommended. This has been mentioned in around here – http://onlinelibrary.wiley.com/doi/10.1046/j.1525-1497.1997.00014.x/pdf
The posterior forniceal conjunctiva is pale compared to anterior and the author recommends comparing the two.
thanks very much. :-))
Can we see pallor in a patient with deep jaundice. If yes where..?
Yes, you can assess for pallor in lower palpebral conjunctiva in cases of deep jaundice.
such a nice way to describe briefly this disease