Author: Sulabh Kumar Shrestha, KISTMCTH
A) RELEVANT ANATOMY AND PHYSIOLOGY
Details of the body fluid compartments are described here
Microvessels for fluid exchange:
The Exchange Vessels – capillaries and most proximal part of the venules
- Sinusoidal capillaries (liver, spleen, bone marrow): freely permeable to all solutes
- Fenestrated capillaries (glands, glomeruli, GIT): permeable to fluid and small solutes
- Continuous capillaries (rest): high permeability for small solutes except in brain but restricted permeability for protein
- In the brain, the interendothelial junctions are tighter, which results in low permeability to all solutes, including small solutes such as sodium and chloride ions, but permeability for water is still relatively high.
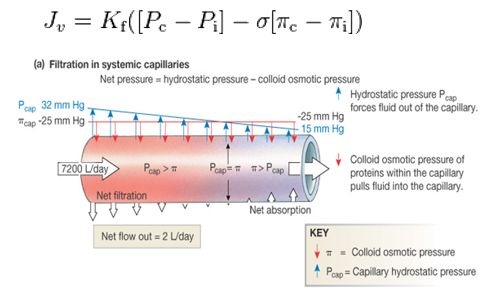
Starling’s equation:
Daily electrolyte requirements:
- Sodium: 1-2 mEq/kg
- Potassium: 0.5-0.8 mEq/kg
- Chloride: 1-2 mEq/kg
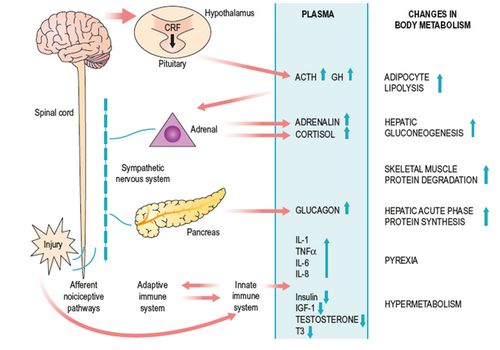
Stress response to surgery:
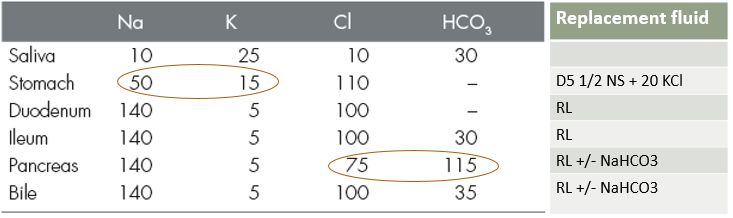
Composition of GI secretions and appropriate replacement fluid:
B) GLUCOSE SOLUTIONS
Needs of the brain, RBC, adrenal medulla, and wound healing ~ 120 mg/kg/hr (equivalent to Glucose 5% every 6 hrly)
Nitrogen sparing effect: 3 l of buffered glucose 5% provides 600 kcal of energy – although too little for basic needs, this still reduces the muscle-wasting characteristic of starvation
Cellular swelling by D5W: 50 g of dextrose adds 278 mOsm/L to an iv fluid (close to plasma).
- Osmolality effect rapidly wanes once dextrose is taken up by cells and metabolized – added water then moves into cells
- 1/3rd moves into ECF and remaining 2/3rd into ICF
Cellular dehydration by D5NS:
- 5% dextrose (278 mOsm/L) + 0.9% NS (308 mOsm/L) = 586 mOsm/L (~2 X plasma osmolality)
- If glucose utilization is impaired (critically ill), large-volume infusions can result in cellular dehydration.
Lactate production:
- Healthy: 5% of glucose load into lactate formation
- In hypoperfused state (critically ill): 85% of glucose load into lactate formation
Indications of glucose solutions:
- Alcoholics
- Patients on parenteral nutrition treated with highly concentrated glucose solutions
- Pancreatic islet cell tumors
- Hepatomas
Problems of glucose solutions:
- Cerebral damage associated with hyperglycemia:
- Acute stroke
- Surgeries with risk of cerebral ischemia: carotid artery and cardiopulmonary bypass
- Impaired lung function:
- Consider CO2 production from glucose – increased load to ventilation
- Raised ICP in head trauma
- Glucose shouldn’t be infused through same equipment used for blood – hemolysis and clumping can occur
Use of glucose solution:
- Large evaporation loss: Plain glucose 5%
- Modest degree of evaporation: buffered glucose 2.5%
- Postoperative follow-up:
- buffered glucose 2.5% (which is half-isotonic with respect to electrolytes) is better
- unlikely to cause subacute hyponatremia
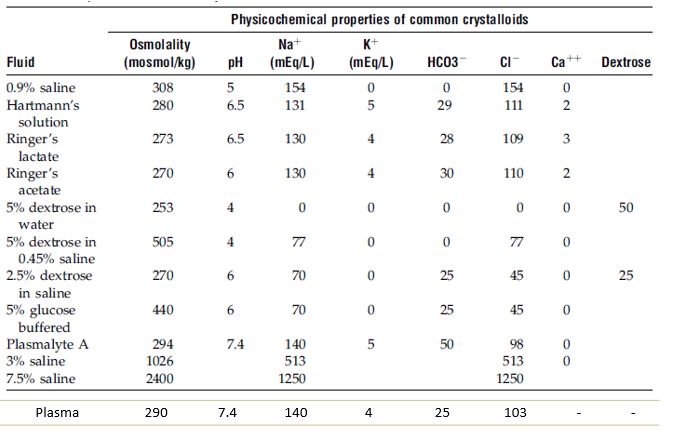
C) CRYSTALLOID SOLUTIONS
Composed of low molecular weight solutes (<30,000 D) – ionic (Na+ and CL-) or non-ionic (mannitol)
Do not contain large oncotic molecules – pass freely across microvascular membrane
Predominant effect is interstitial volume expansion:
- Plasma volume is only 25% of the interstitial fluid volume
- Only 25% of an infused crystalloid fluid will expand the plasma volume
- While 75% of the infused volume will expand the interstitial fluid
Infusion of 1 L NS increases ECF volume by 1.1 L (NS is slightly hypotonic – fluid shift from ICF to ECF)
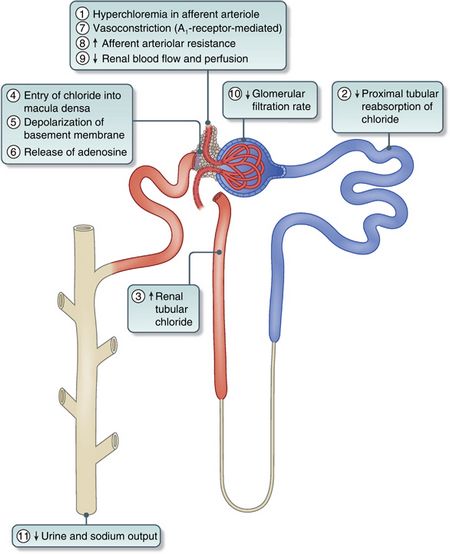
NS results in:
- Interstitial edema: Increased Na in patients with limited cardiac, renal and hepatic functions
- Decreased renal perfusion: Chloride-mediated renal vasoconstriction
- Hyperchloremic metabolic acidosis: Higher Cl- concentration compared to plasma (154 vs 103)
- Strong Ion Difference (SID) + Hydrogen ion = 0Normal plasma SID = Na (140) – Cl (3) = ~ 133
- For NS: SID = Na (154) – Cl (154) = 0
- For RL: SID = Na (130) + K (4) + Ca (3) – Cl (103) = ~ 28
A change in SID must be accompanied by reciprocal change in [H+] or pH (i.e. more for NS and less for RL)
Ringer’s lactate:
- Lower Na concn. (compensatory for sodium lactate)
- Lower Cl concn. (compensatory for negatively charged lactate)
Ringer’s acetate:
- Capacity to metabolize lactate is mainly dependent on the functional capacity of the kidney and the liver.
- Acetate can be metabolized by all tissue cells, which could be beneficial if the patient is hypovolemic or in shock.
Advantage of Ringer’s lactate and Ringer’s acetate over isotonic saline (0.9% NaCL): lack of a significant effect on acid-base balance.
Disadvantage of Ringer’s solutions: is the calcium content i.e., the ionized calcium can bind the citrated anticoagulant in stored RBCs and promote clot formation.
Concerns over serum lactate level:
- In healthy: infusion of 1 liter of RL over 1 hour does not raise serum lactate levels.
- In critically ill:
- may have impaired lactate clearance from circulatory shock or hepatic insufficiency
- if lactate clearance is 0, addition of 1 l of RL (28 mM/L) to blood volume of 5 l, would raise the serum lactate level by 4.6 mM/L
- Hence, RL is unlikely to affect serum lactate level unless large volume is infused in critically ill patients
- Blood samples obtained from intravenous catheters that are being used for RL infusions can yield spuriously high serum lactate determinations.
Normosol and Plasmalyte:
- Contain magnesium instead of calcium, and contain both acetate and gluconate buffers to achieve a pH of 7.4
- No calcium – suitable as diluents for RBC transfusions
- Plasma-Lyte – less tendency to promote interstitial edema when compared with isotonic saline
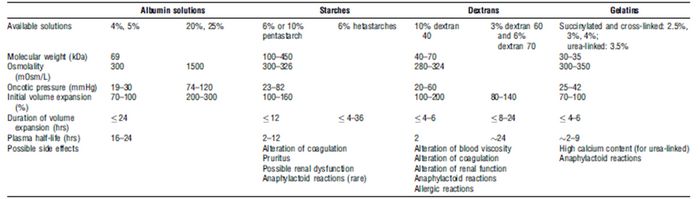
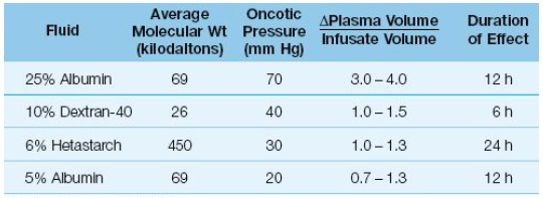
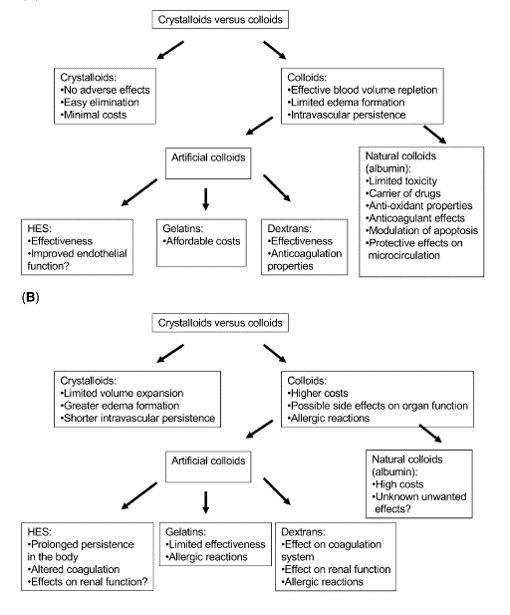
D) COLLOID SOLUTIONS
Colloid fluid is a saline solution with large solute molecules that do not pass readily from plasma to interstitial fluid.
The retained molecules in a colloid fluid create an osmotic force called the colloid osmotic pressure or oncotic pressure that holds water in the vascular compartment.
- Colloid osmotic pressure of plasma = 28 mmHg
- Iso-oncotic colloids: 20-30 mmHg colloid osmotic pressure
- Hyper-oncotic colloids: >30 mmHg colloid osmotic pressure
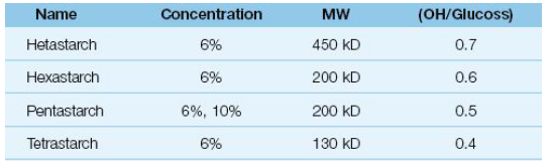
Hydroxyethylstarch (HES):
Addition of hydroxyethyl groups, preventing them from degradation by endogenous amylase
Types:
- Concentration: low (6%) or high (10%)
- Average MW (amylase cleavage results in progressively smaller molecules that are osmotically active. When the cleavage products reach a molecular weight of 50 kD, they can be cleared by the kidneys): low (70 kDa), medium (200 kDa), or high (450 kDa)
- Degree of substitution (modification by hydroxyethyl addition – greater resistance to degradation): low (0.45–0.58) or high (0.62–0.70)
- C2/C6 ratio (site of substitution on initial glucose molecule – higher means greater half life): low (<8) or high (>8)
Effects:
- Can impair hemostasis (inhibits platelet adhesion, factor VII and vWF)
- Associated with nephrotoxicity (mechanism unclear)
- Associated with hyperamylasemia 2-3X with lipase unaffected (amylase binds to HES)
Voluven – Newer HES preparation with minimal effect on coagulation
E) HYPERTONIC SOLUTIONS
Rapid onset of plasma volume expansion e.g. 3% NaCl, 9% NaCl
Administration of 250mL HSD to a 70-kg patient who had suffered a 2-L blood loss would result in plasma volume expansion of at least 700mL (or, in other words, a three- to fourfold increase to the infused volume). To achieve at least momentarily the equivalent plasma volume (If RL ~ 3 L would be necessary)
Mainly beneficial for pre-hospital purposes and battlefield conditions
Other Indications: Severe hyponatremia, Cerebral edema, Hydatid cyst surgery (Scolicidal)
F) PROBLEM BASED APPROACH TO FLUID SELECTION
- Life-threatening hypovolemia from blood loss (prompt increase in plasma volume necessary): iso-oncotic colloid fluid (e.g., 5% albumin)
- Hypovolemia secondary to dehydration (Uniform loss of ECF): crystalloid fluid (e.g., Ringer’s lactate)
- Hypovolemia with hypoalbuminemia (fluid shifts from plasma to interstitial fluid): hyperoncotic colloid fluid (e.g., 25% albumin)
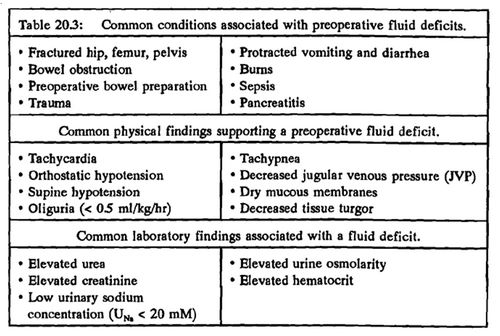
Assessment for fluid therapy:
- Clinical assessment of the patient’s fluid status, i.e. replacement vs maintenance
- Where a fluid deficit is identified (e.g. haemorrhage or vasodilatation, diarrhoea or vomitus, insensible or renal losses) – the nature of the fluid deficit must be identified.
- The type of fluid which will best treat the deficit or maintain euvolaemia.
- The appropriate rate of fluid administration guided by clinical assessment and safety limits.
- The proposed clinical endpoint.
- Continued monitoring of fluid and electrolyte status.
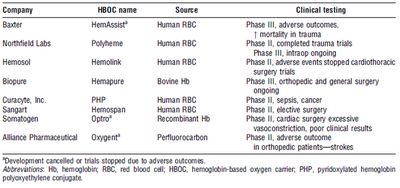
Oxygen carrying plasma expanders (RBC substitutes or Oxyglobins):
G) PREOPERATIVE FLUID MANAGEMENT GUIDELINES:
Clear fluids not to be withheld for > 2 hrs (unless gastric emptying disorder)
Carbohydrate rich drink 2-3 hrs before surgery
- Reduces postoperative insulin resistance
- Facilitates recovery from surgery
Bowel preparation to be avoided whenever possible
- Simultaneous correction with Hartmann’s/RL if mandatory
Gastric aspirates/vomiting to be treated with K+ containing crystalloid
- Hypochloremia is an absolute indication for use of NS
Losses from diarrhea/ileostomy/small bowel fistula/ileus/obstruction to be replaced volume for volume with Hartmann’s or RL or RA
“Saline depletion” for example due to excessive diuretic exposure – Balanced electrolyte solution – Hartmann’s
Hypovolaemia due predominantly to blood loss – Balanced crystalloid solution or a suitable colloid until packed red cells available.
Hypovolaemia due to severe inflammation such as infection, peritonitis, pancreatitis or burns – suitable colloid or a balanced crystalloid.
Diagnosis of hypovolaemia is in doubt and the central venous pressure is not raised – response to a bolus infusion of 200 ml of fluid tested
For period of >24 hours but < 1 week:
- 2/3rd D5W + 1/3rd NS + 15-20 mEq K+/l OR
- ½ NS + 15-20 mEq K+/l
For period <24 hours:
- NS or RL
- K+ replacement no needed
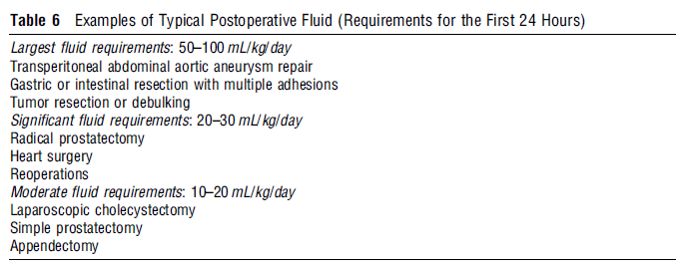
H) POSTOPERATIVE FLUID MANAGEMENT GUIDELINES
Review volume and type of fluids given – compare with fluid losses in OT including urine and insensible losses.
In euvolaemic and haemodynamically stable patients – return to oral fluid administration as soon as possible
In patients requiring continuing i.v. maintenance fluids, sodium poor and of low enough volume until the patient has returned their sodium and fluid balance over the perioperative period to zero.
Once achieved, fluid should replicate daily maintenace requirement and replace ongoing losses
In patients who are oedematous, hypovolaemia if present must be treated, followed by a gradual persistent negative sodium and water balance based on urine sodium concentration or excretion.
Plasma potassium concentration should be monitored and where necessary potassium intake adjusted.
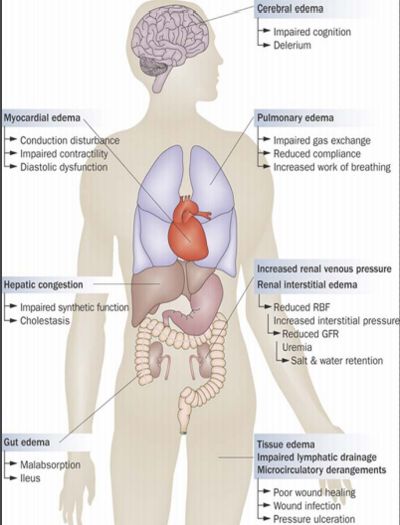
Hazards of overhydration:
I) PERIOPERATIVE FLUID MANAGEMENT CALCULATIONS
1. Deficit: NPO to beginning of surgery
- NPO hours X Maintenance fluid
- Also account for NG losses, losses from bowel preparation, ostomy and fistulas
2. Maintenance: Incision to closure of wound
Based on the 4 – 2 – 1 formula
- 4 ml/kg/hr for 0-10 kg weight
- 2 ml/kg/hr for the next 10 kg weight
- 1 ml/kg/hr for each kg > 20
- A shortcut for patients weighing > 20 kg is weight in kg + 40
3. Surgical losses:
Blood:
- Replace 3-4 ml crystalloid/ml blood loss or 1 ml colloid/1 ml blood loss
- Replace blood at 1 ml/1 ml loss + crystalloid or colloid
- fully soaked sponge (4*4) = 10 ml of blood
- soaked lap = 100 – 150ml
Evaporation from open wound
Third-spacing from fluid redistribution
Estimation of Evaporation and Third-Space Losses—additional maintenance fluid based on amount of tissue trauma
- Minimal procedure, e.g. herniorrhaphy 2-4 ml/kg/hr
- Moderate procedure, e.g. cholecystectomy 4-6 ml/kg/hr
- Major procedure, e.g. bowel resection 6-8 ml/kg/hr
Schedule for Replacement During the Surgical Procedure:
- First hour: 1/2 the deficit + maintenance + replacement for blood loss
- Second hour: 1/4 the deficit + maintenance + replacement for blood loss
- Third hour: 1/4 the deficit + maintenance + replacement for blood loss
4. Preloading: For loss of sympathetic tone following anesthesia
Example:
80 kg patient scheduled for total hip replacement, NPO for 10 hours
Deficit = 10 hours NPO X 120 = 1200 ml
Maintenance = 120 ml/hr
Blood loss replacement (EBL = 300 ml) = 3 ml crystalloid X 300 = 900 ml
1st hour = 600 (1/2 the deficit) + 120 (maintenance*) + 300 ml LR (blood loss replacement) = 1020 ml
2nd hour = 300 (1/4 the deficit) + 120 (maintenance*) + 300 ml LR (blood loss replacement) = 720 ml
3rd hour = 300 (1/4 the deficit) + 120 (maintenance*) + 300 ml LR (blood loss replacement) = 720 ml
Total = 2460 ml
*Additional fluid may be added to the hourly maintenance to account for evaporation and tissue trauma losses
Another approach:
- Deficit: NPO hours X 2 ml/kg
- Maintenance: Dependent upon the type of procedure and duration of surgery
- Extremity procedure, arthroscopy, thyroidectomy: 5 ml/kg/hr
- Mastectomy, laparoscopic procedures: 8 ml/kg/hr
- Minor open abdominal procedures (hysterectomy, cholecystectomy): 8-10 ml/kg/hr
- Colon resection, thoracotomy: 12 ml/kg/hr
- Extensive procedures (spinal fusion): 15-20 ml/kg/hr
- Blood replacement: As before
Schedule of replacement: As before
I) FLUID SPACING
1st spacing: Normal body fluid distribution
2nd spacing: Excess fluid accumulation in interstitium (edema)
3rd spacing: Fluid accumulation from vascular space/ plasma (ECF) into an area normally having minimal to no fluid; sequestration of fluid into interstitial space or body cavity
Causes of 3rd spacing:
- Decrease in plasma proteins
- Increased capillary permeability: trauma, radiation, sepsis, surgical manipulation
- Lymphatic blockage
| Phase I (Fluid loss) | Phase II (Reabsorption) |
| Occurs immediately after surgery or trauma | Capillaries heal and normal permeability returns |
| Lasts 48-72 hours | Lymph block clears |
| Increased capillary permeability and leaking of fluid and proteins | Fluid volume shifts back to vascular space, and is excreted by kidneys |
| Treatment: | Treatment: |
| Administer fluids 200-1000 ml/hr | Recognize signs and symptoms: Increased urine output, decreased specific gravity, output > input, weight loss |
| Monitor VS, urine output, specific gravity, CVP, PA, PACWP | Monitor for circulatory overload: ECG changes, SOB, Rales, Increased CVP, distended neck veins, Possible electrolyte imbalance |
| Monitor K+, BUN, Creatinine | |
| Auscultate chest for breath sounds | Can give Lasix if severe symptoms |
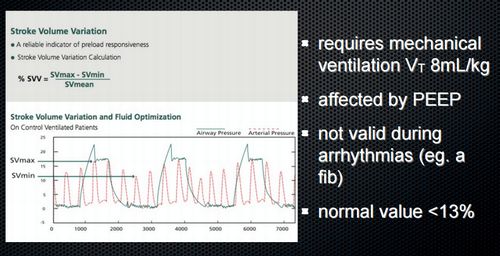
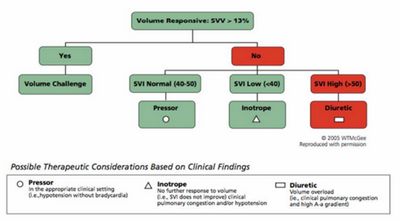
J) GOAL DIRECTED FLUID THERAPY – NEW APPROACH
The assumption of 5 “facts” which was the basis for classical approach:
- Fasting patients are hypovolemic
- Insensible loses increase dramatically with skin incision
- Unpredictable massive fluid shift into the “Third space” must be countered
- The kidneys will take care of any excess fluid
- Fluid unlike vasopressors are always safe
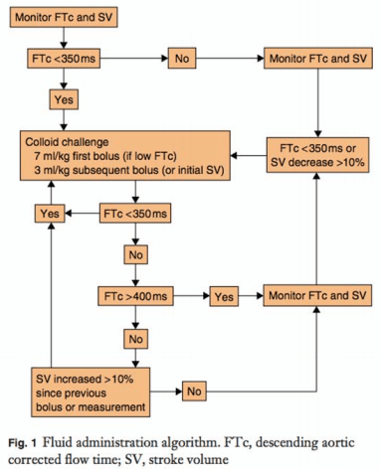
Goal directed therapy: The concept of giving fluids or other therapies to reach hemodynamic goals.
- Hemodynamics / systolic pressure variation
- CVP / PCWP
- Cardiac output / SV
- O2 delivery (CO plus SaO2)
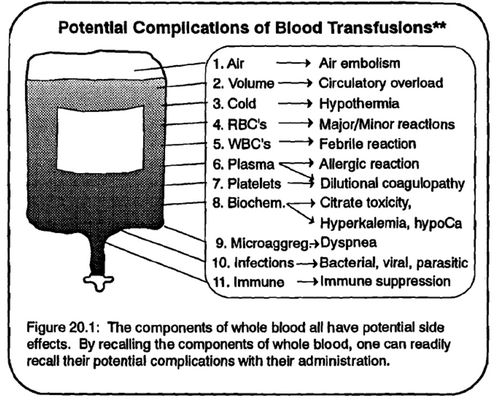
K) TRANSFUSION
“Transfusion Trigger”: Hgb level at which transfusion should be given.
- Varies with patients and procedures
Tolerance of acute anemia depends on:
- Maintenance of intravascular volume
- Ability to increase cardiac output
- Increases in 2,3-DPG to deliver more of the carried oxygen to tissues
Delivery of oxygen is dependent upon cardiac output and oxygen carrying capacity of blood which in turn is dependent upon Hemoglobin. Hence, in cardiac compromised patients, oxygenation is largely dependent upon the level of hemoglobin.
ASA practice guidelines:
- Transfusion rarely indicated when Hgb > 10 g/dL
- Transfusion almost always indicated with Hgb < 6 g/dL
- At levels between 6 and 10, it depends upon the situation upon the situation
- Use of a universal Use of a universal “transfusion trigger transfusion trigger” is not recommended not recommended
- Allowable blood loss (ABL) = (Initial Hb – Final Hb)/Final Hb X Estimated blood volume
Blood is administered at an initial rate of 0.25 mL/kg/hour for the first 15 minutes. Constant monitoring of the recipient during this time enables observation of any potential transfusion reaction. The rate is then increased to 20 mL/kg/hour. The total volume of blood is administered over 2–4 hours.
Anemia in critically stressed patients:
- In bleeding but otherwise healthy patients, cardiovascular compensation is adequate to Hb 5 g/dl
- Further compensation inadequate with mortality 50-95% at Hb < 3.5 g/dl
- Critical care and 28-day mortality were higher in patients receiving blood
Packed RBCs (pRBCs):
- 1 unit = 250 ml. Hct. = 70-80%.
- 1 unit pRBC’s raises Hgb 1 gm/dL.
- Mixed with saline: RL has Calcium which may cause clotting if mixed with pRBC’s
Platelet concentrate:
- Treatment of thrombocytopenia
- Intraoperatively used if platelet count drops below 50,000 cells/mm3 (lab analysis).
- 1 unit of platelets increases platelet count 5000-10000 cells/mm3.
Risks:
- Sensitization due to HLA on platelets
- Viral transmission
Fresh Frozen Plasma (FFP):
- Plasma from whole blood frozen within 6 hours of collection.
- Contains coagulation factors except platelets
- Used for treatment of isolated factor deficiencies, reversal of Coumadin effect, TTP, etc.
- Used when PT and PTT are >1.5 normal
Risks:
- Viral transmission
- Allergy