A) Indications:
- Clinical or radiological evidence of involvement of axillary nodes
- Microscopically positive sentinel node(s) due to metastasis from primary malignant tumor
- In sentinel node negative: 98 % accurate in predicting that the other nodes are negative
- In sentinel node positive: possibility of microscopic disease in any of the remaining lymph nodes is 15–30 %
- When sentinel lymph node cannot be identified at the time of mapping
- Palpable axillary nodes when axilla is not the regional basin, within the context of complete mastectomy for a tumor amenable to this approach (eg. melanoma)
B) Contraindications:
- Absolute: None
- Relative:
- Comorbidities prohibiting GA or Operative procedure
- Pre-existing lymphedema
- Shoulder immobility
C) Relevant anatomy:
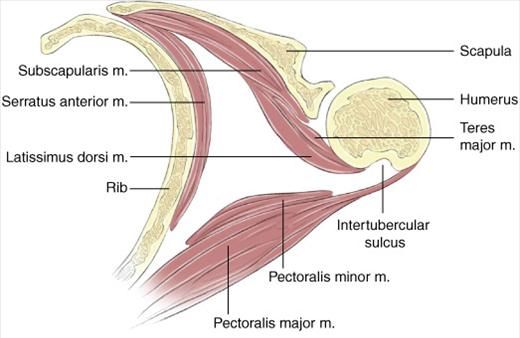
a. Boundaries of axilla:
- Superiorly: Axillary vein
- Anteriorly: Pectoralis major and minor (encased within clavipectoral fascia)
- Posteriorly: Subscapularis, teres major and scapular insertion of latissimus dorsi
- Laterally: Latissimus dorsi
- Medially: Serratus anterior and chest wall
The apex of the triangle (the highest point of the axillary dissection) is the costoclavicular ligament or Halsted ligament.
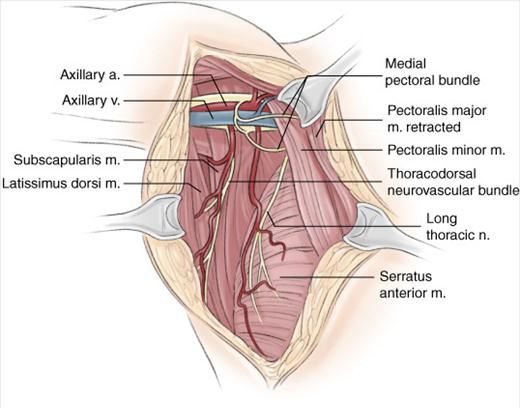
b. Contents of axilla:
It contains a rich complex of neurovascular and lymphatic structures within a layer of dense connective tissue known as the axillary sheath.
- Long thoracic nerve (C5-C7): innervates serratus anterior
- courses vertically along the superficial surface of serratus anterior (lateral chest wall in midaxillary line)
- injury leads to winging of scapula and limitation of abduction of arm above shoulder
- Thoracodorsal nerve (C6-C8): innervates long thoracic nerve
- courses lateral to long thoracic nerve (courses inferolaterally on posterior axillary wall)
- Medial pectoral nerve (from medial cord of the brachial plexus, C8-T1): innervates pectoralis major and minor
- lateral to or through pectoralis minor
- injury may result in muscle atrophy
- Lateral pectoral nerve (from lateral cord of the brachial plexus, C5-C7): innervates pectoralis major
- medial to pectoralis minor and medial pectoral nerve
- injury causes atrophy of pectoralis major
- Intercostobrachial nerves (lateral cutaneous branches of 1st and 2nd intercostal nerves + medial cutaneous nerve of arm)
- travels transversely across the axilla after emerging from 2nd intercostal space
- sensory innervation to skin of axilla and upper medial arm
- Axillary artery: originates medial to pectoralis minor and crosses axilla transversely
- 2nd part of the axillary artery lies behind the pectoralis minor – gives thoracoacromial and long thoracic branches
- Distal to these branches is thoracodorsal artery
- Axillary venous branches: parallel to arterial anatomy
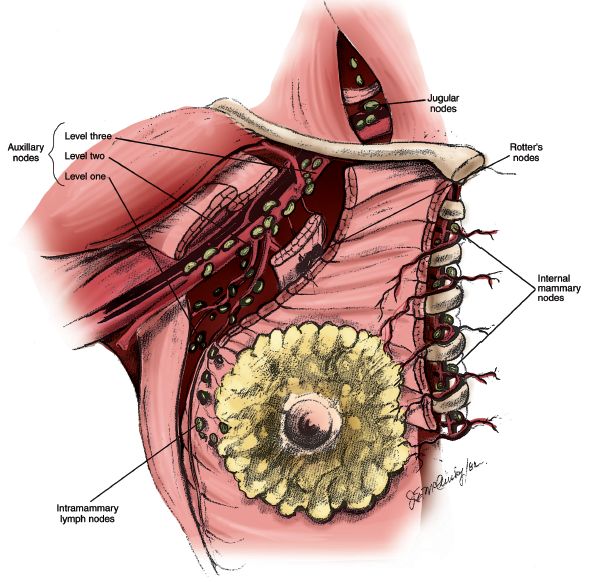
c. Axillary lymph node levels:
- Level I (lateral to pectoralis minor):
- Pectoral (anterior): along inferior border of pectoralis minor
- Subscapular (posterior): along subscapular artery and veins
- Humeral (lateral): along distal part of axillary vein
- Level II (behind the pectoralis minor):
- Central: at the base of axilla, embedded in axillary fat
- Some apical nodes
- Level III (medial to pectoralis minor):
- Majority of apical nodes: along axillary vein between clavicle and pectoralis minor
- Additional lymph nodes: Rotter’s node in rotter’s space between pectoralis major and minor
d. Congenital anomalies:
- Langer arch: abberant fibers of latissimus dorsi extending anteriorly and medially towards pectoralis major muscle; found in ~ 5% of patients undergoing axillary dissection
- failure to recognize its presence may result in residual nodal tissue being left medial to the true latissimus dorsi insertion (the lateral border of the dissection)
- when identified, it is severed at the level of lateral axillary vein
- Bifid or trifid axillary vein: avoiding ligation of structure travelling transversely before identification of axillary vein avoids injury
D) Operative Technique:
1. Anesthesia: GA
2. Positioning: supine on the operating table with the arm extended on to an armboard at 90 degrees (relaxes pectoralis major and allows better access into medial aspects of axilla; extending arms above 90 degrees may result in brachial plexopathy)
3. Painting and draping
4. Incision:
- With mastectomy: mastectomy incision is used
- Without mastectomy: curvilinear incision extending within curve of axilla from pectoralis major to medial border of latissimus dorsi
- better cosmetically
- possible ischemic effects are equal for both anterior and posterior flaps
- centered over lymph nodes of the nodal basin
- provides good exposure to entire nodal basin, axillary vein and spaces above and below it
5. Skin flap creation: Medially upto lateral border of pectoralis major, laterally upto medial border of latissimus dorsi, superiorly to level of axillary vein and inferiorly upto 4th or 5th ribs
6. Dissection of axillary vein:
- Identification:
- Lateral border of dissection: Follow latissimus dorsi superiorly until it becomes tendinous (inserts in the floor of biccipital groove of humerus) – at this level axillary vein lies anterior to the muscle
- Medial border of dissection: Axillary vein is found along an imaginary line extending from the groove between the biceps and triceps muscle (when the arm is abducted) toward the medial pectoral bundle
- Inferior aspect of the axillary vein is skeletonized of lymphatic and fatty tissue, with care being taken to avoid including superior tissue as the specimen is retracted inferiorly (to prevent lymphedema). All inferiorly coursing superficial branches from the axillary vein are ligated and divided.
7. Dissection of Level II and III nodes:
- Retract pectoralis major and minor medially
- Medial pectoral nerve is visualized just lateral to pectoralis minor
- Lymphatic tissue on chest wall is retracted inferolaterally as dissection is continued to inferior aspect of axillary vein
- After level II and III nodes has been freed from inferior aspect of axillary vein, this tissue can be swept laterally into level I of axilla
8. Completion of dissection:
- long thoracic nerve lies approximately 1 cm from the chest wall, deep in the axilla and superficial to the investing fascia of the serratus anterior muscle – often palpated as “piano string” in fatty tissue
- blunt spread in a plane superficial and parallel to the nerve can dissect the nerve from the surrounding axillary tissue and place it back against the chest wall
- tissue lateral and inferior to long thoracic nerve can be divided
- thoracodorsal neurovascular bundle is indentified just lateral to long thoracic nerve and deep to thoracoepigastric vein
- remaining tissue between long thoracic nerve and thoracodorsal nerve is removed
- lateral aspect of thoracodorsal neurovascular bundle is skeletonized
- Hemostasis is confirmed and a single closed suction drain placed. A skin closure with absorbable sutures is performed.
Extent of dissection:
Dissection of the level I and II lymph nodes is sufficient unless:
- Axillary nodal burden is high
- Grossly palpable level III nodes or Rotter’s node
Involvement of Level III is rare if Level II is not involved (<1%)
Level III nodes are positive in 2% with <3 positive axillary notes and 20% with 4-8 positive nodes
Adequacy of dissection: Level I and II lymph nodes and minimum of 10 lymph nodes
Postoperative management:
- Drain out when <30-50 ml/day
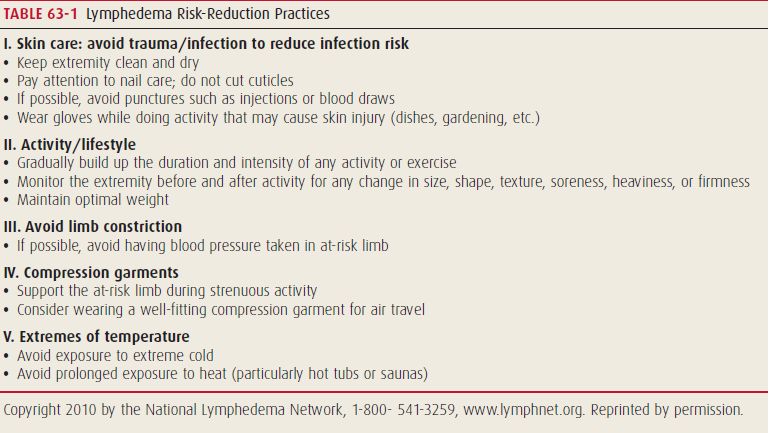
- Lymphedema risk-reduction:
Complications:
- Neurovascular injury: As explained in relevant anatomy section
- Hematoma: Use of supportive brassiere reduces incidence
- Wound infection
- Seroma: early postoperative shoulder mobility increases the incidence of seroma formation; potential benefit of delay in range-of-motion (ROM) exercises on seroma formation must be balanced against the potential negative impact on shoulder morbidity.
- Brachial plexus neuropathy: most commonly as a result of patient positioning error rather than direct dissection of nerves
- Lymphedema
- Decreased range of motion