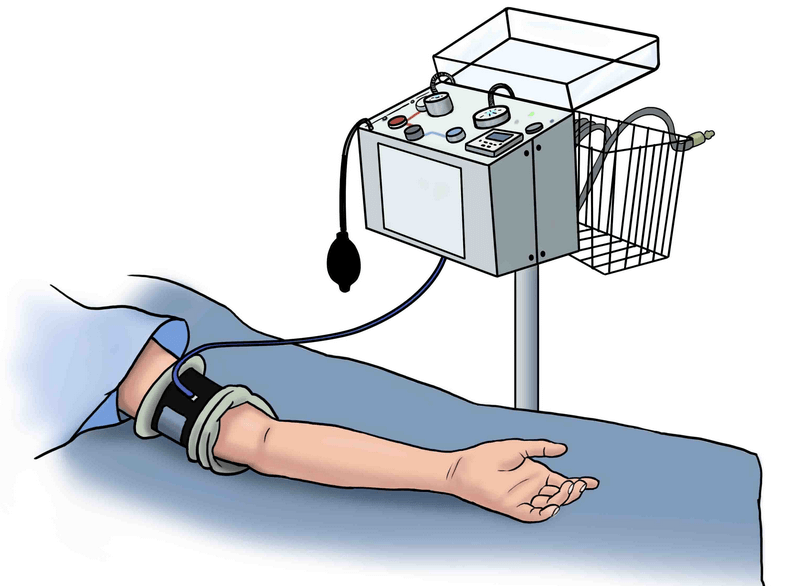
Synonym: Pressure paralysis
Mechanism: Direct extrinsic pressure (displacement of ranvier node) or axonal hypoxia on the nerves beneath the tourniquet and are related to the cuff pressure and duration of application.\
It is different from post tourniquet syndrome which caused due to combined effect of muscle ischemia, edema and microvascular congestion due to reactive hyperemia (to maintain acid-base balance) and return of blood following release of tourniquet leading to stiff, pale, weak, numb limbs.
Characteristics:
Distal to the site of application of the tourniquet, there are disturbances in the function of one or all of the nerves. The constellation of signs are:
1. Motor paralysis with hypotonia or atonia but without appreciable atrophy.
2. Evidence of sensory dissociation:
- Touch, pressure, vibration and position sense are usually absent.
- Pain sensation is never lost (there may be delay in pain recognition in severe cases) and hyperalgesia is usually present.
- Temperature sensation is usually not affected.
- Paresthesia is absent (block of touch fibers). Tinel sign and Neuroma sign are absent.
The affected functions would correspond most likely to the larger fibers described by Erlanger and Gasser, the A fibers. The larger fibers would consequently collapse before the smaller ones. If the damage is severer, the fast or first pain fibers and some of the fibers conveying cold sensation can to some extent be impaired. As a rule they are not involved in the tourniquet syndrome.
3. Sympathetic fibers are not affected.
4. Color and temperature of skin are normal.
5. All peripheral pulses are present.
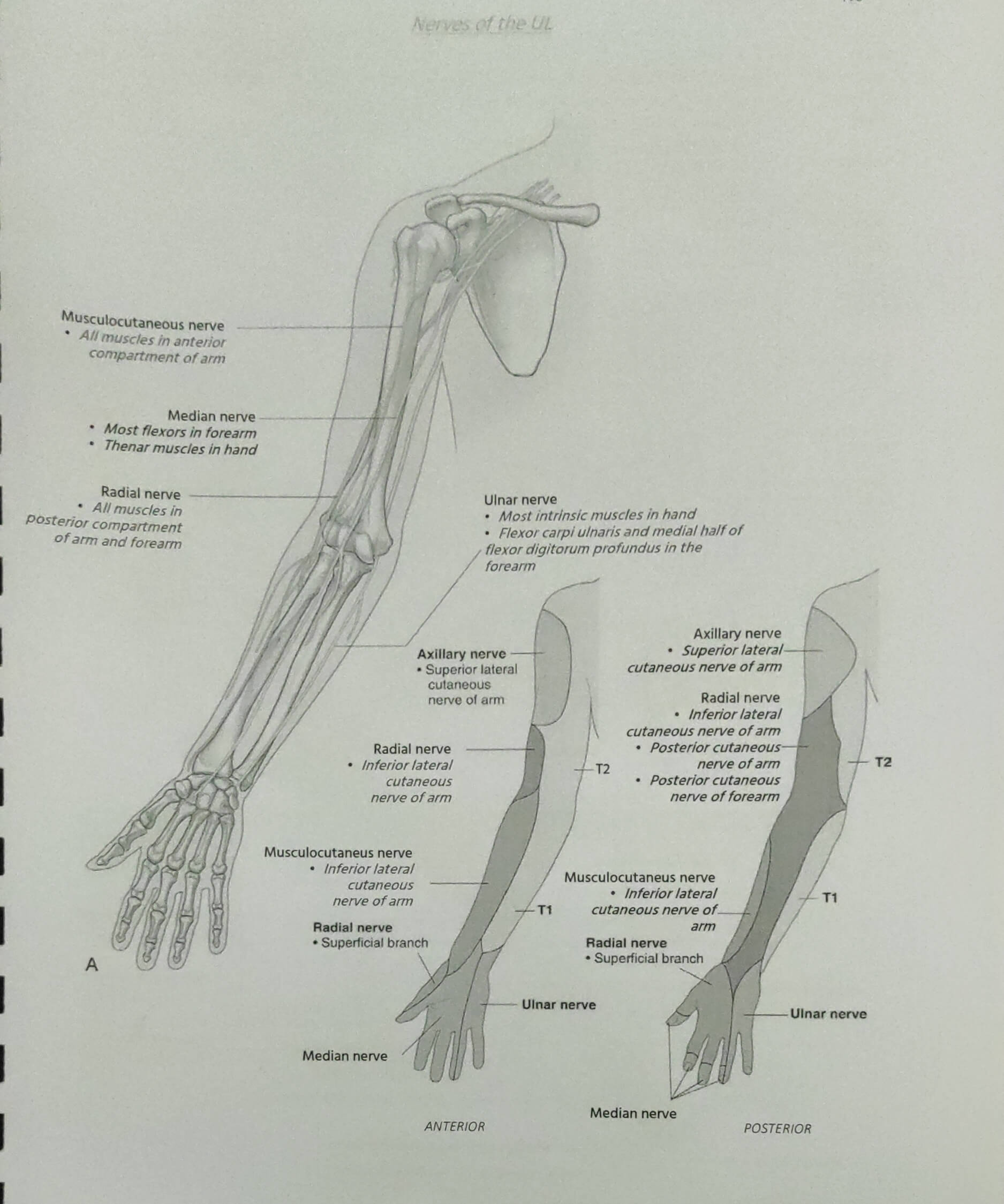
Most commonly involved nerves:
- Upper limb: Radial nerve > Ulnar nerve > Median nerve
- Lower limb: Sciatic nerve
Reference: MOLDAVER J. TOURNIQUET PARALYSIS SYNDROME. AMA Arch Surg. 1954;68(2):136–144. doi:10.1001/archsurg.1954.01260050138002