Approach to a limping child
General points
- Translation of metaphysis anteriorly and superiorly in relation of the epiphysis
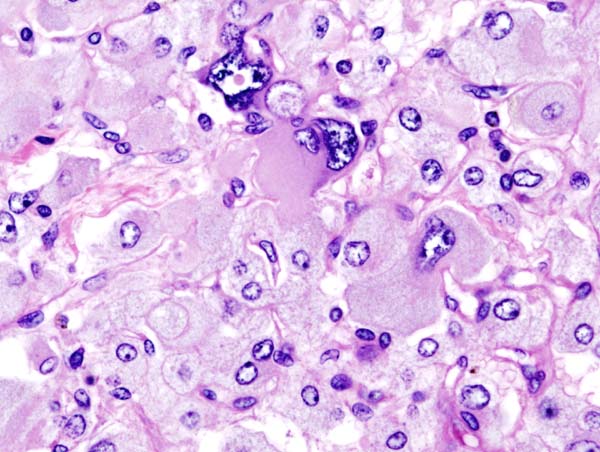
- Slip occurs through the hypertrophic zone due to weakening perichondral ring of La-corix (progresses from infancy through adolescence) and propensity of mamillary processes to unlock with widening of physis
- Incidence: 1 in 10,000
- Age: 10-15 years
- M:F ratio = 3:2 (estrogen narrows physis and increases physeal strength, while testosterone widens physis and reduces physeal strength)
- Obesity is associated with relative femoral neck retroversion which is associated with reduced neck-shaft angle which increases the shear stress across the physis
- Associated with increased physeal obliquity: More vertical physis increases shear force across the physis
Classification
Management depends on 4 factors which can be remembered using the mnemonic SCFE.
- Stability and Severity
- Seniority (<10 years and open triradiate cartilage = higher risk of bilateral slip)
- Chronicity
- Fat (higher risk of bilateral slip in obese)
- Etiology (higher risk of bilateral slip in endocrinopathies, metabolic diseases and radiation therapy compared to idiopathic cause)
Stability and Severity
a. Loder classification:
- Stable: Able to bear weight with or without crutches
- Unstable: Unable to bear weight with or without crutches
b. Severity:
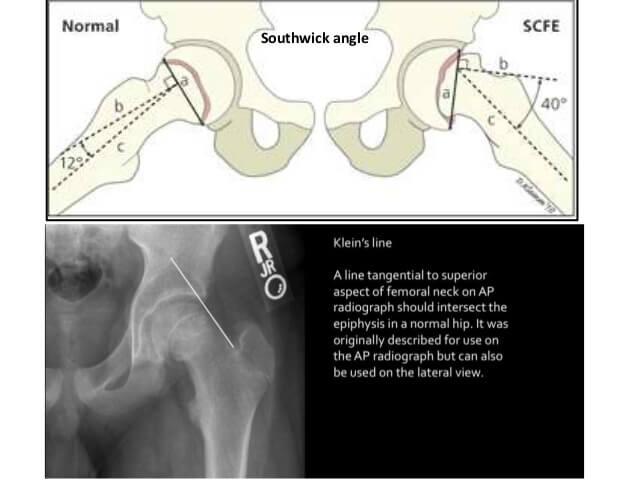
| Severity | Southwick angle on frog-leg lateral view (Difference of head-shaft angle from normal side) | Wilson slip % on AP or frog-leg lateral view (% of epiphyseal displacement in relation to metaphysis) |
| Mild | <30° | <33% or 1/3 |
| Moderate | 30-50° | 33-50% (1/3-1/2) |
| Severe | >50° | >50% (>1/2) |
Chronicity:
| Classification | Duration of symptoms | History | Physical findings | Radiographic findings |
| Pre-slip | Variable, usually <3 weeks | Limp, weakness, pain worse with exertion | Antalgic gait ↓ Internal rotation | Osteopenia of hemipelvis Wide/irregular physis |
| Acute | <3 weeks | Unable to bear weight, severe pain | Unable to ambulate External rotation deformity LLD ↓ Motion secondary to pain | Trethowan’s sign Steel’s sign Slip angle on frog-leg view |
| Chronic | > 3 weeks | Groin, thigh, knee pain (referred from medial obturator nerve); limp | Antalgic gait ↓Internal rotation ↓ Abduction LLD | Metaphyseal remodeling: Posterior/inferior sclerosis Superior/anterior resorption |
| Obligate external rotation and flexion with hip flexion (Drehmann’s sign) | Pistol-grip deformity | |||
| Acute on chronic | Acute increase in baseline symptoms | Acute increase in baseline symptoms | ↓ Motion secondary to pain Antalgic gait ↓ Internal rotation ↓ Abduction LLD External rotation with flexion | Combination of acute and chronic changes |
- Preslip: symptomatic hip with evidence of physiolysis prior to true movement of the femoral neck relative to the femoral head
- Acute: Symptoms <3 weeks
- Chronic: Symptoms >3 weeks
- Acute on chronic: Abrupt increase in symptoms with a preceding prodrome of nonspecific pain
Management
1. General measures: Complete avoidance of weightbearing until the slip is stabilized (Bed rest + Traction)
2. Stable SCFE:
- Any severity of slip:
- In-situ fixation with single cannulated screw:
- Single screw vs multiple screw: Single screw provides satisfactory stability with lower risk of AVN and chondrolysis
- Center-center position in the epiphysis in both the AP and lateral view
- Start on anterior surface of neck and must be perpendicular to physis and not parallel to the neck
- Atleast 5 threads must purchase the epiphysis
- Threads are placed on either side (prevent redisplacement and prevent growth)
- Newer techniques: Allow growth of physis and remodeling
- Modalities: Smooth wires, Growing screws, Proximally threaded screws
- Advantage: Remodeling may improve or resolve the impingement lesion between metaphysis and acetabulum
- Disadvantage: Risk of slip progression (epiphysis “grows off” the transfixion device)
- Bone graft epiphysiodesis:
- Not preferred due to higher incidence of slip progression and higher morbidity of open surgery
- In-situ fixation with single cannulated screw:
- Severe slip:
- Consider Ganz surgical hip dislocation and Dunn osteotomy (severe slip are unlikely to remodel even with growth preservation)
- Intertrochanteric osteotomy after physeal closure (if opted for correction of malalignment)
- Postoperative rehabilitation:
- Toe-touch weight bearing for several days until full weight bearing tolerated
- Remove screws when physis closed (not necessary) and followup until physis fuses
3. Unstable SCFE:
- 2 school of thoughts: Emergent/urgent surgery (quickly restore circulation) vs Delayed treatment (prevent second hit phenomenon)
- Gentle repositioning and Fixation with 1-2 cannulated screws (preferably 2)
- Phillips technique of gentle repositioning: Position the patient on OT table with gentle traction with position of the limb –
- Internal rotation: 15-20°
- Abduction: 20-30°
- Phillips technique of gentle repositioning: Position the patient on OT table with gentle traction with position of the limb –
- Ganz surgical hip dislocation and Dunn osteotomy
- Postoperative rehabilitation: Non-weight bearing crutch walk on affected limb for 6-8 weeks to prevent slip progression
4. Risk of Bilateral slip: Consider contralateral hip prophylactic pinning
- Metachronous slip: 15-35% with unilateral slip develop a contralateral slip within 18 months of presentation
5. Pain on sitting caused by impingement with hip flexion: Femoral neck osteoplasty (removal of prominent antero-superior femoral neck)
Ganz surgical hip dislocation:
- Vessel enters the joint capsule between the gemellus superior and the piriformis muscles
- Interval: Piriformis and Posterior border of gluteus minimus (to avoid blood supply to femoral head)
- Trochanteric flip osteotomy, Z-capsulotomy
- Flex, externally rotate and adduct the hip to dislocate
- Modified dunn osteotomy to reduce epiphysis
Proximal femoral osteotomies:
- Osteotomy close to physis allows greater correction but has higher risk of AVN
- Subcapital osteotomy is contraindicated if the physis is closed
Mnemonic: CKS
- Subcapital: Cuneiform (Fish or Dunn)
- Open excision of callus and physeal cartilage with anterior based wedge osteotomy of neck to relax the blood vessel
- Posterior periosteum left intact to protect lateral epiphyseal vessels
- Fish osteotomy: Similar with complete removal of physis from both the metaphysis and epiphysis (allows bone-on-bone apposition)
- Basicervical: Krammer
- Degree of reduction limited to 35-55° and high risk of leg length discrepancy
- Intertrochanteric: Southwick
- Goals: Flexion, valgus and internal rotation (to increase range of motion and reduce impingement)
X-ray features
Mnemonic: CKS
1. Capener’s sign (AP X-ray): Entire metaphysis is lateral to posterior acetabular margin (loss of capner’s triangular double density sign created by overlap of proximal metaphysis and posterior acetabulum)
2. Klein’s line (AP X-ray): A line drawn along the superior border of the neck should intersect the epiphysis
- Trethowan’s sign: Klien’s line is flush with or below the epiphysis (>2 mm difference from unaffected side must arouse suspicion for SCFE)
3. Steel’s metaphyseal blanch sign (AP X-ray): Crescent double density created by overlap of posteriorly displaced epiphysis over metaphysis
4. Others: Widened physis (epiphysiolysis), Southwick’s angle, Wilson’s slip grade
Complications
Mnemonic: ABCDEF
- AVN: unstable slip is the most accurate predictor (47% vs 10% in stable slip)
- Breakthrough slip (progression): occurs in upto 2% cases with in-situ fixation
- Chondrolysis: associated with inadvertent pin penetration into the joint
- Degenerative joint disease: pistol grip deformity of proximal femur
- Enlargement of femoral head (Coxa magna)
- Fractures: can occur just distal to knowles pins (so must be removed once physis fused) or stress fracture due to over-reaming of neck
References:
- Rathi, R. A., & Khan, T. (2016). Slipped upper femoral epiphysis. Orthopaedics and Trauma, 30(6), 482–491. doi:10.1016/j.mporth.2016.08.002
- Apley and Solomon’s system of Orthopaedics, 10th Edition
- Paediatric Orthopaedics – A system of decision making, 2nd Edition

He is the section editor of Orthopedics in Epomedicine. He searches for and share simpler ways to make complicated medical topics simple. He also loves writing poetry, listening and playing music. He is currently pursuing Fellowship in Hip, Pelvi-acetabulum and Arthroplasty at B&B Hospital.