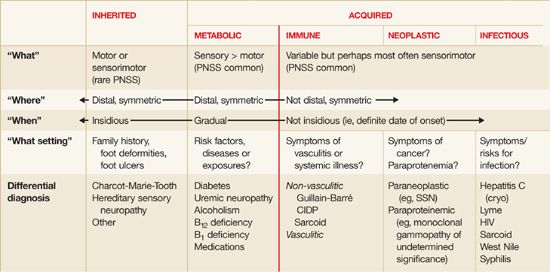
Step 1: What system is involved – motor, sensory, autonomic or mixed?
a. Sensory involvement
- Positive neuropathic sensory symptoms (PNSS) – suggest Acquired polyneuropathy
- prickling, tingling, asleep like numbness
- Pain – suggest Small fiber neuropathy due to toxic, metabolic, ischemic or idiopathic cause
- electric shock, burning, freezing, tightness, throbbing, allodynia (discomfort or pain to apparently painless stimuli), hyperalgesia (exaggerated pain response)
- often accompanied by reduced or absent sensation of pinprick or temperature
- Negative neuropathic sensory symptoms – suggest acquired or inherited cause
- loss of sensation, imbalance
Sensory examination:
1. Sensation: Begin distally at toes or fingertips – move proximally if abnormal
- Vibration: 128 Hz tuning fork
- Pinprick: Disposable safety pin
- Light touch: Cotton swab
- Temperature: Warming or cooling tuning fork’s prongs
2. Joint position sense: Ask patient to close eyes – then, move distal phalanx of toes or finger up or down by small increments and ask the patient to tell the direction of movement
3. Casual and tandem gait: for unsteadiness or ataxia
b. Motor involvement:
Often combined with sensory symptoms:
- Motor symptoms > Sensory symptoms: Immune-mediated like AIDP (Gullian-Barre Syndrome), CIDP
- Sensory symptoms > Motor symptoms: In many other polyneuropathies especially length-dependent neuropathies caused by metabolic or toxic disorders
c. Autonomic involvement:
Symptoms include – lightheadedness, syncope, diarrhea, constipation, postprandial bloating, early satiety, urinary complaints, erectile dysfunction, abnormal or absent sweating, dry mouth and eyes
Tests:
- Pre-syncopal symptoms: Bedside orthostatics or tilt-table testing
- Early satiety or postpradnial bloating: Gastric emptying test
Commonly acquired polyneuropathies with autonomic invovlement:
- Diabetic neuropathy
- Amyloid neuropathy
- AIDP (Guillain-Barre syndrome)
- Paraneoplastic neuropathy (Small cell lung cancer)
- Sjogren’s syndrome associated neuropathy
- HIV
- Vincristine
- Porphyria
- Pandysautonomia
Step 2: Where – distribution of nerve involvement ?
a. Distal (length-dependent) and symmetric: Metabolic, toxic, inherited or idiopathic
b. Not length-dependent and asymmetric: immune-mediated or infectious
- Motor neuropathies (ALS)
- Sensory neuropathies (Paraneoplastic syndrome)
- Demyelinating disease (AIDP, CIDP)
- Mononeuritis complex (Vasculitis)
Step 3: When – onset and course ?
- Acute (<1 month) and Subacute (1-2 months): Immune-mediated or Infectious process
- Chronic (>2 month): Inherited, metabolic, toxic or idiopathic
Step 4: What setting – review of comorbidities and medications?
Common causes of acquired polyneuropathies:
- Diabetes mellitus
- Chronic kidney disease
- Alcohol dependence
- Vitamin B1 and B12 deficiency
Positive family history of: high arched foot or hammer toes – Charcot Marie Tooth (CMT) Disease i.e. Hereditary Sensory and Motor Neuropathy
Step 5: Electrodiagnostic test
- Define – distribution and extent of neuropathy
- Differentiate – axonal and demyelinating or mixed process
- Limitation – normal in small fibre neuropathy (skin biopsy is helpful in these cases)
Step 6: Blood tests
a. For distal symmetric neuropathy:
- Fasting glucose or 2 hour oral glucose tolerance test: Diabetes and impaired glucose tolerance (pre-diabetes)
- Serum protein electrophoresis: Paraproteinemias
- Demyelinating: MGUS i.e. Monoclonal Gammopathy of Undetermined Significance, Waldenstorm’s macroglobulinemia, Osteosclerotic myeloma
- Axonal: Amyloidosis, Mixed cryoglobulinemia
- RFT, Electrolytes, Calcium, Phosphorous: Uremic neuropathy
- Hepatitis C titer: usually asymmetric and as mononeuritis complex, but sometimes as distal and symmetric
- Serum B12 level
b. Specific:
- Metabolic/toxic:
- Elevated MCV: alcoholism, vitamin B12 deficiency
- Thiamine deficiency: alcoholism, bariatric surgery
- Urine heavy metals: Heavy metal intoxication
- Thyroid function tests: Hypothyroid neuropathy (rare)
- Inflammatory:
- CBC: mononeuritis complex
- Markers or vasculitis or systemic inflammation (ESR, ANCA, RF, ANA, cryoglobulins): Vasculitis, Cryoglobulinemic neuropathy (Hepatitis C)
- CSF: protein elevation in AIDP and CIDP
- Neoplastic/Paraneoplastic:
- Paraneoplastic serology: especially subacute and severe neuropathy in smokers
- Chest X-ray and other imaging for cancers: Small cell lung cancer and other malignancies
- CSF cytology: carcinomatous or lymphomatous polyradiculopathy
- Infections:
- CSF: pleocytosis
- Lyme titres (serum, CSF): Lyme neuroborreliosis
- HIV testing: HIV associated neuropathy
- Hepatitis C (Cryoglobulin testing): Hepatitis C – mixed cryoglobulinemia
Summary