Embryology and Development of Prostate Gland
- Time: During 3rd month of gestation
- Fetal testosterone is converted by 5α-reductase into 5α-Dihydrotestosterone (DHT).
- This hormone stimulates urogenital sinus mesenchyme, which in turn stimulates formation of prostatic buds (endodermal outhgrowths) from posterior urogenital sinus epithelium.
- Prostatic buds invade into urogenital sinus mesenchyme.
- Differentiation:
- Prostatic bud: Prostate glandular epithelium
- Inner (central) zone glands develop later
- Outer (peripheral) zone glands develop earlier
- Mesenchyme: Prostatic stroma
- Paired outgrowths from spongy part of urethra: Bulbourethral glands
- Prostatic bud: Prostate glandular epithelium
Size, Shape and Relations of Prostate Gland
Normal adult size: Often compared to the size of a walnut or chestnut (~20-25 grams and 4X2X3 cm)
Shape of prostate: Prostate is conical in shape with:
- Base
- Apex
- Anterior surface
- Posterior surface
- 2 Lateral surfaces
Relations of Prostate:
- Superior: Base of prostate lies against the bladder neck
- Inferior: Apex of prostate lies against the urogenital diaphragm
- Anterior: Extraperitoneal fat in Retzius space (retropubic space) which separates prostate from pucbic symphysis
- Posterior: Denovillier’s fascia which separates prostate from rectal ampulla
- Lateral: Levator ani
Lobar Anatomy of Prostate
The prostatic urethra and the ejaculatory ducts divide prostate into 5 different lobes.
- Anterior lobe:
- Anterior to urethra
- Devoid of glandular tissue
- Posterior lobe:
- Posterior to urethra and Below the ejaculatory ducts
- Palpable during DRE (Digital Rectal Examination)
- Median or Middle lobe:
- Between urethra and ejaculatory ducts
- It’s upper part is related to the bladder trigone.
- Lateral lobes:
- Separated from eachother by prostatic urethra
- Continuous posteriorly except a shallow vertical groove which separates the 2 lateral lobes
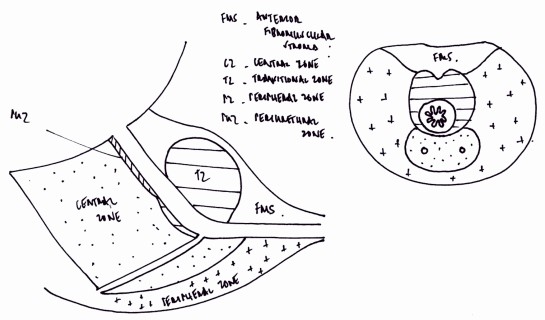
Zonal Anatomy of Prostate
McNeal 1 used urethra as a reference point and divided prostate into 4 zones.
- Peripheral zone (70% of glandular prostate): lateral to urethra and distal to the verumontanum. Almost all carcinomas arise here.
- Central zone (25% of the glandular prostate): surrounds the ejaculatory ducts all the way to the verumontanum
- Transition zone (5% of glandular prostate): surrounds the urethra between bladder neck and colliculus. It is the exclusive site of nodular hyperplasia (BPH) origin.
- Anterior fibromuscular stroma: nonglandular portion
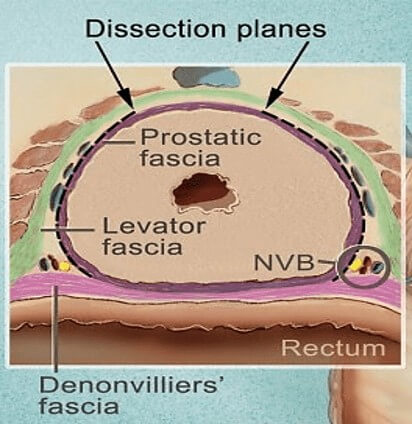
Capsular Anatomy of Prostate
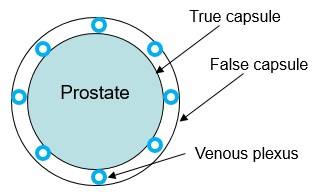
True capsule:
- Outer condensed fibromuscular band inseparable from prostatic stroma is referred to in the literature as prostate “capsule”.
- Important boundary for staging locally aggressive prostate cancer (i.e. extraprostatic extension [EPE]).
- This capsule is absent at prostate base and is not clearly defined at the apex, thus assessment of EPE is not amenable at these 2 sites.
False capsule:
- Visceral layer of pelvic fascia forms a fibrous prostatic sheath outside the true capsule.
Prostatic venous plexus lies between the true and false capsule.
Surgical or Pathological capsule:
- In BPH, normal peripheral parts of the gland becomes compressed into a capsule around this enlarging mass.
Functions of the Prostate
1. Prostatic secretion: The prostatic fluid is thin, slightly acidic (pH 6.4) and forms about 20% of semen volume. It contains: spermine (for the motility of sperms), spermidine, prostataglandins (for uterus stimulation), zinc (affects testosterone metabolism of the prostate), citric acid (buffer), immunoglobulins, phosphatases and proteases (sperm liquefaction).
2. Control of urine or semen flow: Prostate acts like a valve – preventing urine flow during ejaculation and permitting urine flow in between.
- Parasympathetic activity: relaxation of bladder neck and micturition (peeing)
- Sympathetic activity: activation of alpha-receptors lead to contraction of smooth muscle stroma of bladder neck leading to expulsion of contents and closure of bladder neck for anterograde ejaculation.
- Injury of sympathetic nerve leads to retrograde ejaculation
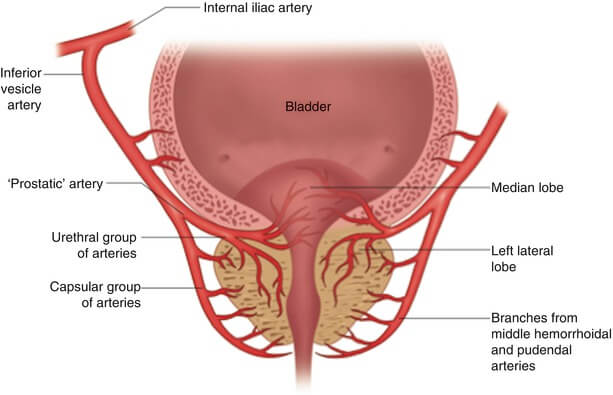
Vascular Anatomy of Prostate
Arterial Supply
Major: Prostatic arteries arising from the Inferior vesical artery
- Urethral branches: urethral branches perforate the basal prostate and bladder neck at 4 and 8 clock and supply the transition zone. Bleeding due to TURP or Adenomectomy are therefore expected at the bladder neck at the 4 and 8 clock position.
- Capsular branches
Additional: Branches from middle rectal artery and Internal pudendal artery
Venous Drainage
- Veins form the prostatic venous plexus which lies between the true and false capsule
- Prostatic plexus receives deep dorsal vein of penis and vesical veins to form vesico-prostatic plexus which drains into internal iliac veins.
- The plexus is valveless and also connected posteriorly to the Internal vertebral venous plexus by Batson’s plexus.
Lymph Drainage
Internal iliac nodes
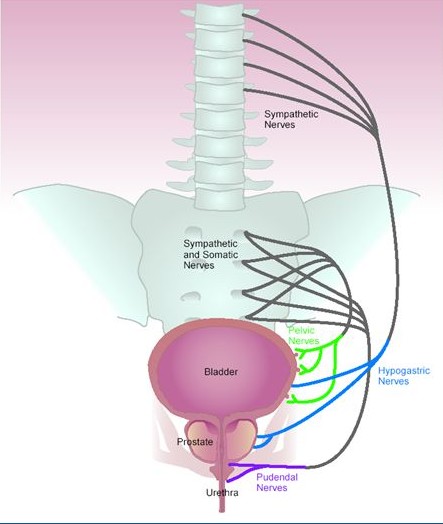
Neural Anatomy of Prostate (Cavernous nerves)
Parasympathetic innervation: hypogastric and pelvic nerves
Sympathetic innervation: peripheral hypogastric ganglion
The neurovascular bundles (NVB) run posterolaterally between the: prostatic capsule, levator fascia and denovillier’s fascia
Prostate Histology

References
- Snell Clinical Anatomy
- Urology-Textbook.com