The Sepsis-2 definition used SIRS criteria and the term “Severe sepsis” which has been recently eliminated by the Sepsis-3. The new sepsis definitions recommend using a change in baseline of the total SOFA score of two or more points to represent organ dysfunction.
New Definition of Sepsis and Septic Shock
According to the new guidelines by Sepsis-3 task force in 2016, sepsis is no longer defined by non-specific SIRS criteria and the focus has been shifted to the pathophysiology of host’s response and related organ dysfunction. The new definition relies on Sequential Organ Failure Assessment (SOFA) score.
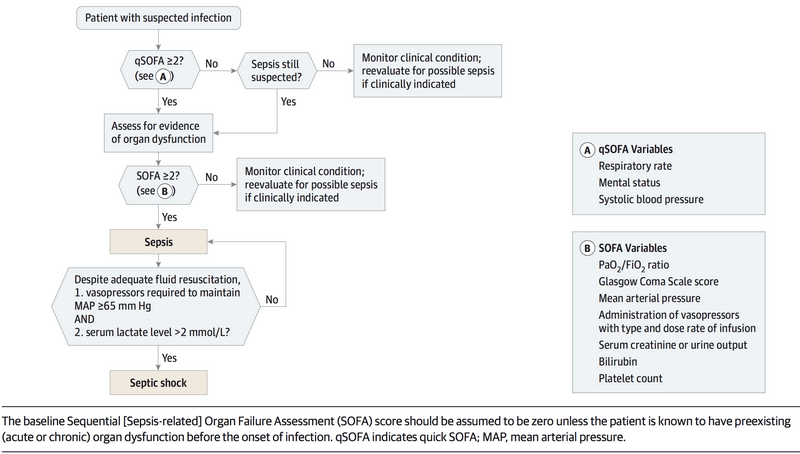
Sepsis-3 task force 1 defines sepsis as the presence of suspected infection along with rise in total SOFA score ≥2 from baseline. Surviving Sepsis Campaign has clarified 2 that qSOFA (quick SOFA) does not define sepsis, but the presence of 2 qSOFA criteria is a predictor of both increased mortality and ICU stays of more than 3 days in non-ICU patients. It may also be used as an initial screening tool to lay out foundation for total SOFA assessment.
qSOFA includes 3 components that are often represented by a mnemonic “HAT“. 2 findings out of 3 is considered significant. It includes:
- Hypotension i.e. Systolic Blood Pressure ≤ 100 mmHg
- Altered mental status (any GCS < 15)
- Tachypnea (Respiratory rate > 22/min).
Septic shock is now defined as sepsis and (despite adequate volume resuscitation) both of: persistent hypotension requiring vasopressors to maintain Mean Arterial Pressure (MAP) greater than or equal to 65 mm Hg, and lactate greater than or equal to 2 mmol/L. The use of the term “severe sepsis” has been abandoned.
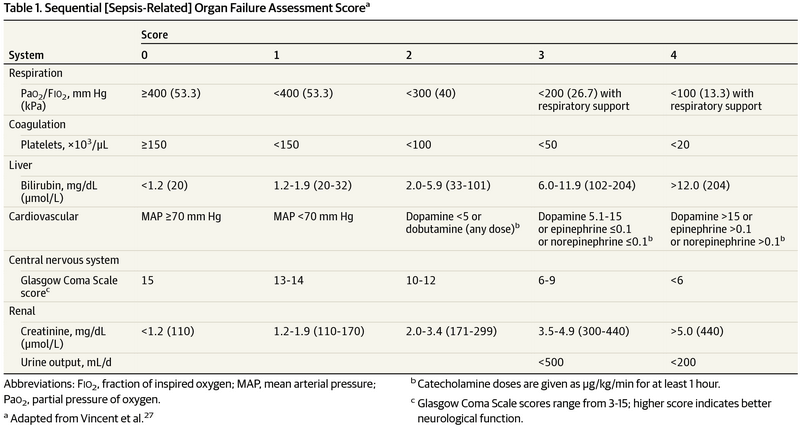
Let us look at the variables to be assessed in SOFA score in a system-wise fashion:
- Brain (CNS): Glassgow Comas Scale (GCS)
- Lungs (Respiratory system): PaO2/FiO2
- Heart (Cardiovascular system): Mean Arterial Pressure (MAP) and vasopressor dosing
- Liver: Bilirubin
- Kidneys: Creatinine and Urine output
Problem with using SIRS to define Sepsis
SIRS, Sepsis, Severe sepsis and Septic shock represented growing severity along a continuous spectrum previously.
A study conducted by Kaukonen et.al. 3 found that SIRS criterion was neither specific nor sensitive to sepsis. In their study, the incidence of SIRS negative sepsis was around 12%. In patients with SIRS-negative severe sepsis, the most frequent single criterion that was met was an abnormal white-cell count, followed by an increased heart rate and increased respiratory rate or a low PaCO2. Of the patients with SIRS-negative sepsis, 20% did not fulfill any SIRS criteria, and 80% fulfilled one SIRS criterion.
Jaimes F et.al 4 concluded that SIRS criteria exhibited a sensitivity of 69%, specificity of 35%, positive predictive value (PPV) of 90%, negative predictive value (NPV) of 12% and positive LR of 1.06.
The problem with the specificity of SIRS is that 2 criteria of SIRS is often easily met in Emergency setting and their presence along with minor infection doesn’t necessarily indicate life-threatening nature of infection.
Criticism about new definitions of sepsis
Since, SOFA and qSOFA are mortality indicators, they may be less specific for infection than the SIRS was. Check out other criticisms of new sepsis defintion at Pulmcirt.