5 components
a. Central aponeurosis
It is triangular in shape with apex originating at the level of flexor retinaculum as a continuation of palmaris longus and thins and fans out distally. It has 3 dimensional fiber orientation: longitudinal, transverse and vertical
1. Longitudinal: Gives 4 pre-tendinous band (PTB) in the hollow of the hand and divides into 3 layers –
- Superficial: Attaches to palmar skin (dermis) via Grapow vertical fibers
- Middle (spiral band of Gosset): Passes dorsal to natatory ligament and neurovascular bundle which becomes lateral digital sheet in fingers
- Deep (perforating fibers): Adheres to the MCP joint, flexor and extensor sheet via McGrouther fibers
2. Transverse: Links the longitudinal bands –
- At distal palmar crease: Superficial transverse palmar ligament or Transverse ligament of Palmar aponeurosis (TLPA or Skoog’s ligament)
- Usually not affected by Dupuytren’s disease
- Continues as Proximal commissural ligament of radial aponeurosis
- At the level metacarpal head and neck, gives origin to septa of Legueu and Juvara (vertical)
- Neurovascular bundles are dorsal to it
- Many advocate preserving this ligament during fasciectomy
- At web spaces: Superficial transverse metacarpal ligament or Natatory ligament
- Digital nerves and vessels pass dorsal to natatory ligament
- Continues as Distal commissural ligament of radial aponeurosis
- Normally tightens as the finger abducts (contracture leads to loss of abduction)
- Coalesces with the lateral cord (contracture leads to PIP joint contracture)
3. Vertical:
- Grapow vertical fibers: Connect superifical layer of pretendinous band to palmar dermis
- Septa of Legueu and Juvara: Arises from superficial transverse palmar ligament
- 8 septa form 7 fibro-osseous compartments:
- 4 for paired FDP and FDS tendons
- 3 for common digital NV bundles and associated lumbricals
- 8 septa form 7 fibro-osseous compartments:
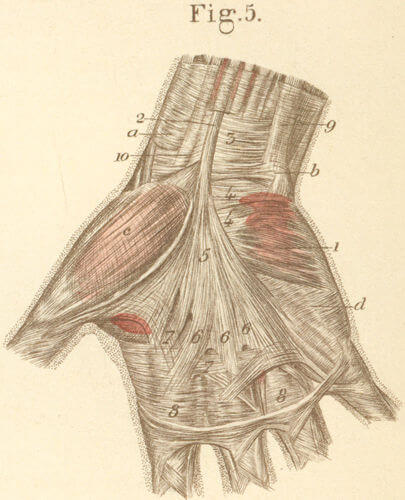
b. Radial or Thenar aponeurosis
It consists of:
- Thenar muscle fascia
- Pretendinous band of thumb (longitudinal)
- Proximal commissural ligament equivalent to Skoog’s ligament (transverse)
- Dorsal commissural ligament equivalent to Natatory ligament (transverse)
c. Ulnar or Hypothenar aponeurosis
It consists of:
- Hypothenar muscle fascia
- Pretendinous band of little finger
- ADM soft tissue confluence
- Pisiform ligamentous complex
d. Palmodigital fascia
- Natatory ligament
- Spiral band of Gosset (middle layer of pretendinous band): Contributes to formation of lateral digital sheath (LDS)
e. Digital fascia
The neurovascular bundles are surrounded by 4 ligaments:
- Lateral digital sheath (LDS) of Gosset laterally: continuation of spiral band and natatory ligament
- Grayson’s ligaments volarly: from flexor sheath to skin
- Thomine retrovascular fibers medially
- Cleland’s ligament dorsally: from phalanges to skin (typically spared in Dupuytren’s disease)
Mnemonic: Put your hands facing palm downwards –
1. Grayson: to the Ground (volar)
2. Cleland: to the Ceiling (dorsal)
3. Thomine: to the Thenar (medial)
4. Lateral: obviously lateral
Pathoanatomy in Dupuytren’s disease
In Dupuytren’s disease, normal fibrous bands are transformed into pathologic contracted cords leading to joint and soft tissue contractures.
a. Micro-cords (Grapow vertical fibers) → Skin thickening mimicking callus (one of the earliest manifestation)
b. Dermal cord (Superficial layer of PTB) → Skin pitting
c. Pretendinous cords (Pretendinous band or PTB) → MCP joint contracture
d. Vertical cords (Vertical septa of Legueu and Juvara) → Stenosing tenosynovitis (painful trigger finger)
e. Commissural ligament cord (Proximal or Distal) and Natatory cord → Webspace contracture
f. Isolated digital cord (ADM coalescence) → PIP joint contracture
g. Spiral cord (Spiral band or SB) → PIP and MCP joint flexion contracture
- Spiral cord components in digits = PTB + SB + LDS + Grayson’s ligament
- As they contract, they cause Neurovascular bundles to spiral medially and superficially (spiral nerve and artery) increasing the risk of iatrogenic neurovascular injury (Skin incisions must be made through the dermis and not onto the cord)
h. Central cord (Deep layer of PTB) → PIP joint flexion contracture
i. Lateral cord (LDS) → PIP joint flexion contracture
j. Retrovascular cord (Thomine’s retrovascular fibers) → PIP +/- DIP joint flexion contracture