Features of Osteochondroma
Mnemonic: Six “C”
- Commonest benign bone tumor
- Continue to grow until Closure of physis
- Cartilage cap (appears larger clinically than in X-ray)
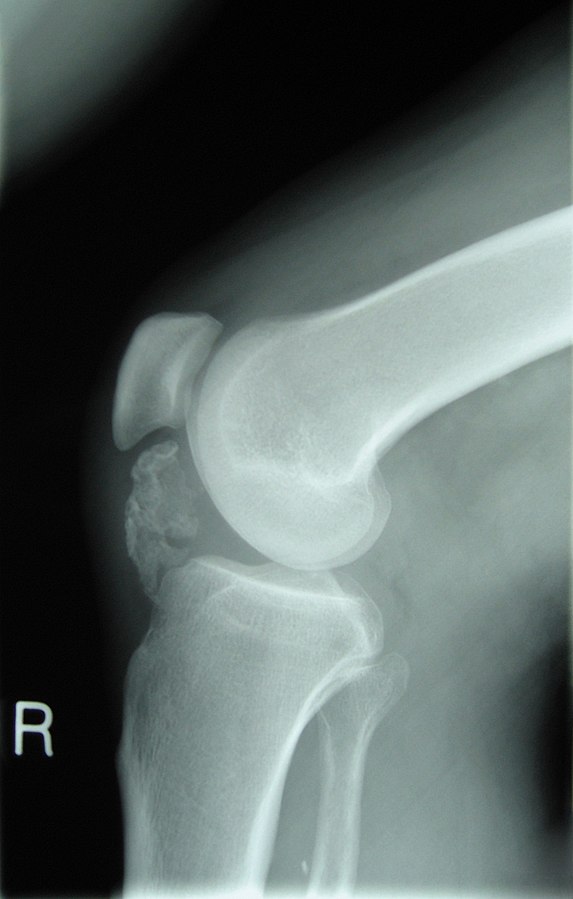
- Continuous with native bone (cortex and medullary canal)
- Cane (pedunculated/stalked points away from joint and sessile/broad based have higher risk of malignant degeneration)
- Change (mutation) in EXT1, EXT2 and EXT3 genes
Complications
Mnemonic: ABCDE
- Adventitious bursa (pain)
- Breakage of stalk (pain)
- Chondrosarcoma (pain; risk: 1% in solitary osteochondroma and 10% in multiple osteochondroma)
- Deformities:
- Femoral shortening
- Coxa valga
- Genu valgum, Ankle valgus (because of shortened fibula)
- Patellar dislocation
- Ulnar shortening, radial bowing and ulnar deviation of hand
- Radial head dislocation
- Encroachment:
- Nerve compression (sciatic, common peroneal, radial)
- Pseudoaneurysm (popliteal artery)
- Tendon (rotator cuff impingement, subscapularis tear, bicipital tendinitis)
Common locations
Mnemonic: FGH
- Femur (proximal)
- Genu (knee)
- Humerus (proximal)
- Hallux (subungual)
Risk factors for Malignant transformation
Mnemonic: GLAD PaST
- Growth after skeletal maturity
- Lucency (new)
- Additional scintigraphic activity
- Destruction (cortical)
- Pain after puberty
- Soft tissue mass
- Thickened cartilage cap >1.5 cm
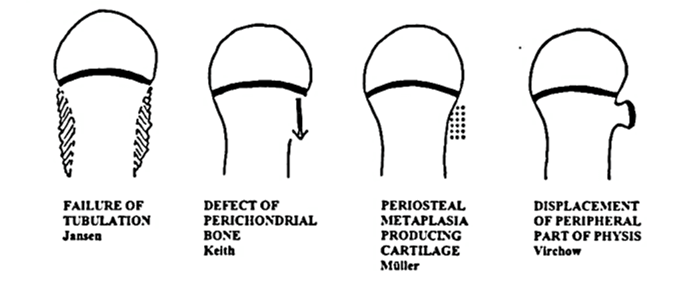
Pathogenesis theories
Mnemonic: Five “P”
1. Bone defect
- Perichondral bone defect and (Keith)
2. Cartilaginous metaplasia
- Periosteal metaplasia in periphyseal-perimetaphyseal area producing cartilage (Muller)
3. Displacement of physis
- Peripheral part of physis displacement (Virchow)
4. Epiphysis retains chondrogenic potential
- Pathological retainment of chondrogenic properties by the epiphysis that would form perichondral bone of the groove of ranvier (Langenskiold)
5. Failure of tubulation
- Prominent metaphysis suggesting tubulation failure (Jansen)

He is the section editor of Orthopedics in Epomedicine. He searches for and share simpler ways to make complicated medical topics simple. He also loves writing poetry, listening and playing music. He is currently pursuing Fellowship in Hip, Pelvi-acetabulum and Arthroplasty at B&B Hospital.