Acute pancreatitis along with case based discussion has been already covered earlier here:
To remember the initial management of acute pancreatitis, one can remember the mnemonics given below:
iPA-NCREAS (Ye et.al.)
Investigations:
- Imaging (CT, MRI or Ultrasonography)
- Prognostic screen to identify severe pancreatitis
- Amylase and lipase levels
Initial treatment:
- Nutritional support
- Cholecystectomy if suspected/proven gallstone pancreatitis
- Resuscitation of fluids
- ERCP within 72 hours of pain onset if gallstone pancreatitis
- Antibiotics
- Supplemental oxygen
Another acronym mnemonic based approach has been discussed by Khaliq et.al.
PANCREAS
- Perfusion:
- Fluid resuscitation to maintain urine output 0.5-1 ml/kg/hr
- Oxygenation in order to maintain SpO2 >95% in severe pancreatitis
- Analgesia: including opioids
- Nutrition: Enteral feeding within 48 hours (+/- nasojejunal feeding)
- Clinical: Prognostic scoring e.g. BISAP, RANSON, APACHE-II
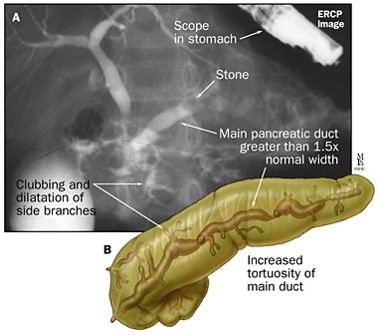
- Radiology:
- USG: to detect gallstones, choledocholithiasis and local complications
- CECT: after 48-72 hours of pain onset to determine degree and extent of necrosis
- Percutaneous catheter drainage guided by USG or CECT is helpful in management of necrosis and as bridging therapy until surgical management
- ERCP: with 72 hours if cholangitis or severe acute pancreatitis with persistent obstruction
- Antibiotics: Empirical antibiotics if infection is suspected
- Surgery: for –
- MODS with necrosis unresponsive to conservative management and percutaneous drainage
- Pseudo-aneurysm of surrounding vessels with bleeding
- Infected necrosis
- Pancreatic abscess
- Bowel perforation