Definition
- Cobb’s angle >10°
- Diagnosis of exclusion: Congenital scoliosis and Neuromuscular scoliosis ruled out
- Types:
- Early onset (<10 years):
- Infantile: 0-3 years
- Juvenile: 4-10 years
- Late onset (>10 years)
- Adolescent: 10-18 years
- Adult: >18 years
- Early onset (<10 years):
Indications for MRI in general
Mnemonic: Left JAPAN
- Left thoracic curves
- Juvenile onset (<10 years)
- Apical thoracic hypokyphosis
- Painful and Progressive curves
- Anomalies (Congenital abnormalities)
- Neurological signs or symptoms
Management
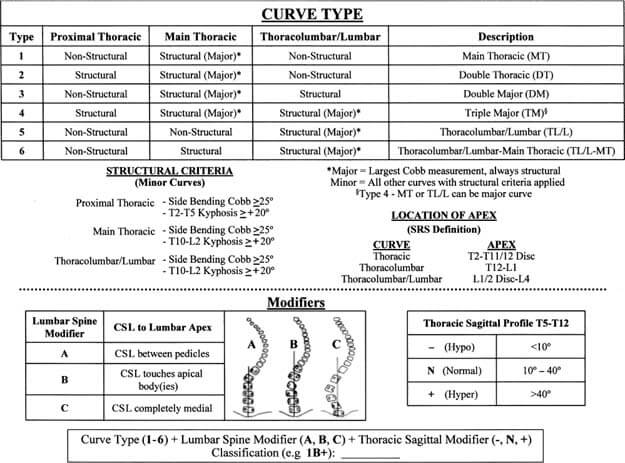
| Cobb’s angle (Curve magnitude) | Risser 0/Premenarchal/ Before TRC closure/ PHV (Olecranon closure) | Risser 1-2 | Risser 3-5 |
| <25 degrees | Observation (every 3-4 months) | Observation (every 4-6 months) | Observation (longer interval e.g., every 6 months) |
| Orthosis if: 1. Infantile scoliosis: RVAD >20°, Rib phase 2, 2 curves (double curves) 2. Documented progression in curves >20°: ≥5° in 2 consecutive visits or ≥10° in single visit | Orthosis if: Documented progression | ||
| 25-45 degrees | Orthosis | Orthosis (begin at 30°) | Observation (yearly standing PA radiographs for 2-3 years after skeletal maturity, then every 5 years) |
| >45 degrees | Operation | Operation | Operation (when curve >50°) |
Risser sign and Growth
A simple mnemonic can be used:
- Risser 1 to 5 lasts about 2 years
- At Risser 1, there is further 4 cm remaining of increase in sitting height
- At Risser 2, there is 3 cm
- At Risser 3, there is 2 cm
- At Risser 4, there is 1 cm
Mnemonic: Risser Stage + Remaining increase in sitting height (in cm) = 5
Reference: Spinal Anatomy – Modern Concepts edited by Jean Marc Vital, Derek Thomas Cawley
Orthosis
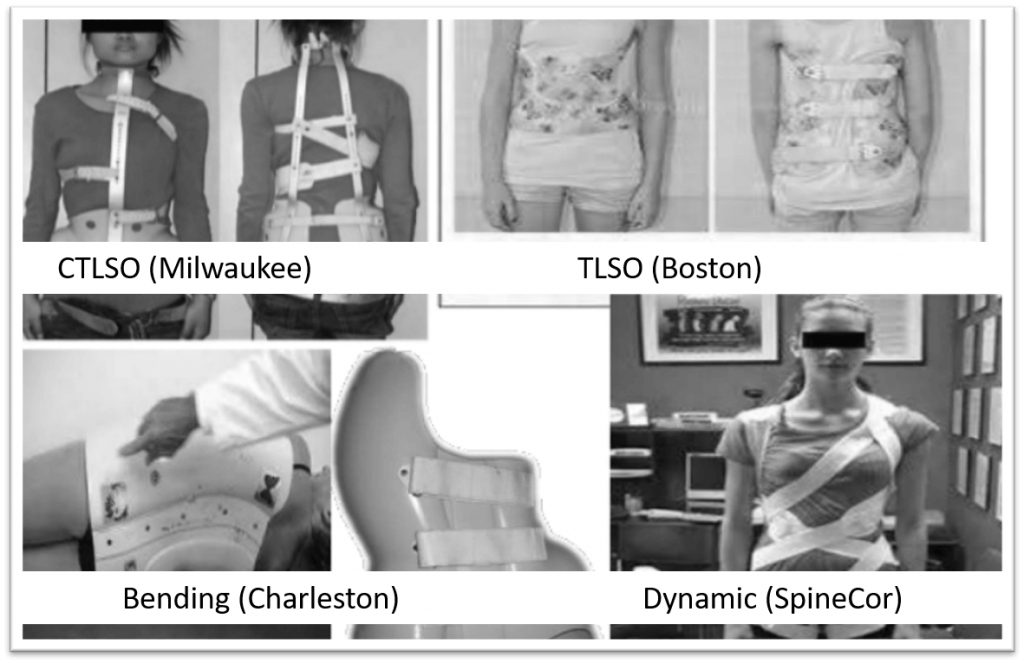
Types:
- Apex at T6 and above: CTLSO (Milwaukee brace)
- Apex at T7 and below: TLSO (Boston underarm brace)
- Infantile scoliosis: Elongation-derotation-flexion (EDF) or Mehta casts under GA (changed every 2-4 months; until deformity resolves or until child is big enough to manage in brace)
- Bending brace: Charleston brace (night-time bracing in maximal side-bending correction; reserved for single lumbar or thoracolumbar curves <35°)
- Flexible brace: Spine-Cor brace
Bracing is ineffective in: Thoracic hypokyphosis or lordosis
Protocol: Full-time bracing (23 hr/day) is more effective than Part-time bracing (16 hr/day or 8 hr/day); effectiveness is dose-dependent
Mechanism: Doesn’t correct scoliosis but prevents progression
In-brace radiograph after 2-4 weeks of application to verify amount of correction achieved:
- Boston brace: minimum 40-50% correction must be achieved
- Charleston brace: about 90% for flexible curves and 70% for rigid curves
Continue bracing if curve progression controlled:
- Girls: Upto 18-24 months post-menarchal and Risser 4 and Height growth stops
- Boys: Upto Risser 5
Operation
Indications:
- Curve magnitude as above in table
- Failure of orthosis: to control pain and/or progression of curve
- Thoracic lordosis or hypokyphosis (orthosis could exacerbate the rib deformity)
- Significant cosmetic deformity
Modalities:
- <8-10 years:
- Magnetic growing rods
- Dual growing rods (lengthened via open procedure every 6 months)
- VEPTR (Vertebral Expanding Titanium Prosthetic Rib): corrects spine by acting on ribs
- Shilla procedure: Fusion of apical vertebra via locked pedicle screw + Non-locked pedicle screws at the end of curve (can slide along the rods)
- 9-10 years: Combined anterior and posterior fusion to prevent risk of crankshaft phenomenon (preferrable over Growing rods)
- >10 years:
- Posterior instrumentation and fusion preferred
- Anterior instrumentation and fusion:
- Alone: Single TL/L fusion (Lenke 5), Single thoracic fusion (if hypokyphosis and if fusion levels can be saved)
- With posterior instrumentation and fusion: Open triradiate cartilage (to prevent crankshaft phenomenon), Large or stiff curves >75° (to improve flexibility)
- Fusion levels:
- Must include structural curves
- Must include non-structural curves that are:
- >45°
- Associated with significant rotation and translation
- Upper Instrumented Vertebra (UIV) to T2 (higher) when:
- Left shoulder is elevated in common right thoracic curve (fusion of MT curve only leads to further elevation of left shoulder and is suitable in neutral or elevated right shoulder)
- T1 tilt >5°
- Structural proximal thoracic curve
- Lower Instrumented Vertebra (LIV):
- Lenke 1 and 2:
- A modifier: Vertebra touched by CSVL unless L4 is titled to right
- B modifier: Stable vertebra (most proximal lower thoracic or lumbar vertebra most closely bisected by CSVL)
- Lenke 3-6: Distal end vertebra
- Lenke 1 and 2:
| Lenke type | Description | Structural regions recommended for fusion | Approach |
| 1 | Main thoracic | MT | PSF or ASF |
| 2 | Double thoracic | PT, MT | PSF |
| 3 | Double major | MT-TL/L | PSF |
| 4 | Triple major | PT, MT, TL/L | PSF |
| 5 | Thoracolumbar/lumbar | TL/L | ASF or PSF |
| 6 | Thoracolumbar/lumbar, main thoracic | TL/L, MT | PSF |
References:
- Rothman Simeone – The Spine
- Tachdjian’s Pediatric Orthopedics, 5th Edition
- Paediatric Orthopaedics, A system of Decision making, 2nd edition
- Miller’s Review of Orthopedics, 8th edition
- Kotwicki T, Chowanska J, Kinel E, Czaprowski D, Tomaszewski M, Janusz P. Optimal management of idiopathic scoliosis in adolescence. Adolesc Health Med Ther. 2013 Jul 23;4:59-73. doi: 10.2147/AHMT.S32088. PMID: 24600296; PMCID: PMC3912852.

He is the section editor of Orthopedics in Epomedicine. He searches for and share simpler ways to make complicated medical topics simple. He also loves writing poetry, listening and playing music.