HISTORY
1. General Information:
- Name:
- Age/Gender:
- Address:
- Source of history: Patient/Relative/Carer
2. Chief complaints:
- Complaint X Duration
- Chronological order
- Maximum 4-5
- Should include all major symptoms (important for making hypothesis)
- Duration should be specific rather than time interval (e.g. 10 days instead of 1-2 weeks)
- Chief complaints can be included in retrospect
Example:
Lower abdominal pain X 2 days
Nausea and vomiting X 1 day
3. History of Presenting Illness:
“OPQRST” for each symptoms
- Onset (acute, insidious, chronic)
- Provocative/Palliative and Progression
- Quality and/or Quantity
- Region and Radiation
- Severity
- Timing and Temporal relationships
- Others:
- Duration and Frequency
- Any diurnal variation
- Associated symptoms
- Last meal and Tetanus status
Negative history:
- Red-flag symptoms
- Ruling out differentials
- Probable etiology
- Severity and complications
Treatment received for the complaint
Review of systems: may or may not be related to chief complaint – include only positive finding
Add for females
Menstrual and Obstetric History:
• LMP
• Duration of flow/Cycle Length
• Clots passage, Average number of pads soaked, Dysmenorrhea
• GxPxAxLx – mode, indication and time
• ContraceptivesAdd for pediatric patients
• Birth history
- Any antenatal/natal/postnatal complications
- At birth – gestational age, mode of delivery, weight
• Development history: Gross motor/Fine motor/Language/Social
- Development of this __ months old child matches the chronological age in all 4 spheres of development. OR if delayed
- Development of this __ months old child in the __ area corresponds to a chronological age of between __ to __ months.
Nutritional history
- 24 hour dietary recall
Immunization history
- Are immunizations up to date? If not – why?
4. Past history:
- HTN, DM, TB or any prolonged illness (duration; treated/untreated)
- Surgeries with indication and time
- Hospitalizations with indication and time
5. Personal history:
- Smoking
- Alcohol
- Drug abuse
Eliciting smoking and alcohol history
6. Family history:
History of 2-3 generations for similar disease or related disease, hypertension or diabetes mellitus.
7. Drug and Allergy history:
- Prescribed drugs and other medications
- Compliance
- Allergies and reaction
Physical Examination
General examination:
G/C – Note relevant findings and abnormalities in –
Mnemonic: ABCDEF
- Appearance
- Built
- Consciousness
- Decubitus
- Environment
- Facies
Vitals –
- Temp:
- PR:
- RR:
- BP:
- SpO2:
- CRT (if applicable)
- Bedside GRBS (if applicable)
Pallor, Icterus, Lymphadenopathy, Clubbing, Cyanosis, Edema, Dehydration:
- Mention positive findings
- Characterize positive finding if applicable
- Grade positive finding if applicable
GCS and pupils – if applicable
Local examination: Of hypothetically involved system (present in detail)
P/A:
• Any abnormalities on inspection incl. hernia orifices and external genitalia
• Tenderness/Guarding/Rigidity
• Organomegaly
• Costovertebral angle tenderness
• Percussion – if ascites (shifting dullness/fluid thrill)
• Bowel sounds or other added sounds
• P/R and P/V findings (if applicable)
Chest:
• Any abnormalities in RR, Shape, Movement or use of accessory muscles
• Any abnormalities in tracheal position, chest expansion, vocal fremitus or tenderness
• Hyper-resonant/Resonant/Woody dullness/Stony dullness – location
• Vesicular/Bronchial/Broncho-vesicular – location if abnormal
• Wheeze/Crackles/Other added sounds – location
• Vocal resonance
CVS:
• Any abnormalities in shape or visible pulsation
• Apex beat – location and any abnormality
• Left parasternal heave/thrills
• S1 S2 – any abnormality
• Murmur
• Location (A, P, T or M)
• Systolic/Diastolic
• Grading
• JVP and HJ reflex (if relevant clinically)
CNS:
• Higher mental functions: note only abnormalities
• Cranial nerves: note only abnormalities
• Motor system: note any abnormality; grade power of relevant muscles
• Reflexes: note any abnormality; compare and grade relevant DTR
• Sensory: light touch, superficial pain, temperature, vibration, joint position sense, stereognosis/graphesthesia
• Cerebellar signs: mention if any sign present
• Signs of meningeal irritation: mention if any sign present
Skin lesions:
• Morphology:
• Primary: Macule/Papule/Plaque/Nodule/Abscess/Wheal/Petechia/Purpura/Telangiectasia/Cyst/Milia/Burrow
• Secondary: Scale/Erosion/Ulcer/Fissure/Excoriation/Scar
• Shape and configuration
• Distribution
• Single or Multiple
• Color
• Edge
Joints and Spine:
• Look: SEAD (Swelling/Erythema/Atrophy/Deformity)
• Feel: Skin to bones and joints – note temperature, tenderness, swellings
• Move: Active and Passive ROM
• Measure: Motor, Sensory and Circulation status
• Special tests: e.g. SLRT, Scaphoid test, Talar tilt test, Tests for knee ligaments, etc.
Ear:
• External ear
• EAC
• TM
• Hearing test
Nose:
• External nose
• Nasal mucosa and discharge
Throat:
• Oral cavity
• Tonsils
• Posterior pharyngeal wall
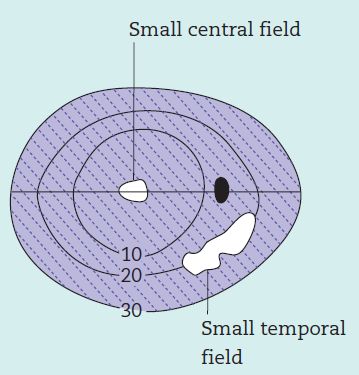
Eye:
• Visual acuity
• Orbit and adnexal structures
• Ocular movements
• Pupil – Size, shape, symmetry, reflex
• Conjunctiva
• Cornea
• Digital tonometry
System examination: Other than that mentioned in local examination (mention only abnormal findings)
If normal – mention as following:
• Chest: B/L NVBS, no added sounds
• CVS: S1S2 M0
• P/A: soft, non-tender, BS+
• CNS: grossly intact
Diagnoses
Provisional Diagnosis
Differential Diagnoses
1.
2.
3.
Management and Advice (Including investigations)
1.
2.
3.
4.
5.
For details about procedure and eliciting specific history and examination: Clinical skills

He is the section editor of Orthopedics in Epomedicine. He searches for and share simpler ways to make complicated medical topics simple. He also loves writing poetry, listening and playing music. He is currently pursuing Fellowship in Hip, Pelvi-acetabulum and Arthroplasty at B&B Hospital.


Thank you.
thank you
very important