DEFINITION OF CARDIAC FAILURE
It is a state in which there is:
a. Forward failure: inability of heart to maintain cardiac output sufficient to meet the metabolic demands of peripheral tissues AND/OR
b. Backward failure: ability to do so with elevated filling pressure
PATHOGENESIS OF CARDIAC FAILURE
1. Myocyte loss and/or dysfunction:
a. Myocyte loss:
- Necrosis: MI, Cardiotoxic drugs
- Apoptosis: Elevated catecholamines, angiotensin II, inflammatory cytokines, mechanical strain from increased wall stress
b. Myocyte dysfunction (Changes in expression of contractile proteins, ion channels, enzymes, receptors and secondary messengers):
- Reduced cellular ability to maintain calcium homeostasis
- Changes in handling of high-energy phosphates
2. Compensatory mechanisms:
a. Increased myocardial contractility:
- Frank-Starling law: Within physiological limits, the force of contraction is proportional to initial length of cardiac muscle fibre (end diastolic fibre length) i.e. beyond the limit of stretch-ability of myocytes, instead of increase in contractility – the contractility diminishes.
- In cardiac failure: Decreased stroke volume → Increased diastolic → Increased contractility → Increased cardiac output
b. Myocardial hypertrophy:
- By Laplace’s law: Wall stress = (Ventricular pressure X Ventricular chamber radius)/2 times Ventricular wall thickness (i.e. PXR/2h)
- In cardiac failure: Sustained increase in pressure and chamber radius (dilation) → Increased wall stress → Hypertrophy of myocytes → Increased cardiac output
c. Neurohumoral mechanisms:
- Renin-Angiotensin-Aldosterone-System (RAAS): Angiotensin II causes –
- Vasoconstriction: Increases total peripheral resistance
- Stimulation of thirst at hypothalamus: Increases intravascular volume and preload
- Increases Aldosterone secretion at adrenal cortex: Increases water retention via sodium resorption
- Anti-Diuretic Hormone (Vasopressin):
- Increased by arterial baroreceptors (detecting decreased CO) and angiotensin II
- Promotes water reabsorption in distal collecting tubule (increases preload)
d. Sympathetic stimulation:
- Decreased perfusion pressure is sensed by baroreceptors in carotid sinus and aortic arch
- Central and peripheral chemoreflex activation induces epinephrine, norepinephrine and vasopressin release – leading to increased sympathetic outflow to heart and peripheral vessels while decreasing parasympathetic tone:
- Heart: Increased heart rate and contractility (CO = HR X SV)
- Peripheral vasoconstriction: Venous (Increased preload); Arteriolar (Raised peripheral resistance)
DELETERIOUS EFFECTS OF PROLONGED COMPENSATORY MECHANISM
1. Continuous sympathetic activation: β-adrenergic downregulation and desensitization (less inotropic response)
2. Increased heart rate: Increased metabolic demands and myocardial cell death
3. Increased circulating volume and preload: Beyond limits of Starling’s law, pressure is transmitted to pulmonary vasculature leading to alveolar exudation and pulmonary congestion
4. Increased total peripheral resistance: Higher afterload leading to decreased stroke volume and cardiac output
5. Continuous neurohumoral activation: Chronically elevated angiotensin-II and aldosterone trigger production of cytokines, which stimulate macrophages and stimulate fibroblasts resulting in myocardial remodelling which leads to loss of contractility.
PRECIPITATING AND AGGRAVATING FACTORS OF CARDIAC FAILURE
1. Increased metabolic demands (like your company is already in loss and your workers ask for more salary):
- Fever
- Infection
- Anemia
- Pregnancy
- Tachyarrhythmia
- Hyperthyroidism
- Emotional and physical stress
2. Increased preload (when the Starling’s law is overwhelmed – increased ventricular filling pressure leads to transmission of pressure back to systemic veins from right side leading to systemic venous congestion and to pulmonary vasculature from left side leading to pulmonary congestion):
- Excess salt intake
- Excessive fluid administration
- Renal failure
3. Increased afterload (increased resistance against which the ventricles must pump leading to reduced stroke volume):
- Uncontrolled hypertension (left side)
- Pulmonary embolism (right side)
4. Impaired contractility (reduces stroke volume and cardiac output):
- Negative inotropic medications: Beta-blockers, Calcium channel blockers
- Supervening heart disease: Ischemia, Myocarditis, Infective endocarditis
5. Direct drop in cardiac output:
- Bradyarrhythmias
6. Poor compliance with therapy
Mnemonic: FAILURE
- F: Forget to take medications
- A: Arrhythmias, Anemia
- I: Infection, Ischemia, Infarction
- L: Lifestyle changes
- U: Upregulators (thyroid, pregnancy)
- R: Rheumatic heart disease and other valvular disease
- E: Embolism
TYPES OF CARDIAC FAILURE
A) Systolic Vs Diastolic Heart Failure:
1. Systolic heart failure: Impaired contraction (LVEF <40%)
- Ischemic heart disease
- Modifiable: Smoking, Hyperlipidemia, Hypertension, Diabetes mellitus, Sedentary lifestyle and obesity
- Non-modifiable: Family history of premature CAD (Men <55 yrs and Women <65 years), Age (Men >45 years and Women >55 years), Genetic factors
- Dilated cardiomyopathy: Mnemonic – ABCDEFGHI
- Alcohol abuse (>90 g/day for several years)
- Beriberi
- Cyclophosphamide, Cocaine, Coxscakie/Chaga’s myocarditis
- Diabetes mellitus, Doxorubicin
- Endocrine (hypothyroidism and hyperthyroidism)
- Familial (friedrich’s ataxia, muscular dystrophies)
- Glycogen storage diseases, Gestational i.e. Peripartum (within last month of pregnancy to 6 months of delivery; without demonstrable cause of heart failure and heart disease before last month of pregnancy; with documented systolic dysfunction)
- Hemochromatosis (infiltrative)
- Idiopathic
2. Diastolic heart failure: Impaired filling (diastolic dysfunction) and normal systolic function (LVEF >40%) e.g.
- Hypertension
- Essential hypertension (85%)
- Secondary hypertension:
- Alcohol
- Obesity
- Pre-eclampsia
- Renal – Glomerular (Glomerulonephritis), Vascular (RAS), Polycystic kidney disease, CKD
- Endocrine – Pheochromocytoma, Cushing syndrome, Conn’s syndrome, Hyperparathyroidism, Hyperthyroidism, Acromegaly, Congenital adrenal hyperplasia, Primary hypothyroidism
- Drugs – OCPs, steroids, sympathomimetics
- Coarctation of aorta (associations – bicuspid aortic valve, berry aneurysms, turner’s syndrome, VSD, PDA)
- Restrictive/Obliterative cardiomyopathy: Mnemonic – PRIME
- Primary: Idiopathic
- Radiation
- Infiltrative: Amyloidosis, Sarcoidosis, Neoplasm, Hemochromatosis
- Metabolic: Glycogen storage disease, Fabry’s disease
- Endomyocardial fibrosis, Eosinophilic endomyocardial disease
- Hypertrophic cardiomyopathy (familial – autosomal dominant trait)
- Cardiac tamponade (minimum amount of fluid required depends upon speed of accumulation – 250 ml in rapidly developing effusions and 2000 ml in slowly developing effusions)
- Rheumatic fever
- Infections – TB, Viral (Coxscakie, Mumps, Varicella, EBV), Pyogenic, Fungal
- Collagen vascular disease – SLE, RA, Scleroderma
- Uremia
- Idiopathic
- Post-MI (Dressler’s syndrome)
- Post-traumatic
- Drugs (Anticoagulants, thrombolytics)
- Constrictive pericarditis (fibrosed, thickened and inelastic pericardium):
- Tuberculosis (commonest)
- Hemopericardium and cardiac surgery
- Mediastinal irradiation
- CVD – SLE, RA
- Uremia
- Asbestosis
B) Acute Vs Chronic Heart Failure:
1. Acute heart failure (sudden): Cardiogenic shock and Acute pulmonary edema without peripheral edema e.g. MI, rupture of cardiac valve
2. Chronic heart failure (insidious):
- Compensated: Compensatory mechanisms have prevented development of overt heart failure – precipitants may lead to decompensation
- Decompensated: Systemic arterial pressure is well maintained, but edema accumulates e.g. dilated cardiomyopathy, multivalvular disease
C) Low output vs High output failure:
1. Low output heart failure: Heart fails to generate adequate cardiac output or can do so with high filling pressures e.g. ischemic heart disease, hypertension, cardiomyopathy, valvular disease, pericardial disease
2. High output heart failure: Heart fails to maintain sufficient circulation despite increased cardiac output (>8 L/minute) or increased cardiac index (>3.9 L/minute/sq.m) e.g. hyperthyroidism, anemia, pregnancy, AV fistula, beriberi, etc.
- Mechanism: Peripheral vasodilation or systemic arteriolar shunting leading to fall in systolic BP and warm peripheries rather than cold.
D) Left-sided vs Right-sided heart failure:
1. Left-sided (left ventricular) failure (LVF): Reduction in left ventricular output, increase in left atrial pressure and increase in pulmonary venous pressure. e.g. Aortic stenosis
- Acute increase in left atrial pressure: Pulmonary congestion and edema
- Gradual increase in left atrial pressure: Pulmonary hypertension without pulmonary edema
2. Right-sided (right ventricular) failure (RVF): Reduction in left ventricular output, resulting in systemic venous congestion. e.g. Cor pulmonale, Pulmonary valvular stenosis, Multiple pulmonary emboli
Cor pulmonale: RV dilation +/- RV hypertrophy +/- overt RVF secondary to Pulmonary HTN resulting from:
- Diseases of lung: COPD, Chronic asthma, Pulmonary TB, ILD, Bronchiectasis, High altitude dwelling, Cystic fibrosis, Pleural fibrosis
- Diseases of pulmonary circulation: Recurrent pulmonary embolism, Primary pulmonary hypertension, Collagen vascular disease, Chronic liver disease
- Diseases of thorax: Kyphoscoliosis, Neuromuscular diseases, Sleep apnea syndrome, Pickwickan syndrome (Obesity-hypoventilation syndrome)
Pulmonary hypertension (PH): Mean pulmonary artery pressure >25 mmHg or Resting systolic pulmonary artery pressure >40 mmHg; Dana Point classification –
- I : Pulmonary artery hypertension (Cor pulmonale)
- II: Left heart disease
- III: Lung disease and/or hypoxia (Cor pulmonale)
- IV: Thromboembolic (Cor pulmonale)
- V: Unclear multiple mechanisms
3. Biventricular (Congestive) heart failure: Examples –
- Diseases affecting both ventricles: Dilated cardiomyopathy, Ischemic heart disease
- LVF leading to pulmonary hypertension and subsequent RVF
E) COMMON CAUSES OF HEART FAILURE
1. Pressure overload of ventricle:
- Systemic hypertension
- Pulmonary hypertension
2. Volume overload of ventricle:
- Increased metabolic demand
- Mitral and Aortic regurgitation
- Ventricular and Atrial Sepdal defect (VSD and ASD)
- Patent Ductus Arteriosus (PDA)
3. Inflow obstruction of ventricle:
- Mitral stenosis
- Tricuspid stenosis
- Endomyocardial fibrosis
4. Impaired ventricular function:
- Myocarditis
- Cardiomyopathy
- Myocardial infarction
Common causes of valvular heart diseases:
1. Mitral Stenosis (MS): Normal orifice 4-6 sq.cm; Mild 1.5-2.5 sq.cm; Moderate 1-1.4 sq.com; Severe/Critical/Tight <1 sq.cm
- Rheumatic fever (almost all cases)
- CVD: SLE, RA
- Rare causes (4 “M”s): Mucopolysaccharidosis, Myxoma (atrial), Malignant carcinoid, Methysergide
2. Mitral Regurgitation (MR):
- Rheumatic Heart Disease
- Ischemic (Papillary muscle dysfunction and rupture)
- Degenerative (Mitral valve prolapse)
- Infective (Endocarditis)
- Connective tissue disorder (SLE, RA, Marfan’s syndrome, Ehler-Danlos syndrome)
- LV dilation of any cause
- Congenital MR
3. Aortic Stenosis (AS): Normal orifice 3-4 sq.cm; Critical stenosis <0.8 sq.cm
- Valvular: Congenital, RHD, Aortic sclerosis, SLE, Infective endocarditis, Radiation
- Subvalvular: HOCM, Congenital
- Supravalvular: Congenital
4. Aortic Regurgitation (AR):
- Aortic valve disease: RHD, Congenital (bicuspid valve), Infective endocarditis, Trauma (rupture)
- Aortic disease: Aortitis (Syphilitic, CVD, Autoimmune vasculitis), Hypertension, Aneurysm
5. Tricuspid stenosis (TS):
- RHD
- Carcinoid syndrome
- Congenital
6. Tricuspid regurgitation (TR):
- Functional: RHD or CHD with severe PAH, Inferior wall MI, Corpulmonale, Cardiomyopathy
- Organic: RHD, Ebstein’s anomaly, Carcinoid syndrome, Tricuspid valve prolapse, Infective endocarditis, Trauma
6. Pulmonary stenosis (PS):
- Congenital (may be associated with maternal rubella syndrome)
- May be isolated or associated with Tetralogy of Fallot
PATHOPHYSIOLOGY AND CLINICAL FEATURES OF CARDIAC FAILURE
| Signs and symptoms | Underlying mechanism |
| Left-sided heart failure | |
| Symptoms | |
| Dyspnea | Backflow causes interstitial pulmonary edema, leading to:
|
| Orthopnea (dyspnea on lying supine; relieved by sitting) |
|
| Paroxysmal nocturnal dyspnea i.e. PND (awakens patient from sleep; persists even after sitting) | |
| Cough +/- frothy blood-tinged sputum | Pulmonary congestion Rupture of engorged bronchial veins – hemoptysis |
| Confusion and/or impaired memory or syncope e.g. Complete heart block (Stokes-Adams-Morgagni syndrome) | Cerebral hypoperfusion and arterial hypoxemia |
| Decreased urine output | Decreased renal perfusion during daytime leading to pre-renal AKI |
| Nocturia | Redistribution and better perfusion of kidneys at night when supine |
| Signs | |
| Pulmonary crackles | Opening of small airways closed by interstitial edema prior to inspiration; initially at lung bases (hydrostatic forces greatest) and later diffuse |
| Cardiac “asthma” | Wheezing caused by compression of conduction airways by pulmonary congestion – most prominent at night |
| Accentuated P2 | Pulmonary artery hypertension due to backflow of elevated left atrial pressure |
| Mitral regurgitation murmur | Excessive stretching of mitral valve annulus due to left ventricular dilation |
| Pulsus alternans | A sign of advanced ventricular dysfunction |
| Narrow pulse pressure | Reduced systolic BP due to reduced stroke volume Increased diastolic BP due to generalized vasoconstriction |
| Right-sided heart failure | |
| Symptoms | |
| Peripheral edema, sacral edema, ascites, effusions and/or anasarca | Increased hydrostatic venous pressures (in dependent parts) –
RAAS activation leading to salt and water retention |
| Congestive Hepatosplenomegaly (+/- RUQ pain) | Portal and splenic circulation engorgement Pain and tenderness is due to the stretching of capsule |
| Anorexia/weight loss | Diminished appetite due to hepatic and intestinal congestion Increased metabolism due to increased myocardial oxygen consumption and excessive work of breathing Intestinal fat malabsorption and protein losing enteropathy (rarely) |
| Signs | |
| Elevated JVP | Elevated right sided pressure Positive abdomino-jugilar reflex suggests inadequate ventricular compliance |
| Kussmaul sign | Paradoxical elevation of JVP with inspiration (as opposed to decrease) reflects increased right atrial pressure |
| Palpable right ventricular heave | Right ventricular hyperthrophy (RVH) |
| Tricuspid regurgitation murmur | Excessive stretching of tricuspid valve annulus due to right ventricular dilation |
| Right- or left-sided heart failure | |
| Symptoms | |
| Ischemic Chest pain/pressure a. Angina: retrosternal; exertional/emotional; <20 min; relieved by rest and GTN; radiating to left arm, jaw and backb. Myocardial infarction: similar to angina but >20 min; not relieved by GTN |
Primary myocardial ischemia: CAD
Secondary myocardial ischemia: increased filling pressures, poor cardiac output (with consequent poor coronary diastolic filling) or hypoxemia |
| Palpitations a. Extrasystoles: “Heart misses a beat; jumps” b. SVT/VT: “Heart flutters” c. AF: “Heart races irregularly” |
Sinus tachycardia due to decompensated heart failure Atrial/ventricular tachyarrhythmias arising in dilated heart chambers High cardiac output failure |
| Chronic fatigue/weakness | Chronic state of hypoxemia from inadequate oxygen delivery to peripheral tissues Generalized decreased muscle strength, decreased endurance and multi-organ system dysfunction |
| Cardiac Cachexia | Anorexia Gut congestion leading to decreased absoprtion Increased metabolic demands Immobility leading to skeletal muscle atrophy Increased chornic inflammatory markers |
| Signs | |
| S3 gallop (S1+S2+S3 = Triple rhythm) Sounds like “-Ken-tuck-y” |
Abnormal filling of dilated ventricle |
| S4 gallop (S1 S2+S4 = Triple rhythm; S1+S2+S3+S4 = Quadruple rhythm) | Forceful contraction of the atria into a stiffened ventricle; common in diastolic dysfunction |
| Cardiomegaly (Displaced apex beat) | Work hypertrophy and Volume dilation |
FRAMINGHAM CRITERIA FOR DIAGNOSIS OF CARDIAC FAILURE
Definite diagnosis requires: 2 Major OR 1 Major + 2 Minor criteria
A) Major Criteria:
Mnemonic: 3CDEFGH
- Crackles
- CVP raised (Neck vein distension)
- Cardiomegaly on Chest X-ray
- Dyspnea – PND
- Edematous lungs (Acute pulmonary edema)
- Fall of weight >4.5 kg in 5 days in response to CHF treatment
- Gallop rhythm (S3)
- Hepatojugular reflux positive
B) Minor Criteria:
Mnemonic: MNOPQRS
- Megaly of liver (Hepatomegaly)
- Night cough
- Oedema – bilateral ankle
- Pleural effusion
- Quantitative PFT – Vital capacity reduced by 1/3 of maximum
- Rapid pulse (tachycardia > 120/min)
- SOB on strain (sternous exertion)
AHA and NYHA CLASSIFICATION OF HEART FAILURE
| ACC/AHA grade | NYHA functional class |
| A: At risk of heart failure but without structural disease or symptoms | None |
| B: Structural heart disease but without heart failure | I: Asymptomatic HF – no limitations of daily activities |
| C: Structural heart disease with prior or current heart failure symptoms | II: Mild HF – symptomatic with moderate exertion |
| III: Moderate HF – symptomatic with minimal exertion | |
| D: Refractory heart failure requiring specialized interventions | IV: Severe HF – symptomatic at rest |
COMMON DIAGNOSTIC STUDIES FOR CARDIAC FAILURE
A) Chest X-ray Features of Pulmonary edema:
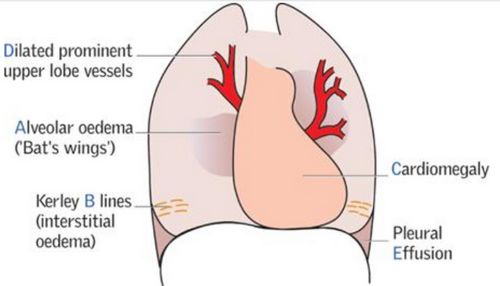
- Grade 1: Dilated prominent upper lobe veins (reverse moustache sign; stag antler’s sign)
- Grade 2: Interstitial edema (Kerley lines – “A” towards apex and “B” towards base; interstitial opacities)
- Grade 3: Alveolar edema (Bat’s wing; Bilateral fluffy lung shadows; Pleural effusions at uncommon sites – lamellar effusion. interlobar effusion/phantom/vanishing tumor, subpulmonic effusion)
B) ECG: Features of –
- Ventricular hypertrophy
- Atrial abnormality
- Arrhythmias
- Conduction abnormalities, previous MI and active ischemia
C) Echocardiography: Assessment of –
- Ejection fraction (Normal 50-70%)
- Valvular functions
- Chamber size and shape
- Differential systolic and diastolic dysfunction
D) Brain Natriuretic Peptide (BNP):
Origin: BNP is secreted by the cardiac ventricles in response to left ventricular stretching or wall tension. Cardiac myocytes secrete precursor pro-BNP which is secreted into ventrciles, where it is cleaved into biologically active C-terminal portion and biologically inactive N-terminal (NT pro-BNP) portion.
Functions of Natriuretic peptides (ANP and BNP):
- Downregulates sympathetic nervous system and RAAS
- Facilitates natriuresis and diuresis
- Increase smooth muscle relaxation and decrease peripheral resistance
Uses in heart failure:
- A negative result rules out disease more effectively than a positive result rules in disease
- Predictor of prognosis
- Monitoring
BNP levels:
- <100 pg/ml: Heart failure unlikely
- 100-250 pg/ml: Compensated heart failure
- 250-500 pg/ml: Both diastolic and systolic dysfunction
- 500-1000 pg/ml: Decompensated heart failure
- >1000 pg/ml: Increased risk of substantial heart failure
E) Others: RFT (look for renal dysfunction), CBC (look for anemia), Serum electrolytes (electrolyte imbalances) and TFT (thyroid dysfunction) because these may contribute to HF symptoms and progression.
- Cardiac biopsy: suspected acute myocarditis or infiltrative cardiomyopathy
History and physical examination should focus on distinguishing between ischemic causes of HF (coronary artery disease [CAD]) and nonischemic causes of HF (valvular heart disease, diabetes, hypertension, alcohol abuse, neuromuscular disorders, and cardiomyopathies). The family history should be explored for premature CAD, HF, arrhythmias, and sudden cardiac death.
The baseline ECG should be reviewed for evidence of myocardial infarction, conduction disturbances, and arrhythmias.
MANAGEMENT OF ACUTE DECOMPENSATION (ACUTE CARDIOGENIC PULMONARY EDEMA)
Pathophysiology of Cardiogenic Pulmonary Edema:
It is defined as an episode of acute heart failure accompanied by severe respiratory distress and oxygen saturation <90% on room air before all treatment.
- As pulmonary congestion increases, oxygen saturation decreases – decreased myocardial oxygen supply (risk of ischemia and further worsening of cardiac performance)
- Hypoxemia and increased fluid content in lungs induces pulmonary vasoconstriction increasing the right ventricular pressure – this compromises left ventricular function through ventricular interdependence mechanism (interventricular septum is common to both the ventricles)
- Circulatory insufficiency leads to metabolic acidosis – further impairs cardiac performance
Mnemonic: POD MAN
1. Precipitants: Find and treat it simultaenously
2. Position: Propped-up (raise the head of bed or use 2-4 pillows) or Sitting position
- Reduces venous return to heart and decreases preload
3. Oxygen +/- NIV: 100% Oxygen, preferably under positive airway pressure
- Oxygen: Reduces hypoxemia
- Positive airway pressure: Raises intra-alveolar pressure and reduces transudation of fluid (Non-invasive ventilation may be used if saturation remains <90% despite medical therapy) –
- CPAP (Initiate at 5-10 cm H2O): Set continious pressure throughout respiratory cycle, patient initiates all breaths
- Augments inspiratory and expiratory flow and pressure – increases tidal volume and unloads inspiratory muscles
- Decreases dead-space ventilation and improves alveolar ventilation – reexpands flooded alveoli
- During systole, increases intrathoracic pressure and reduces preload – improves mechanics of overloaded heart
- During diastole, increases pericardial pressure and reduces transmural pressure – decreases afterload
- BiPAP: Set higher inspiratory pressure (start 8-12 mmHg) and lower expiratory pressure (3-5 mmHg); can set up backup respiratory rates; patient initiates breath
- It has all benefits of CPAP plus:
- Unloads the respiratory muscles, reduces respiratory effort, and increases tidal volume before any changes in pulmonary mechanics (in contrast to CPAP in which it occurs after changes in pulmonary mechanics)
- CPAP (Initiate at 5-10 cm H2O): Set continious pressure throughout respiratory cycle, patient initiates all breaths
4. Diuretics:
Intravenous loop diuretics like:
- Furosemide/Lasix (40-100 mg) OR
- Ethacrynic acid (40-100 mg) OR
- Bumetanide (1 mg)
Mechnism of furosemide benefit:
- Within few minutes: Venodilator action reduces preload
- Within 30 minutes: Reduces circulating volume and preload
Avoid in hypertensive pulmonary edema – patient are euvolemic or hypovolemic
5. Morphine: 2-5 mg i.v. slowly
- Venodilator effect: reduces preload
- Anxiolytic and Analgesic effect: reduces sympathetic stimulation and reduces cardiac oxygen demand
6. Methylxanthines: I.V Aminophylline 250-500 mg reduces bronchoconstriction, increases renal blood flow and sodium excretion (by diuresis) and increases myocardial contractility
7. Adrenergic drugs (Inotropes):
Useful in hypotensive pulmonary edema or cardiogenic shock
- With normal or low-normal blood pressure: Dobutamine
- With shock: Dopamine
- With SVT: Digoxin
- Inodilators: Milrinone (risk of life-threatning arrhythmia), Levosimendan (novel calcium sensitizer)
8. Nitrates and Nesiritide (Vasodilators):
Mechanism: Venodilation reduces preload and Arteriolar dilation reduces afterload – both reduces overloading of heart
a. GTN infusion if SBP >110 or 2 Puffs GTN spray if SBP >90
- Initial dose: 10-20 mcg/min
- Increment as needed: 5 mcg/min every 3-5 minutes
b. Sublingual nitrates: 5-10 mg Isosorbide dinitrate
c. Nitroprusside (when acute afterload reduction needed – hypertensive emergency, acute aortic regurgitation, acute mitral regurgitation, acute VSD): 20-30 mcg/min
d. Nesiritide (recominant BNP): arterial and venous dilator + diuretic effect; i.v. 2 mcg/kg bolus followed by 0.01 mcg/kg/min infusion

Very comprehensive and easy to understand. Thank you.
God bless you….Keep the Good work
Very useful God bless you
Its very nice and organized ,,,easy to understand,thanks keep up