Author: Sulabh Kumar Shrestha, KISTMCTH
The “Red Death” had long devastated the country. No pestilence had ever been so fatal, or so hideous. Blood was its Avatar and its seal—the redness and the horror of blood. There were sharp pains, and sudden dizziness, and then profuse bleeding at the pores, with dissolution. The scarlet stains upon the body and especially upon the face of the victim, were the pest ban which shut him out from the aid and from the sympathy of his fellow-men. And the whole seizure, progress and termination of the disease, were the incidents of half an hour.
From “The Masque of Red Death” by Edgar Allan Poe
MICROBIOLOGY OF EBOLA VIRUS

Family: Filoviridae (Others – Marburg virus, Cuevavirus)
Shape: long filamentous or “U” or “6” shaped
5 species:
- Bundibugyo ebolavirus (BDBV)
- Zaire ebolavirus (EBO-Z) – Most dangerous
- Reston ebolavirus (EBO-R) – Non-pathogenic to humans
- Sudan ebolavirus (EBO-S)
- Tai forest ebolavirus (TAFV)
Important features:
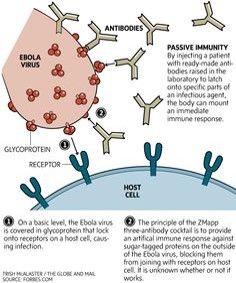
- Envelope glycoprotein – Binds to host cells
- Secreted glycoprotein –
- Cytotoxic
- Suppresses immune response
- Antibodies to glycoprotein may enhance infectivity
- VP40 – Cytotoxic
- VP35 – Interferon atagonist
BRIEF HISTORY OF EBOLA VIRUS
- Named after Ebola river in the Democratic Republic of Congo
- Early outbreak: 1st recognized in 1976 in a twin outbreak (Zaire/Congo and Sudan)
- Recent outbreak (2014) – 28,600 cases and 11,300 death as of November, 2015 (Zaire strain)
- Initial case traced to the handling of infected bushmeat as in prior cases
- 1st victim: 2 year boy in southeastern Guinea died in December 2013, followed by the deaths of several family members.
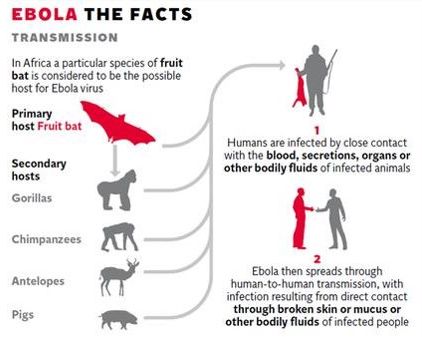
TRANSMISSION OF EBOLA VIRUS
High risk groups:
- Health care workers – involved in the treatment of patient
- Often, initially mistakenly classified as common diseases with resembling early symptoms – leading to spread with medical centers: Malaria, Dysentery, Influenza, Typhoid fever or other bacterial infections
- Laboratory personnel – handling infected material
- Family and friends – of infected person
- Burial ceremonies in which mourners have direct contact with the deceased
- Sexual partner of a known or suspected male case, as the virus remains present in semen up to 3 months after clinical recovery
Incubation period and spread from asymptomatic infected patients:
- Spread from asymptomatic infected individuals not possible
- Incubation period: 2-21 days (Average 8-10 days)
- Early, if injected with large amount of virus by reuse of needle
- Late, if exposed with external contact to small amount of body fluid from infected
- When the infected person is asymptomatic (in incubation period): Doesn’t shed virus (Non-contagious)
- When the infected person 1st start to exhibit symptoms: viremia is low (risk of transmission is low)
- When the disease progresses: viremia is high (risk of transmission is high)
- Based on Incubation Period, WHO and CDC recommend, potentially infected people with Ebola virus – be quarantined for 21 days.
Insect vectors may play a role:
- Nucleotide stability: Fairly stable at the nucleotide level, even when viruses are compared that were isolated from cases from past. This is characteristic of pathogens maintained in >1 host.
- Ebola does not appear to be easily transmitted via direct contact.
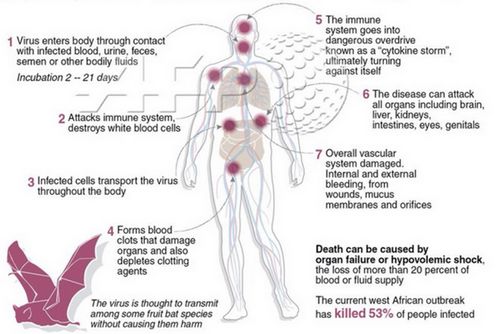
PATHOGENESIS OF EBOLA VIRUS DISEASE
1. Tissue invasion
2. Initial infection: Dendritic cells, monocytes and macrophages (replication)
3. Migration of infected cells to regional lymph nodes, spleen, liver
4. Dissemination of infection
5. Cytokine storm: when virus triggers expression of a host of pro-inflammatory cytokines, including: IFNs; ILs; TNF-alpha (damage to virus along with collateral damage to endothelial cells)
6. This leads to endothelial activation and reduced vascular integrity, release of tissue factor (coagulopathy), and increased nitric oxide levels (hypotension)
7. Lymphocyte depletion through indirect apoptosis (since the virus does not replicate in lymphocytes), and neutrophil suppression via glycoprotein GP
8. Thrombocytopenia – Platelet disappearance from damaged tissue or DIC
9. DIC + Hepatic dysfunction = Bleeding complications
10. Other complications: AKI, Hepatitis, Pancreatitis
11. Shock: Bacterial sepsis (gut translocation), Direct effect of virus, DIC or hemorrhage
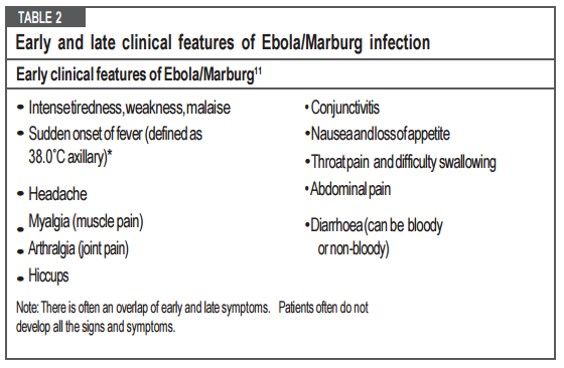
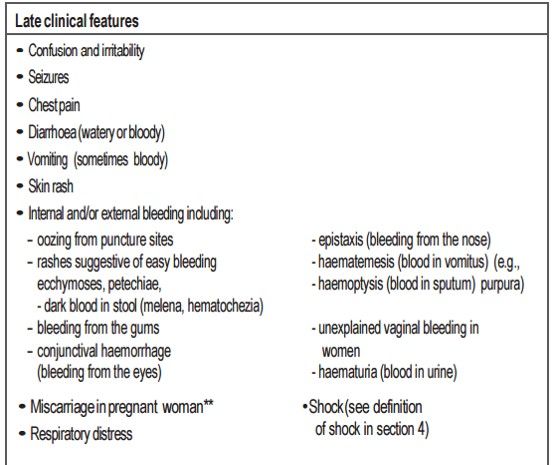
EARLY AND LATE CLINICAL FEATURES OF EBOLA VIRUS DISEASE

Nonpruritic, Erythematous
Begin focally, then become generalized, diffuse and confluent
Convert to purpuric or petechial (coagulopathy)\
Phases of illness:
1. Early febrile (0-3 days): Fever, malaise, fatigue, body aches
2. Gastrointestinal (3-10 days):
- Primary: Epigastric pain, nausea, vomiting, diarrhea
- Associated: Persistent fever, asthenia, headache, conjunctival injection, chest pain, abdominal pain, athralgias, myalgias, hiccup, delirium
3. Shock or recovery (7-12 days):
- Shock: diminished consciousness or coma, rapid thready pulse, oliguria, anuria, tachypnea
- Recovery: resolution of GI symptoms, increased oral intake, increased energy
4. Late complications (≥10 days):
- Gastrointestinal hemorrhage
- Secondary infections
- Meningoencephalitis
- Neurocognitive abnormalities
INVESTIGATIONS FOR EBOLA VIRUS DISEASE
1. RT-PCR (positive for ebola virus RNA):
- Results are available 4 hours after the sample has arrived
- Viral RNA can be detected in the patient’s blood by RT-PCR from day 3 up to days 6 to 17 of symptom onset.
- If negative, the test should be repeated within 48 hours since viral load is low and can be undetectable early in the course of the illness.
2. Malarial investigations: Negative (may be positive if dual infection)
3. ReEBOVTM Antigen Rapid Test Kit (Corgenix) – Indicated in:
- If the investigation of suspected Ebola outbreaks in remote settings where PCR tests are not immediately available
- In settings where the number of cases and suspects arriving for triage and care cannot be managed with the existing health staff and laboratory facilities
4. Other tests:
- Serum electrolytes level: may be abnormal
- BUN and creatinine: may be elevated
- ABG and Blood lactate: variable
- CBC: platelets↓, lymphocytes↓, Hb↓ (bleeding)
- Coagulation studies: ↑PT or aPTT, ↑D-dimer (bleeding)
- Urinalysis: +/- hematuria or proteinuria
- LFT: ↑AST to ALT ratio +/- ↑bilirubin, GGT and ALP
- Serum amylase: +/- ↑ (pancreatitis – severe disease)
- Blood cultures (r/o non-viral infections): -ve
- Antigen capture ELISA: +ve for Ebola RNA (day 3-6)
- IgM and IgG antibodies: +ve
- IgM: recent infection (by 1st wk & disappear by 1-5 mo)
- IgG: past infection (by 2nd wk & perist for years)
- Chest X-ray: +/-ARDS
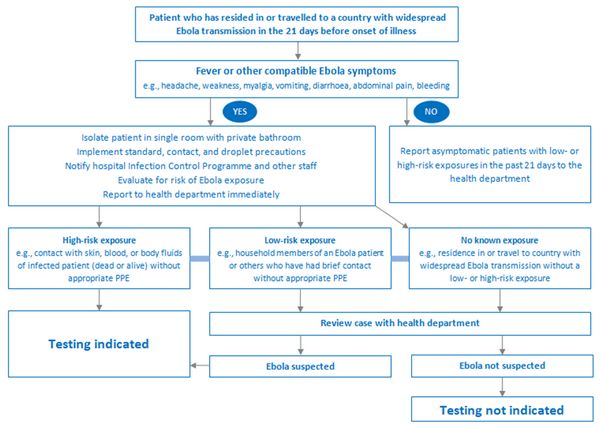
SURVEILLANCE OF EBOLA VIRUS DISEASE
A) Suspected case:
1. Alive/dead + Sudden onset high fever + Contact (Suspected/pobable/confirmed Ebola or Dead/Sick animal for Ebola) OR
2. Sudden onset high fever + ≥ 3 early symptoms (including vomiting) OR
3. Inexplicable bleeding
B) Probable case:
1. Clinician evaluated Suspect case OR
2. Deceased + Epidemiological link with confirmed case
C) Confirmed case: Suspect/Probable + RT-PCR/IgM +ve
TREATMENT OF EBOLA VIRUS DISEASE
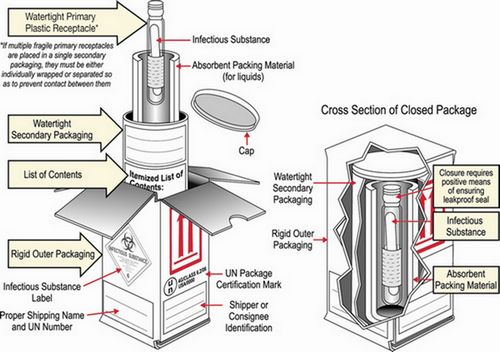
1. Isolation, Infection control and Notification of disease:
- Steps to put Personal protective equipment (PPE)
- Storage and shipment of collected sample:
- <24 hrs: Room temperature
- <1 week: 0-5° Celsius
- >1 week: -20 ° Celsius (or better at -70 ° Celsius if available)
2. Diarrhea, vomiting and dehydration:
| NO DEHYDRATION (PLAN A) | SOME DEHYDRATION (PLAN B) | SEVERE DEHYDRATION (PLAN C) |
| Drink Extra fluid •SOS (as much as needed) •≥ 200-300 ml/loose stool •Continue until diarrhea stops | ORS to give during 1st 4 hours: Use age or weight If weight known: 75 ml/kg Adults: upto 750 ml/hr Children: upto 20 ml/kg.hr Give more ORS if patient wants | If IV fluid possible: 100 ml/kg RL/NS <12 mo: 30ml/kg X 1 hr, 70ml/kg X 5 hr >12 mo: 30 ml/kg X ½ hour, 70 ml/kg X 2 ½ hours Plus ORS oral 5 ml/kg/hr (possible) Repeat X1 if radial pulse feeble |
| Continue eating Return to health facility when: •Diarrhea worsens •Persistent/large volume diarrhea | Re-assess and classify dehydration after 4 hours | If NG or oral rehydration possible: •ORS 20 ml/kg/hr for 6 hrs •Reassess every 1-2 hr •If hydration not improving after 3 hrs – send for IV therapy |
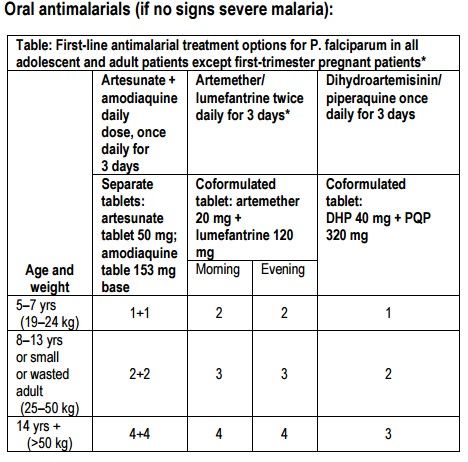
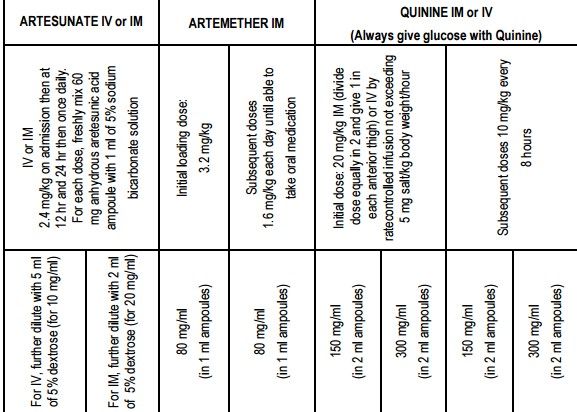
3. Malaria treatment:
4. Analgesics and antipyretics:
AVOID ASPIRIN AND NSAIDs due to ANTI-PLATELET EFFECTS
1st line: Paracetamol
- Children: 10-15 mg/kg PO/PR/IV every 4-6 hrs when required (max: 75 mg/kg)
- Adults: 500-1000 mg PO/PR/IV every 4-6 hrs when required (max: 4000 mg)
2nd line: Tramadol
- 50-100 mg every 4-6 hrs (max: 400 mg/day)
3rd line: Morphine sulfate
- Children: 0.2-0.4 mg/kg PO every 4-6 hrs OR 0.05-0.1 mg/kg IV every 4-6 hrs
- Adults: 2.5-10 mg PO/IV every 4 hrs when needed
5. Anti – Emetic:
1st line: Ondansetron
- Avoid in arrhythmias and co-administration with tramadol
- 4-8 mg PO/IV 8 hrly (max: 24 mg/day)
2nd line: Metoclopramide 10 mg PO/IV every 8 hrs (max: 30 mg/day)
6. Heartburn/Dysphagia/Abdominal Pain:
- Adults and children ≥ 10 years: Omeprazole 20 mg PO daily OR Magnesium trisilicate 2 tabs PO every 8 hrs
- Children 5-12 years: Magnesium trisilicate 5-10 ml, 3 times daily
7. Convulsions:
- Recognize and correct contributing factors (fever, dyselectrolytemia)
- Abort seizure: BZDs (Diazepam 5-10 mg IV/IM, repeat every 10-15 min if required; max 30 mg/dose OR 0.2 mg/kg PR – can be repeated in 4 to 12 hrs)
- Control seizure: Phenobarbital 10 mg/kg IV followed by 5 mg/kg every 30-60 minutes until seizure control (max total loading dose 30 mg/kg)
8. Signs of hypoglycemia:
- Test glucose – if low, give IV D50 25-50 ml; Nutritional support
9. Agitation:
- Diazepam 5 mg PO/IV single dose OR
- Haloperidol 5 mg IM single dose
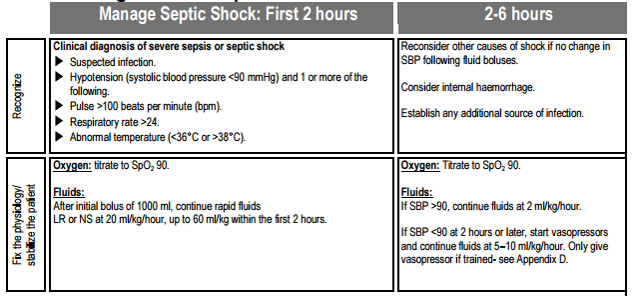
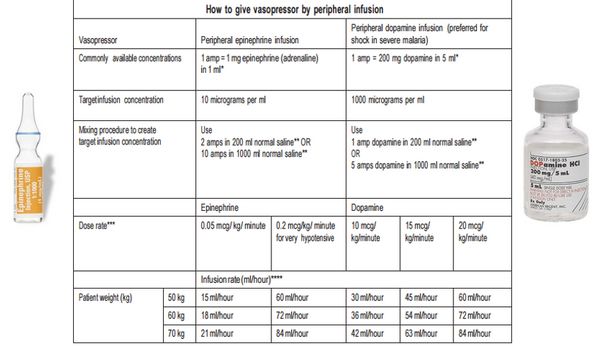
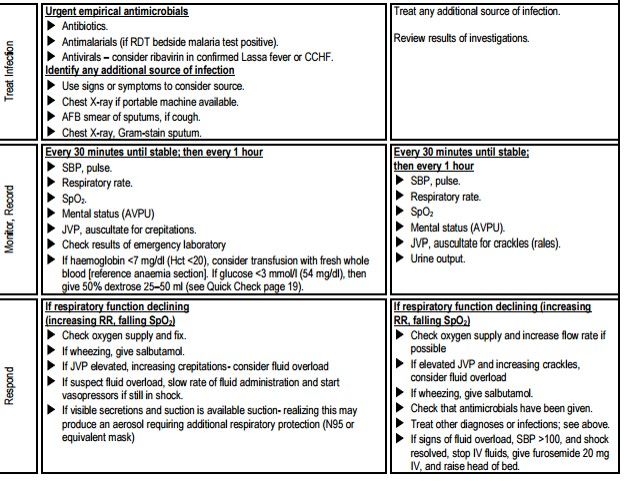
10. Management of spetic shock:
Options for empirical antibiotics:
Ceftriaxone 2 g IV OR Ampicillin 2 g q6h + Gentamicin 1.5 mg/kg IV q8h + Ciprofloxacin
11. Consider:
- With hemorrhage or DIC: Platelet or Plasma transfusion
- Broad-spectrum antibiotics: Endemic areas with poor access to diagnostic tests
- Convalescent whole blood and plasma: Transfusion of blood from convalescent patients could be beneficial in the acute phase of infection, and may reduce mortality
EXPERIMENTAL THERAPIES FOR EBOLA VIRUS DISEASE
- Favipiravir (Antiviral active against RNA viruses including Influenza and Yellow fever)
- TKM-Ebola (Short RNA sequence that cleaves Ebola RNA in cells and prevent virus multiplication)
- Zmapp/MIL-77 (Cocktail of 3 monoclonal antibodies with neutralizing activity against Ebola virus)
- Others: BCX-4430, Interferons, Amiodarone, Atorvastatin + Irbesartan +/- Clomiphene, FX06, Zmab, Amodiaquine, Brincidofovir
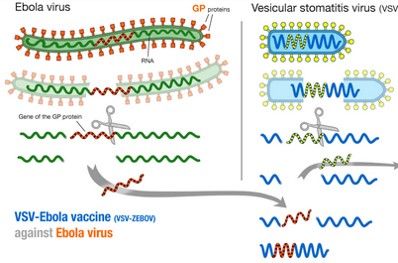
VACCINES UNDER TRIAL FOR EBOLA VIRUS DISEASE
- ChAd3-ZEBOV
- rVSV-ZEBOV
- Ad26-EBOV and MVA-EBOV
- Recombinant protein Ebola vaccine
References:
WHO VHF Pocket book (2014)
CDC – Ebola Virus Disease
WHO – Steps to put on PPE; steps to remove PPE
WHO – Ebola vaccines, therapies and diagnostics
BMJ best practice – Ebola Virus Infection
Deadly Disease and Epidemics : Ebola – Tara C Smith
Robert Koch Institute – Framework Ebola Virus Disease
Author: Sulabh Shrestha