A) General consideration:
Febrile seizures are seizures during fever occuring between 6 months and 5 years of age in absence of:
- CNS infections
- Abnormal neurologic findings
Types of febrile seizure:
- Simple febrile seizure:
- Solitary
- Brief (< 15 minutes)
- Within 24 hours of onset of fever
- Generalized Tonic Clonic Seizure (GTCS)
- Atypical/Complex febrile seizure:
- Lasting more than 15 minutes
- Multiple occurence in a day
- Focal seizures
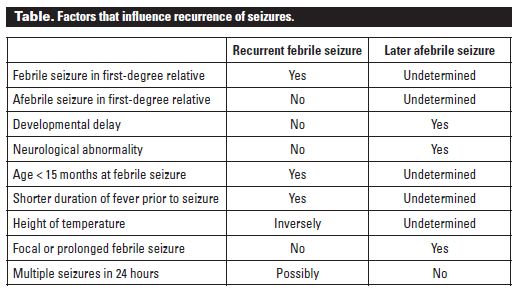
Risk of recurrence:
Risk of reccurence increases in following conditions:
- Age < 18 months
- Family history of febrile seizure
- Low peak temperature
- Shorter duration of fever
HISTORY FOR FEBRILE SEIZURE
1. Seizure:
- Generalized or focal at onset?
- Incontinece of urine and tongue biting confirms generalized nature of seizure
- Unilateral postictal weakness (todd paresis) or speech difficulty indicates focal onset of seizure
- Length of seziure:
- Simple or typical vs Complex or atypical febrile seizure
- Status epilepticus (>30 minutes)
- Differentiate between seizure itself and postictal state
- Prior history of seizures with or without fever?
- If more than 1 seizure occured in 24 hours?
2. Nature of illness and relation to seizure:
- How long was the temperature elevated before onset of seizure?
- Rule out possible CNS infections?
- Altered mental state
- Severe headache
- Focal signs before seizure
- Evidence of acute rise in ICP?
- Any treatment or drugs received?
3. Family history: Epilepsy ?
4. Rule out differential diagnoses:
- School aged child, partial seizure in sleep: Benign epilepsy of childhood with centrotemporal spikes (Benign rolandic epilepsy)
- Early morning tonic-clonic seizure: Juvenile myoclonic epilepsy
- Possible precipitants: Toxins or drugs
- Pre-existing developmental/neurologic disorders
- Immunization: Pertussis
- Post-infection: Varicella, Measles
- Non-epileptic paroxysmal events:
- Breath holding attacks
- Benign nocturnal myoclonus
- Shuddering or shivering attack
- Tics/Tourette
- Night terrors
- Migraine
- Conversion disorder
- Staring spells
- Benign Positional Paroxysmal Vertigo (BPPV)
PHYSICAL EXAMINATION FOR FEBRILE SEIZURE
1. Source of infection or fever?
- Acute Gastroenteritis (AGE)
- Sepsis
- Otitis Media
- Urinary tract infection
- Penumonia
- Upper respiratory tract infection
2. Features of meningitis: Meningismus is absent in 1/3rd infants
3. Features of raised ICP:
- Abnormal eye movement (setting sun sign)
- Excessive vomiting
- Cushing’s triad: Raised blood pressure, Irregular respiration and Bradycardia
- Papilledema
4. Examine scalp for head trauma
5. Complete neurologic examination to rule out focus
6. Examination of skin:
- Neurofibromatosis: Cafe-au-lait spots
- Tuberous sclerosis:Ash-leaf lesions (hypopigmented lesions with pointed tip)
- Sturge-Weber syndrome: Facial hemangioma
INVESTIGATIONS FOR FEBRILE SEIZURE
Consider following investigations according to the history and examination:
- CBC, differential counts and C-reactive protein (CRP)
- Cultures (blood and urine)
- Lumbar puncture
- Urinalysis
- Electrolytes
- Random blood glucose
- BUN and creatinine
- Calcium and Magnesium levels
- Toxicology screen
- Metabolic tests (In infants and mental retardation)
- Stool culture (If shigellosis is suspected)
- CT or MRI (MRI is preferred):
- Rarely required in:
- Febrile seizures
- Absence seizure
- Benign rolandic epilepsy
- Nonfebrile Generalized seizure with normal examination findings
- Required in:
- Features suggestive of raised ICP
- Intracranial hemorrhage
- Space Occupying Lesions
- Difficulty controlling seizure
- Prolonged unresponsiveness
- Progressive neurologic findings
- Rarely required in:
- EEG:
- To document ongoing seizure
- To identify underlying cerebral structural process
- Identify risk of recurrence
- Diagnosing epilepsy syndromes
- May be part of evaluation of 1st unprovoked seizure (controversy – very low reccurence risk) or 2nd
MANAGEMENT OF FEBRILE SEIZURE
1. Hospitalization: Indications of hospitalization are –
- Number of seizures: 2 or more spontaneous seizures within 24-48 hours
- Duration of seziures: Prolonged seizures that resolved spontaneously
- Prolonged altered mental state or focal signs
- Initiation of anticonvulsant therapy (Observation)
- Severe febrile seizure:
- Serious bacterial infections
- Bacteremia
- Meningitis
- Pneumonia
- UTI/pyelonephritis
- Bacterial enteritis
- Very severe febrile seizure:
- Status epilepticus
- Shock
- Coma
- Respiratory failure
- Hypoxia
2. Antipyretics
3. Benzodiazepines if needed
4. Education and reassurance
PROPHYLAXIS OF FEBRILE SEIZURE
1. Intermittent prophylaxis:
Indications:
- 3 or more episodes in 6 months
- 6 or more episodes in 1 year
- Lasting more than 15 minutes
Regimen:
- 2 doses of oral diazepam 0.3-0.5 mg/kg given 8 hours apart at the time of fever (or rectal diazepam or clobazam for 3 days)
- Antipyretics
- Hydrotherapy
2. Continuous prophylaxis:
Indications:
- Failed intermittent prophylaxis
- Recurrent atypical febrile seizure
- Parents unable to recognize onset of fever
Regimen:
- Valproate or Phenobarbitone X 1-2 years or untile 5 years of age