Synonyms: Courvoisier’s sign, Courvoisier syndrome, Courvoisier-Terrier sign, Bard-Pic disease
Over years, the use of the term Courvoisier’s sign or gallbladder has been suggested instead of law, because of rising number of exceptions.
Eponymous to: Ludwig Courvoisier (1843-1918)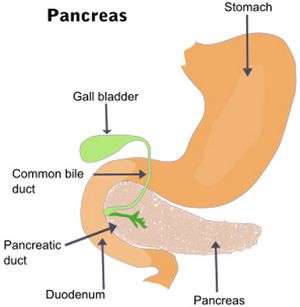
Definition of Courvoisier’s law
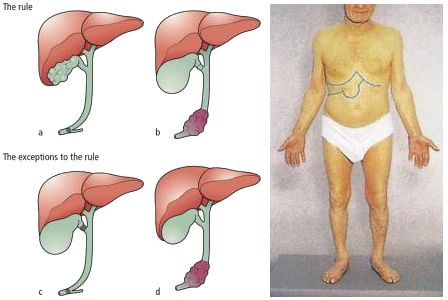
Courvoisier’s (koor-vwah-zee-ayz) law states that ‘a palpable non-tender gallbladder in the presence of jaundice is unlikely to be due to gallstones’. It usually indicates a neoplastic stricture obstructing the distal common bile duct. A palpable gallbladder due to stones is usually tender i.e. due to acute cholecystitis.
Basis of Courvoisier’s law
A gallbladder containing stones is likely to have been chronically diseased and subject to repeated, although possibly subclinical, episodes of cholecystitis. This results in extensive fibrosis of the gallbladder wall which is then unable to distend when obstructed. A contracted gallbladder is consistent with obstruction above the level of the cystic duct insertion.
Converse of Courvoisier’s law
The converse of this law is not true; the cause of jaundice in non-palpable gallbladder is not necessarily gallstones as 50% of dilated gallbladders are not palpable.
Differential diagnoses of Courvoisier’s law
1. Periampullary tumors (Bulging papilla sign on radiograph):
- Tumors of pancreatic head/uncinate process
- Tumors of distal common bile duct
- Ampullary tumors (of ampulla of vater)
- Periampullary duodenal tumors
2. Pancreatic stricture: Chronic pancreatitis
3. Portal lymphadenopathy
4. Bile duct obstruction due to ascaris
5. AIDS associated cholangiopathy
Exceptions of Courvoisier’s law
1. Double impaction: Stones, simultaneously occluding the cystic duct and the distal common bile duct (CBD). The stone in the CBD causes obstructive jaundice and a synchronous stone in the cystic duct leads to mucocele or empyema of gall bladder.
2. Pancreatic calculus obstructing the ampulla of vater
3. Oriental cholangiohepatitis (Ductal stones formed secondary to liver fluke infestation)
4. Periampullary carcinoma in patients with cholecystectomy
5. Mirizzi syndrome: A stone is lodged in Hartman’s pouch causing intense inflammation in the region of Calot’s triangle and compressing the common hepatic duct, while also obstructing the gall bladder; this causes the gallbladder to distend.
Double duct sign
The combined dilatation of pancreatic and common bile ducts is known as double duct sign and occurs most commonly in malignancy of the head of pancreas.
Please, I need you to explain how portal lymphadenopathy leads to a PAINLESS DISTENDED gallbladder. Thank you.
Portal LN compresses on the bile ducts causing, biliary obstruction leading to distension of GB.
hi, what is oriental cholangiohepatitis, can u explain it in simple ways ? tq
Oriental cholangiohepatitis is also called as Recurrent Pyogenic Cholangitis (RPC) by Chinese clinicians. It is an endemic disease of Southeast asia. It is commonly caused by infestation of Fluke (Clonorchis sinensis) and other parasites like fasciola hepatica, ascaris, etc. It is characterized by intrahepatic pigmented stones and recurrent bouts of cholangitis. The fluke acts like a nidus for stone formation and either directly or by causing strictures aids which to their formation.
Can you please explain the exception once ?
Does these exceptions mean that the gall stone has been formed, it might have moved to the CBD as secondary CBD stones and cause distention of GB as well as jaundice ?
What you meant to say are secondary CBD stones. As per courvoisier’s law, they wouldn’t cause enlarged gallbladder (atrophy due to chronic or recurrent cholecystitis) although the migrated CBD stone may lead to Jaundice.
While in distal CBD obstruction due to malignancy, chronic rise in intraductal pressureleads to gallbaladder distension, cholelithiasis are usually associated with chronic cholecystitis leading to fibrosis and shrinkage of gall bladder. Obstruction of cystic duct is usually by stones (rarely malignancy) and cystic duct obstruction doesn’t produce derangement in the liver function – hence, even if enlarged due to mucocele or empyema (painful), there is no jaundice.
So, the exceptions would be:
1. To have palpable gallbladder with jaundice in patient with stones. Examples-
2. To not have palpable gallbladder with jaundice in patient with periampullary carcinoma.
e.g. Cholecystectomy in patient with distal CBD compression from malignancy – although LFT is deranged, no gallbladder is present to be enlarged.
If you still have confusion, feel free to ask us.
Hope this helps you.
I really appreciate the excellent work done to up this article. Much thanks. More research is expected.
Hey there, thank you for the helpful information, glad to come across your website during revision. However, I’m still confused in certain areas.
For choledocholelithiasis (obstruction at CBD), it is also an acute condition where the stones lodges at CBD causing increased biliary tree pressure –> subsequently causing gallbladder distension. It also blocks the CBD causing jaundice. Doesn’t it fulfill the Courvoisier’s Law? (I’m not sure whether it causes pain)
As for the double stone impaction, you mentioned that the stone’s blockade at the cystic duct can lead to enlarged gallbladder due to mucocele. Wouldn’t this cause pain as well? I picture it the same as acute cholecystitis secondary to cholelithiasis obstruction at cystic duct. If so, it no longer obeys the Courvoisier’s Law right?
Looking forward to your teachings, thank you very much.
Nice questions Kai.
Courvoisier’s law: Palpable non-tender gallbladder + Jaundice = Unlikely to be due to gall stones
1. Acute cholecystitis = Tender palpable gallbladder
2. Chronic cholecystitis = Non-palpable gallbladder
3. Double impaction = Tender palpable gallbladder due to mucocele (that’s why an exception – as the stone is not expected to follow the rule)
This is our understanding.
It is very good and easy to understand
Admin……my doubt is that the law mentions it as “gallstones”…so the exceptions should be in the view of gallstones right? I think Harshit was trying to ask the same.
Courvoisier originally didn’t give a law but described 187 cases of common bile duct obstruction, making the observation that gallbladder dilatation seldom occurred with stone obstruction of the bile duct. In his findings, malignancy was the commonest finding responsible for gall bladder distension. His observation was latter named as “law” or “sign” and there’s no clear consensus to what constitutes the exceptions. I think, various book authors have used exception as:
1. Either the presence of gallstones in a case of distended, non-tender gallbladder with jaundice
2. Or, the non-malignant causes responsible for distended, non-tender gallbladder with jaundice
That was very helpful. Thank you!
Dear Sir/Madam,
I’m extremely happy motivated by your website discussion and please can you take through cancers of biliary tree.
thanks
Hello William, we have done an article on your request. Please read and leave your feedback and queries.
http://epomedicine.com/medical-students/cholangiocarcinoma-bile-duct-cancer-made-easy/
Could you explain why Periampullary carcinoma in patients with cholecystectomy is an exciption of the law ?
How GB can be palpable inspite of its removal ?
Hello Ahmed,
The exception is in the sense that, gallbladder wouldn’t be palpable despite of periampullary carcinoma.
Just came here to say..you are wonderful. Thanks you cleared every doubt that i had. I am so grateful.
Please kindly throw more explanation on mirizzi syndrome.
Can all patients with mirizzi syndrome present with classical triad of fever, right upper quadrant pain and jaundice?
This study have found occurrence of signs and symptoms in Mirizzi syndrome as follows:
1. Abdominal pain (100%)
2. Jaundice (87.5%)
3. Nausea and vomiting (62.5%)
4. Choluria (62.5%)
5. Fever (25%)
Average total bilirubin was 8.5 mg/dl.
Waisberg J, Corona A, de Abreu IW, Farah JF, Lupinacci RA, Goffi FS. Benign obstruction of the common hepatic duct (Mirizzi syndrome): diagnosis and operative management. Arq Gastroenterol. 2005 Jan-Mar;42(1):13-8. doi: 10.1590/s0004-28032005000100005. Epub 2005 Jun 22. PMID: 15976905.
Also, another study delineated the preoperative diagnostic scoring system for Mirzizi syndrome. According to the study:
“Score of 3 or more was found to have a 90% sensitivity of predicting MS among complicated cholecystitis. Similarly, a score of 6 or more had an 80% sensitivity of predicting Mirizzi’s types II, III, and IV indicating fistulization. Jaundice, leucocytosis, associated choledocholithiasis/hepatolithiasis, intrahepatic biliary radical dilatation, meniscus sign and mass at confluence were found to be significant parameters.”
For further reading, you can go through the article mentioned below.
Tataria RD, Salgaonkar HP, Maheshwari G, Halder PJ. Mirizzi’s syndrome: A scoring system for preoperative diagnosis. Saudi J Gastroenterol. 2018 Sep-Oct;24(5):274-281. doi: 10.4103/sjg.SJG_6_18. PMID: 29873320; PMCID: PMC6151998.
Can you please explain the prognosis or outcome of courvoisier’s gallbladder/syndrome. What happen if left untreated?