Cellulitis is a rapidly spreading acute inflammation with infection of skin and subcutaneous tissue that spreads widely through tissue spaces. It is commonly caused by either Streptococcus pyogenes or Staphylococcus aureus. Erysipelas is a superficial form of cellulitis involving lymphatics; it has a peau d’orange appearance and a sharp border. It characteristically appears on the face.
Since, cellulitis lacks pathognomic findings, it can be challenging to diagnose it and may often be confused with pseudo-cellulitis or cellulitis mimics. Pseudocellulitis conditions include stasis dermatitis, venous ulceration, acute lipodermatosclerosis, pigmented purpura, vasculopathy, contact dermatitis, adverse medication reaction, and arthropod bite. Stasis dermatitis and lipodermatosclerosis, both resulting from venous insufficiency, are the most common skin conditions that mimic cellulitis.

Mnemonic: CELLULITIS
1. Cellulitis history (prior): Single most important history (present in nearly 50% cases with odds ratio/OR 31)
2. Edema and Erythema: OR for edema is 6.77; Erythema is the least useful sign of inflammation
3. Local warmth: Temperature difference of >/= 0.47 degree celsius between affected and unaffected skin showed 87.5% accuracy in diagnosing cellulitis
4. Lymphangitis: May be associated with ascending lymphangitis (continuous or interrupted red streaks) or lymphadenopathy
5. Unilateral: Unilaterality is the most useful criterion distinguishing cellulitis from mimics (OR 8.65); stasis dermatits (a mimic) is often bilateral
6. Leukocytosis: OR 2.43
7. Injury: Local injuries and skin disruptions are more predictive of cellulitis than systemic factors like diabetes, obesity, and smoking (OR for ulcer is 12.73 and injury is 19.11)
8. Tenderness: More useful diagnostic factor than the resting pain
9. Instant onset: Patient often clearly remember the day of onset of cellulitis but the same for stasis dermatitis is vague
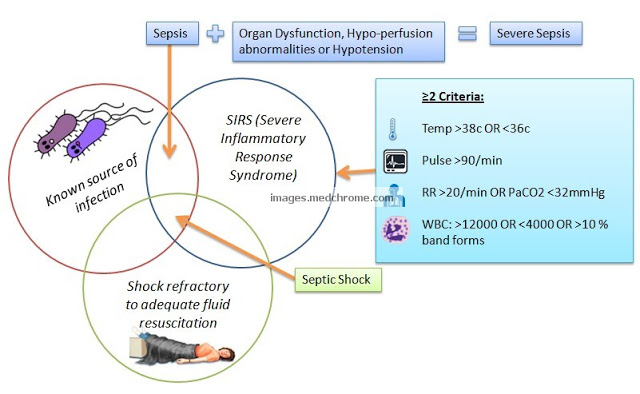
10. Systemic signs: SIRS criteria can be used to classify cellulitis which can guide the treatment (OR for heart rate >/= 90/min is 1.94).
- No SIRS criteria met: Mild cellulitis
- >/= 1 SIRS criteria: Moderatre cellulitis
- >/= 2 SIRS criteria + Hypotension Or Immune compromise Or Rapid disease progression: Severe cellulitis
Antibiotic selection in Cellulitis:
- Mild cellulitis: Oral Cephalexin, Dicloxacillin, Penicillin VK or Amoxicillin/Clavulanate
- Moderatre cellulitis with 1 SIRS criterion: As in mild cellulitis (switch to IV antibiotics if treatment failure)
- Moderatre cellulitis with >1 SIRS criteria: IV Cefazolin, Ceftriaxone or Penicillin G
- Severe cellulitis:
- Start with Vancomycin + Tazobactam/Piperacillin, Imipenem, Meropenem
- Possible necrotizing cellulitis: Surgical assessment with culture and sensitivity of any surgically obtained tissue
- Signs of shock: Penicillin G and Clindamycin for potential streptococcal shock syndrome
Adjust antibiotic selection based on culture results, local resistance patterns, and clinical response after 24-48 hours. If unresponsive after 24-48 hours, consider possible pseudocellulitis or resistant or atypical organisms.
Use clindamycin in penicillin allergy. Linezolid can be used if intravenous vancomycin is contraindicated.
Another literature evaluated the NEW HAvUN – a mnemonic critera.
- New onset (</= 3 days duration)
- Erythema
- Warmth (Pyrexia >100.4 F)
- History of associated trauma (mechanical, surgical, bite, burn)
- Ache (Tenderness to light touch)
- Unilaterality
- Number of WBC (>10,000/cu.mm)
Each of these are scored as 1 with a maximum possible score of 7. The study found that testing positive for 4 of 7 clinical criteria was highly specific (95%) and sensitive (100%) for a diagnosis of cellulitis among its range of
mimics.
Reference:
1. Neill BC, Stoecker WV, Hassouneh R, Rajpara A, Aires DJ. CELLULITIS: A mnemonic to increase accuracy of cellulitis diagnosis. Dermatol Online J. 2019 Jan 15;25(1):13030/qt9mt4b2kc. PMID: 30710907.
2. Raff, A. B., & Kroshinsky, D. (2016). Cellulitis. JAMA, 316(3), 325. doi:10.1001/jama.2016.8825
3. Ezaldein HH, Waldman A, Grunseich K, Jubanyik K. Risk stratification for cellulitis versus noncellulitic conditions of the lower extremity: a retrospective review of the NEW HAvUN criteria. Cutis. 2018 Jul;102(1):E8-E12. PMID: 30138510.

He is the section editor of Orthopedics in Epomedicine. He searches for and share simpler ways to make complicated medical topics simple. He also loves writing poetry, listening and playing music.