DEFINITION OF BRONCHIECTASIS
Bronchiectais refers to the end-stage of variety of pathologic processes characterized by abnormal, irreversibly dilated thick-walled bronchi due to destruction of elastic and muscular components of bronchial wall.
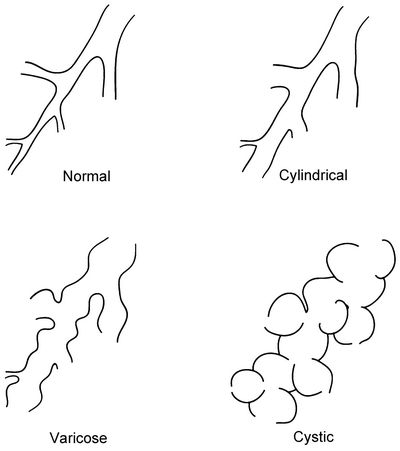
MORPHOLOGICAL CLASSIFICATION OF BRONCHIECTASIS
Mnemonic: CVS
1. Cylindircal (Fusiform):
- involves airways from 6th-10th generation
- bronchi have uniform calibre, do not taper and have parallel walls
- commonest form
2. Varciose:
- resembles varicose vein
- beaded appearance where dilated bronchi have interspersed sites of narrowing
- relatively uncommon
3. Saccular (Cystic):
- occurs in proximal bronchi
- dilation ends in large cysts, saccules or grape-like clusters
- most severe form
ETIOLOGY OF BRONCHIECTASIS
a. Structural lung conditions:
- Williams-Campbell syndrome (deficiency or absence of cartilage, mostly from the third division of the bronchi down)
- Mounier-Kuhn syndrome (tracheobronchomegaly)
- Ehler’s Danlos syndrome
b. Toxic damage to airways:
- Inhalational injury
- Aspiration secondary to neuromuscular disease
- GERD
c. Obstruction of single bronchus:
- Foreign body
- Tumor
- Lymph nodes
d. Obstructive airway disease:
- Asthma
- COPD
- Alpha-1-antitrypsin deficiency
e. Defects of mucociliary clearance:
- Ciliary dyskinesia: Primary (e.g. Kartagener’s syndrome), Secondary (P.aeruginosa, H.influenzae, cigarette smoke, aspiration of gastric contents)
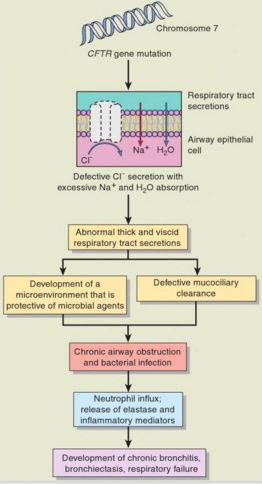
- Channelopathies: CFTR (inhibitor of eNAC) dysfunction (Cystic fibrosis), eNAC dysfunction
f. Allergic Bronchopulmonary Aspergillosis (ABPA)
g. Immunodeficiency:
- Common Variable Immunodeficiency (CVID)
- X-linked Agammaglobulinemia (XLA)
- Chronic granulomatous disease (CGD)
- Secondary: Hematologic malignancy, GVHD
h. Infections:
- Childhood infections: TB, pneumonia, measles, whooping cough
- Nontuberculous mycobacteria
i. Traction:
- Post-tuberculous fibrosis
- Post-radiation fibrosis
- Fibrosis (sarcoidosis)
- Inflammatory bowel disease
j. Connective tissue diseases
k. Yellow nail syndrome (bronchiectasis, lymphoedema and a characteristic appearance of the nails)
l. Idiopathic
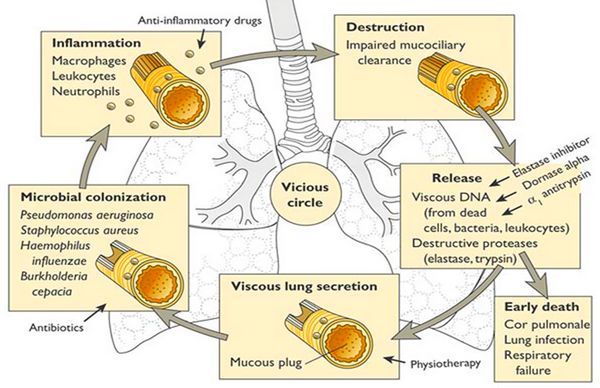
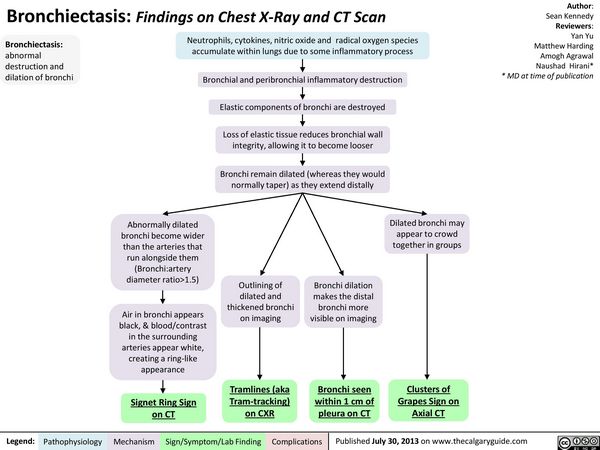
PATHOGENESIS OF BRONCHIECTASIS
PATHOLOGY OF BRONCHIECTASIS
- Characterisitc feature: multiple bronchiectatic cavities
- Left lung is involved more than right lung
- Lower lobes are involved more than upper lobes due to more efficient drainage of upper lobes by gravity
- Common sites of involvement: lower lobes, lingula and middle lobe
- Smaller bronchi with less supportive cartilage are predominantly involved
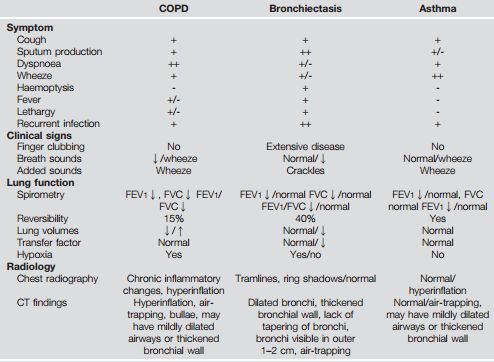
PATHOPHYSIOLOGY AND CLINICAL FEATURES OF BRONCHIECTASIS
The clinical manifestations result due to pathophysiologic mechanisms caused by following anatomic alterations:
- Incomplete obstruction: Hyperinflation of the distal alveoli as a result of expiratory check-valve mechanism
- Complete obstruction: Atelectasis, consolidation and fibrosis
A. Cough, Sputum production, Hemoptysis and Recurrent Infection:
- Chronic cough with production of large quantities of foul-smelling sputum (due to anaerobic infection) is a hallmark
- Productive cough: due to stimulation of subepithelial mechanoreceptors in tracheobronchial tree by stagnant secretion, which produces vagal reflex that triggers cough
- 24 hour collection of sputum: is usually voluminous and tends to settle in 3 different layers – mucoid layer on top, mucopurulent layer in middle and purulent layer at bottom
- Sputum production varies with posture: and is maximum within 2 hours of waking up (stagnation of sputum while asleep)
- Hemoptysis: due to necrosis of bronchial wall and erosion of bronchial blood vessels
- Secondary bacterial infection: frequent due to excessive bronchial secretion – H.influenzae, Streptococcus, P.aeruginosa, various anaerobic organisms
Bronchiectasis sicca (Dry bronchitis): repeated episodes of hemoptysis without sputum production; occurs in upper lobe bronchiectasis of post-tubercular variety
Middle lobe bronchiectasis/Middle lobe or Brock’s syndrome: post-obstructive bronchiecatasis due to obstruction of middle lobe by tubercular lymph nodes
B. Vital signs:
1. Tachypnea:
- Stimulation of peripheral chemoreceptors (V/Q mismatch and hypoxemia)
- Decreased lung compliance and increased ventilatory rate relationship
- Anxiety
2. Tachycardia and Raised Blood pressure:
- Stimulation of medullary vasomotor center (V/Q mismatch and hypoxemia)
3. Fever: Inflammatory response in cases of infection
C. General examination:
Use of accessory muscles, Pursed lip, Barrel chest:
- Increased airway resistance and increased work of breathing
Cyanosis:
- Hypoxemia
Digital clubbing (2-3% cases):
- Megakaryocytes bypass lung mechanism and lodge in peripheries and release PDGF and VEGF resulting in vasodilation and fibroblast deposition
Peripheral edema and venous distension:
- Corpulmonale
4. Chest findings:
- When bronchiectasis pathology is primarily obstructive:
- Decreased tactile and vocal fremitus; Hyperresonant percussion note
- Decreased lung density
- Diminished breath sounds
- More air in alveoli – hence, more muffling effect of alveolar air
- Prolonged expiration
- Wheezing
- Crackles
- Decreased tactile and vocal fremitus; Hyperresonant percussion note
- When bronchiectasis is primarily restrictive (atelectasis, fibrosis, consolidation):
- Increased tactile and vocal fremitus; Dull percussion note
- Increased lung density
- Bronchial breath sounds
- No air in alveoli – hence, muffling effect of alveolar air lost
- Crackles
- Whispering pectoriloquy
- Increased lung density
- Increased tactile and vocal fremitus; Dull percussion note
INVESTIGATIONS FOR BRONCHIECTASIS
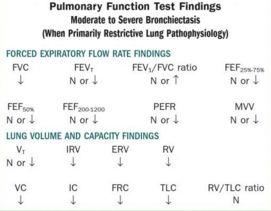
A. Pulmonary Function Test (PFT) findings:
1. Primarily obstructive pattern:
| FVC | FEVT | FEV1/FVC ratio | FEF25%-75% |
| ↓ | ↓ | ↓ | ↓ |
| FEF50% | FEF200-1200 | PEFR | MVV |
| ↓ | ↓ | ↓ | ↓ |
| VT | IRV | ERV | RV | |
| N or ↑ | N or ↓ | N or ↓ | ↑ | |
| VC | IC | FRC | TLC | RV/TLC ratio |
| ↓ | N or ↓ | ↑ | N or ↑ | N or ↑ |
2. Primarily restrictive pattern:
B. ABG findings:
1. Mild to moderate stages: Acute alveolar ventilation with hypoxemia (Respiratory alkalosis)
- Increased pH, decreased PaCO2, decreased PaO2, decreased HCO3
2. Severe stages: Chronic ventilatory failure with hypoxemia (Compensated respiratory acidosis)
- Normal pH, Increased PaCO2, Increased HCO3 (significantly), Decreased PaO2
C. Oxygen indices:
1. Qs/Qt (Shunt equation – percentage of blood flow not exposed to inhaled gas): Increased
Qs/Qt = (CcO2 – CaO2)/(CcO2 -CvO2) * 100
CcO2 = Oxygen content of pulmonary capillary
CaO2 = Oxygen content of artery
CvO2 = Oxygen content of vein
Normal <10%
2. DO2 (Total oxygen delivery): Decreased
DO2 = Cardiac output
x (CaO2 x 10)
Normal ~ 1000 mlO2/min
3. C(a-v)O2 (Arterial venous oxygen content difference): Normal
C(a-v)O2 = CaO2 – CvO2
Normal ~ 5 vol%
4. VO2 (Oxygen consumption): Normal
VO2 = Cardiac output X C(a-v)O2 X 10
Normal ~ 250 mlO2/min
5. O2ER (Oxygen extraction ration): Increased
O2ER = (CaO2 – CvO2)/CaO2
Normal ~ 0.25
6. SvO2 (Mixed venous oxygen saturation): Decreased
Normal 65-75%
D. Abnormal Lab tests and results:
1. Complete blood count:
- Increased hematocrit and hemoglobin (hemoglobin may be low due to anemia of chronic inflammation)
- Increased WBC in acute infection
2. Sputum culture results:
- S.pneumoniae
- H.influnezae
- P.aeruginosa
- Anaerobic organisms
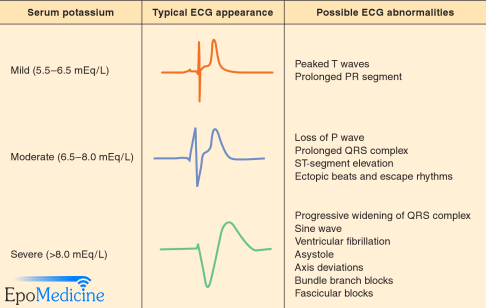
E. ECG:
- Normal (usually)
- Features of Right Ventricular Hypertrophy (RVH) and Cor pulmonale
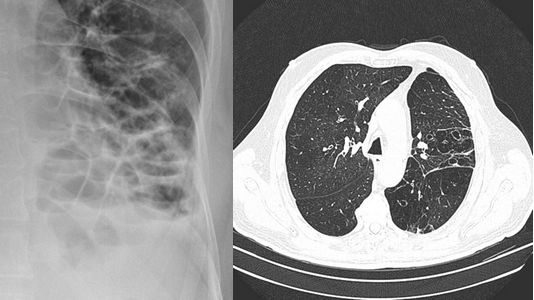
F. Chest Radiographs:
With primarily obstructive disease:
- Emphysematous changes with tubular heart
- Enlarged heart (if heart failure present)
- Tram-tracks (cylindrical), Honey-comb (cystic), signet-ring deformity
- Areas of consolidation and/or atelectasis may be seen
With primarily restrictive disease:
- Atelectasis and consolidation
- Infiltrates (suggesting pneumonia)
- Increased opacity
Bronchogram has been replaced by HRCT.
Specific features:
- ABPA: upper zone central bronchiectasis
- Cystic fibrosis: upper zone bronchiectasis
- Nontuberculous mycobacteria and MAC: middle lobe irregular branching and tree-in-bud appearance
G. Bronchoscopy:
- Doesn’t establish diagnosis
- For identifying source of secretions
- For identifying the site of bleeding in hemoptysis
- For therapeutic and diagnostic evacutation of sputum
- Dilatation of airways and purulent secretions
- Thickened bronchial walls with necrosis of bronchial mucosa
- Peribronchial scarring
H. Further investigations according to suspected cause:
| Aetiology | Suggestive signs | Additional investigations | Expected abnormalities |
| Cystic fibrosis | Age under 40, malabsorption, poor growth, infertility in males, faecal masses on abdominal x-ray, diabetes | Sweat test | Positive sweat test: chloride concentration >60 mEq/l |
| Genetic testing | 2 CFTR mutations | ||
| NPD | Abnormal NPD | ||
| Congenital disorders | Primary ciliary dyskinesia: sinusitis, otitis media, hearing loss, poor sense of smell, middle lobe predominance | Nasal epithelial brushing or biopsy | Abnormal ciliary beat pattern and frequency of ciliogenesis in culture |
| Nasal NO measurement (>5 years of age) | Nasal NO <150 ppb | ||
| Saccharin test (no clinical value anymore) | Increased time (>60 min) before tasting saccharin | ||
| Marfan’s syndrome: myopia, arachnodactylia, tall stature, thoracic deformations, glaucoma, abnormal joint flexibility, heart murmur | Search for major and minor indicators of the disorder | Diagnosis based on family history and a combination of major and minor indicators of the disorder, rare in the general population but occurring in one individual Genetic testing | |
| α1-Antitrypsin deficiency | α1-Antitrypsin deficiency | Levels below 150 mg/dl | |
| Anatomical deformations: visible on clinical examination | Thoracic imaging | Scoliosis or pectus excavatum | |
| IBD | Diarrhoea, abdominal pain, haematochezia, weight loss, arthritis, pyoderma gangrenosum, primary sclerosing cholangitis | Colonoscopy with biopsy of pathological lesions | Biopsy inflammation suggestive of IBD |
| Gastrointestinal advice | |||
| Coeliac disease | Malabsorption, chronic diarrhoea, failure to thrive in children, fatigue, mouth ulcers, anaemia, weight loss, dermatitis herpetiformis | tTG antibodies and IgA | Positive tTG antibodies test without IgA deficiency |
| Endoscopic duodenal or jenunal biopsies | Lymphocytic infiltration, villous atrophy | ||
| Post infectious | History of multiple pulmonary infections, tuberculosis or cough suppression | History or radiological evidence of previous infection | Radiological evidence of previous infection, history of cough suppression |
| Sputum with smear and culture for acid-fast bacilli | Positive for Mycobacterium aviumcomplex or other mycobacteria | ||
| Immunological disorders | Primary: recurrent infections, developmental delay in children, particular organ problems | IgG and subclasses, IgA, IgM | Decreased values, depending on age of patient. Adult: IgG<7.51 g/l; IgA<0.82 g/l; IgM<0.46 g/l |
| Full blood count | Lymphocyte or granulocyte deficit | ||
| Neutrophil antibody and function test, challenge with common humoral bacterial antigens | Result suggestive of antibody presence or impaired function | ||
| Secondary: lung transplant patients, patients under immunosuppressive therapy, HIV | IgG and subclasses, IgA, IgM | Decreased values, depending on age of patient | |
| HIV testing | Positive HIV serology | ||
| ABPA | Asthma, wheezing, coughing up brownish mucoid plugs or blood, upper lobe predominance | Total IgE, sputum sample | Raised total IgE>1000 ng/ml, presence in sputum |
| Specific serum IgE and IgG toAspergillus fumigatus | Raised Aspergillus IgE and/or IgG | ||
| Aspergillus fumigatus skin prick test | Positive skin prick test | ||
| Rheumatic disorders (RA, SLE, Sjögren, ankylosing spondylitis, relapsing polychondritis) | RA: rheumatoid nodule, arthritis, synovitis, specific skeletal deformities, rheumatoid nodule, other skin symptoms, etc | Autoimmune screening: rheumatoid factor, ANCAs, ANAs and anti-citrullinated peptide antibodies | Diagnosis depending on clinical examination combined with autoimmune screening results (positivity of rheumatoid factor, anti-citrullinated peptide antibodies, ANCAs, ANAs and/or ANA subtypes) |
| SLE: malar rash, ulcers, neuropsychiatric symptoms, etc | Rheumatological advice | ||
| COPD | Dyspnoea, Smoking history, Recurrent infections | Spirometry, bronchodilatation test | Obstructive lung function |
| Traction, obstruction, inhalation | Sarcoïdosis: fatigue, erythema nodosum, lupus pernio, arthralgia, uveitis, Bell’s palsy, etc | Chest CT scan | Hilar lymphadenopathy, reticulonodular infiltrates, pulmonary infiltrates, fibrocystic or bullous changes, non-caseating granulomas, upper lobe predominance |
| History of radiation therapy | Biopsy | ||
| History of inhalation/aspiration trauma | Bronchoscopy if imaging showing foreign body | ||
| YNS, Young’s syndrome, amyloidosis, endometriosis | YNS: yellow dystrophic nails, lymphoedema, sinusitis, pleural effusion | Exclusion diagnosis based on imaging and clinical findings | |
| Young’s syndrome: history of mercury contact, rhinosinusitis, infertility | Urological advice | ||
| Endometriosis: pelvic pain, infertility, cyclic haemoptysis/pain | Gynaecological evaluation | ||
| Idiopathic | Lower lobe predominance, combined chronic rhinitis/sinusitis | All of the above excluded | Exclusion diagnosis |
-
ABPA, allergic brochopulmonary aspergillosis; ANA, anti-nuclear antibodies; ANCA, anti-neutrophil cytoplasmic antibodies; CFTR, cystic fibrosis transmembrane conductance regulator; COPD, chronic obstructive pulmonary disease; IBD, inflammatory bowel disease; NPD, nasal potential difference; RA, rheumatoid arthritis; SLE, systemic lupus erythematosus; tTG antibodies, tissue transglutaminase antibodies; YNS, yellow nail syndrome.
BRONCHIECTASIS SEVERITY INDEX
Mnemonic: ABCDEFGH
- Age
- BMI
- Colonization status
- Dyspnea index (mmRC)
- Exacerbations in last 12 months
- FEV1% predicted
- Grading radiologically
- Hospital admissions in past 2 years
|
Severity criteria |
0 points |
1 point |
2 points |
3 points |
4 points |
5 points |
6 points |
|
Age |
<50 |
50-69 |
– |
70-79 |
– |
80+ |
|
|
BMI kg/m2 |
>18.5 |
<18.5 |
– |
– |
– |
– |
|
|
FEV1 % predicted |
>80% |
50-80% |
30-49% |
<30% |
– |
– |
– |
|
Hospital admissions in the past 2 years |
No |
Yes |
|||||
|
Exacerbation frequency in last 12 months |
0-2 |
3 or more |
|||||
|
MRC dyspnoea score |
1-3 |
4 |
5 |
||||
|
Colonisation status |
Not colonised |
Chronic colonisation |
P. aeruginosa colonisation |
||||
|
Radiological severity |
<3 lobes involved |
3 or more lobes or cystic changes |
Interpretation:
0-4: Mild bronchiectasis
- 1 year outcome: <2.8% mortality rate; <3.4% hospitalization rate
- 4 year outcome: <5.3% mortality rate; <9.2% hospitalization rate
5-8: Moderate bronchiectasis
- 1 year outcome: 0.8-4.8% mortality rate; 1-7.2% hospitalization rate
- 4 year outcome: 4-11.3% mortality rate; 9.9-19.4% hospitalization rate
9+: Severe bronchiectasis
- 1 year outcome: 7.6-10.5% mortality rate; 52.6% hospitalization rate
- 4 year outcome: 9.9-29.2% mortality rate; 41.2-80.4% hospitalization rate
COMMON DIFFERENTIAL DIAGNOSES OF BRONCHIECTASIS
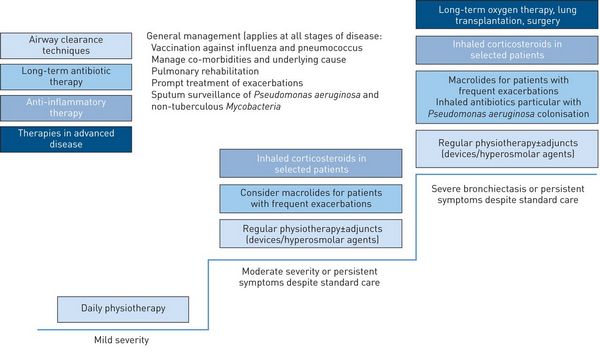
MANAGEMENT OF BRONCHIECTASIS
A) Treat underlying conditions
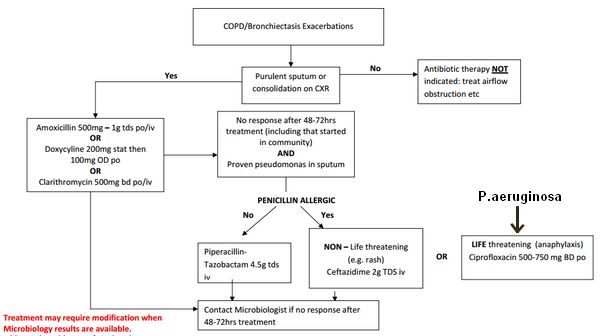
B) Recognize and treat acute exacerbation:
Recognize an acute exacerbation with 4 out of 9 criteria
- Change in sputum production
- Increased dyspnea
- Increased cough
- Fever
- Increased wheezing
- Malaise, fatigue, lethargy
- Reduced pulmonary function
- Radiographic changes
- Changes in chest sounds
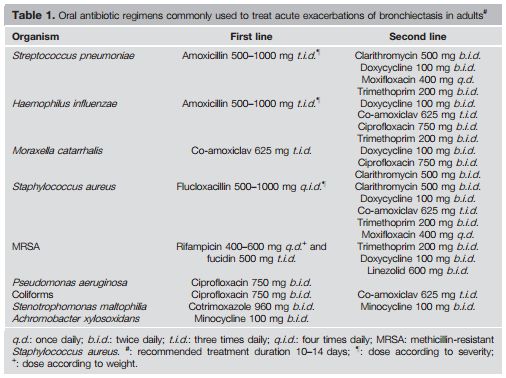
Antibiotic choice –
Source: http://www.dbh.nhs.uk/Library/Pharmacy_Medicines_Management/Formulary/Formulary_S5/COPD%20Flowchart.pdf
Source: Antibiotic treatment strategies in adults with bronchiectasis – C.S. Haworth
C) Maintenance treatment:
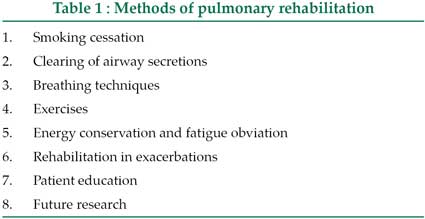
1. Pulmonary rehabilitation, improved nutrition and vaccination:
Get a brief idea on breathing techniques.
Airway clearance therapy: postural drainage, percussion, vibration, and the use of oscillatory devices for 15 to 30 minutes, 2 or 3 times daily.
Vaccination: Influenza vaccine and 23 valent pneumococcal vaccone
2. Inhaled bronchodilator:
- Appropriate for patients with co-morbid COPD or Asthma
- May improve tolerability of hyperosmolar agents
- Options:
- Salbutamol inhaled: 200 micrograms (2 puffs) every 4-6 hours when required; 2.5 mg nebulised every 6-8 hours when required
- Arformoterol inhaled: 15 micrograms nebulised every 12 hours when required
- Salbutamol/ipratropium inhaled: 200/40 micrograms (2 puffs) every 6 hours when required
- Ipratropium inhaled: 40 micrograms (2 puffs) every 6 hours when required
- Tiotropium inhaled: 18 micrograms (1 capsule) inhaled once daily when required
3. Inhaled hyperosmolar agent:
- Use bronchodilator prior to administration
- Shown to reduce inflammatory mediators, improve sputum bacteriology, and improve quality of life
- Options: hypertonic saline or mannitol
4. Long-term oral macrolide:
- Benefits: small improvement in FEV1, decreased sputum volume, and decreased exacerbation rate
- Action: Immunomodulatory
- Option: Azithromycin 250 mg orally once daily, or 500 mg orally three times weekly
- Disadvantages:
- Resistance development: Presence of mycobacteria in the sputum necessitates prompt discontinuation of macrolide monotherapy to minimise the risk of resistance developing.
- Cardiovascular risk: QTc prolongation
5. Inhaled antibiotic:
- Indication: high risk for chronic Pseudomonas infection (repeated exacerbations, recent history of antibiotic use, cystic fibrosis)
- Options:
- Tobramycin inhaled: 300 mg nebulised every 12 hours; give in cycles of 28 days on and then 28 days off
- Colistimethate sodium: dose depends on local formulation
- Gentamicin: 80 mg nebulised every 12 hours (no cycling)
- Disadvantages:
- Adverse events: some patients also suffered from cough, wheezing, and fatigue in response to the treatment
- Resistance development
6. Inhaled steroids:
Insufficient evidence exists to recommend use of inhaled steroids with stable bronchiectasis.
A therapeutic trial of inhaled steroids may be justified in adults with difficult-to-control symptoms.
Decrease sputum and tend to improve lung function
- Fluticasone propionate: 110–220 μg inhaled BID
-
Potential synergistic effect of long-acting β2-agonists with inhaled corticosteroids, allowing for lower steroid dose: Budesonide 160 μg/Formoterol 4.5 μg 2 puffs inhaled BID
7. Mucolytics:
- Avoid recombinant DNAse B in non-CF Bronchiectasis
- Options (use with antibiotics): Bromhexine 30 mg TDS, Erdosteine (mucolytic with antibacterial, antioxidant, anti-inflammatory properties)
Use of BRMs: In patients with recurrent episodes of pneumonia and bronchitis, BRMs be avoided until more trials have been carried out.
D) Surgery:
Indications:
- Recurrent infections
- Hemoptysis
- Focal disease
Options:
- Complete resection of bronchiectatic areas of lungs
- Lung transplantation
E) Supplemental oxygen and NIV:
- For severe ventilatory failure
Disclaimer: This is only for learning purpose and shouldn’t be used as a reference for the management.