We have already discussed about the practical essentials about Ascitic Paracentesis including absolute contraindications, site of needle entry and appropriate volume replacement. Laboratory analysis of ascitic fluid may provide answers to important clinical questions, as its composition varies depending on the underlying cause.
| Gross | Special test |
WBC (/mm³) |
PMN (/mm³) |
SAAG (g/dl) | Other testing | Provisional Diagnosis |
Further tests |
| Transparent or Crystal or Cloudy yellow (Neutrophils lead to shimmering effect when sample is glass tube is shaked back and forth in front of light) | PMN > 5000/ cu.mm is quite cloudy.PMN > 50,000/ cu.mm is like mayonnaise. |
<500 | <250 | ≥1.1 | Total protein <2.5 gm/dl | Uncomplicated cirrhotic ascites (WBC can rise to >1000/cu.mm but is lymphocyte predominant and PMN <250 /cu.mm in absence of signs and symptoms of infection occurs in diuresis related elevation) | Ultrasound &/or liver biopsy |
| Total protein ≥2.5 gm/dl | Cardiac ascites | Chest X-ray and ECG | |||||
| Bloody (>10,000 RBCs/cu.mm is pink; >20,000 is red; hetero-genous and clots immediately in traumatic tap; homo-genous and doesn’t clot because clot has already lysed in non-traumatic or remotely traumatic tap) | Subtract 1 WBC / 750 RBCs
Subtract 1 PMN / 250 RBCs |
<1.1 | Total protein <2.5 gm/dl | Nephrotic ascites | 24 hour urine protein | ||
| <500 or ≥500 | ≥250
(≥50% PMNs) |
≥1.1 | Single organism in culture, TP <1 gm/dl, Glucose >50 mg /dl, LDH <225 IU/L | SBP | Collect fluid for culture in blood culture bottles.
Gram stain is positive only when >10,000 bacteria/ml. Clinical response to antibiotic |
||
| ≥1.1 or <1.1 | Polymicrobial infection, TP >1 gm/dl, Glucose <50 mg/dl, LDH ≥225 IU/L | Secondary bacterial peritonitis | Look for perforation –
Upright chest xray (gas under diaphragm); Contrast studies of GI tract |
||||
| Milky | Triglyceride concentration >110 mg/dl is diagnostic of chylo-peritoneum; 100-200 mg/dl is like dilte skim milk; >200 mg/dl is like opaque milk | <1.1 | Ascitic fluid amylase >100 U/L | Pancreatic ascites | Abdominal CT | ||
| ≥250
(<50% PMNs) |
≥1.1 | Positive cytology | Peritoneal carcinomatosis & portal hypertension | Search for primary tumor Serum AFP is more sensitive than peritoneal fluid cytology in HCC (rarely sheds cells in ascitic fluid). |
|||
| Dark brown | Bilirubin concentration (> than serum in biliary perforation; < than serum in deeply jaundiced patients)
Tea-colored in pancreatitis (Effect of pancreatic enzymes on RBC) Black in pancreatic necrosis and melanoma. |
Fluid for TB testing | Tuberculous peritonitis and underlying cirrhosis | Myoco-bacterial growth on culture of laparoscopic biopsy specimen of peritoneum (100% sensitive)
Culture of 50 ml ascitic fluid (50% sensitive) ADA >30 U/L (93% sensitive and specific) IFN-γ >3.2 U/ml (93% sensitive and 96% specific) |
|||
| <1.1 | Positive cytology (nearly 100% sensitive) | Peritoneal carcinomatosis | Search for primary tumor | ||||
| Fluid for TB testing | Tubercular peritonitis | Myoco-bacterial growth on culture of laparoscopic biopsy specimen of peritoneum |
Serum Ascites Albumin Gradient (SAAG)
SAAG = Serum Albumin Concentration – Ascitic fluid Albumin Concentration
- ≥1.1 gm/dl suggests portal hypertension (pre-hepatic, hepatic or post-hepatic)
- <1.1 gm/dl suggests portal hypertension to be unlikely.
| HIGH GRADIENT≥1.1 g/dL (11 g/L) | LOW GRADIENT<1.1 g/dL (11 g/L) |
|---|---|
| Sinusoidal | Biliary ascites |
| Cirrhosis including SBP | Bowel obstruction or infarction |
| Acute Hepatitis or Hepatic failure | Nephrotic syndrome and hypoalbuminemic states |
| Extensive malignancy (HCC or metastases) | Pancreatic ascites |
| Post-sinusoidal | Peritoneal carcinomatosis |
| Right sided heart failure including constrictive pericarditis and Tricupsid regurgitation | Postoperative lymphatic leak |
| Budd-Chiari syndrome | Serositis in connective tissue diseases |
| Tuberculous peritonitis | |
| Sinusoidal obstruction syndrome | Meig’s syndrome (Ovarian fibroma) |
| Pre-sinusoidal: Portal or splenic vein thrombosis |
Mixed Ascites:
- Portal hypertension from cirrhosis with another cause of ascites like tubercular peritonitis or peritoneal carcinomatosis.
- SAAG ≥1.1 gm/dl in such cases.
Points to remember:
- If SAAG is definitive: determine SAAG only on the 1st paracentesis specimen and donot repeat in subsequent paracentesis.
- If SAAG is borderline (1 or 1.1 gm/dl): analysis in subsequent paracentesis usually provides definitive result.
- Both serum and ascitic fluid sample must be obtained nearly simultaneously (on the same day, preferably within same hour).
Falsely low SAAG:
- Serum albumin <1.1 gm/dl
- Arterial hypotension (may result in decrease in protal pressure)
- Hyperglobulinemia (contribute to oncotic force)
Correction of SAAG for hyperglobulinemia:
Corrected SAAG = Uncorrected SAAG X 0.16 X (serum globulin in gm/dl + 2.5)
Falsely high SAAG:
- Chylous ascites (lipid interferes with the albumin assay)
Choleperitoneum following Biliary perforation
- Ascitic fluid bilirubin >6 mg/dl
- Ascitic fluid bilirubin to Serum bilirubin ration >1
Bacterial Peritonitis
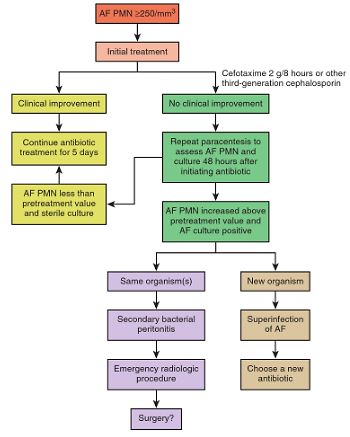
In patients with Ascitic fluid ANC ≥250/cu.mm it is necessary to differentiate between Spontaenous Bacterial Peritonitis (SBP) and Secondary Bacterial Peritonitis (due to bowel perforation or intra-abodminal source of infection). 2 out of 3 criteria of the following must be met for diagnosis of secondary bacterial peritonitis:
- Total protein
- Glucose
- LDH
| Ascitic fluid tests | Early Spontaneous bacterial peritonitis | Secondary bacterial peritonitis |
| ANC | ≥250/cu.mm | ≥250/cu.mm |
| Total protein | <1 gm/dl | >1 gm/dl |
| Glucose | >50 gm/dl | <50 gm/dl |
| LDH | < upper limit of normal (<225 U/L) | > upper limit of normal (>225 U/L) |
| Culture | Monomicrobial | Polymicrobial |
References:
- Sleisenger and Fordtran’s Gastrointestinal and Liver Disease
- Koss’ Diagnostic cytology and Its Histopathologic Bases
- GI/Liver Secret Plus by Peter R McNally