Synonyms: Ear drum, Myringa
Definition: Tympanic membrane is a thin membrane that separates the external ear from the middle ear.
Anatomy:
Site: Located at medial end of the external auditory canal, separating it from the middle ear cavity
Position: At an angle of 55° to the horizontal to the floor and directed downward, forward and laterally. It is horizontal in newborns but the reason behind this angulation in adults is because the anterior and inferior walls of the external canal grows longer than the posterior and superior walls. Adult position is reached by about 5 years of age.
Shape:
- Oval
- Concave laterally (towards external auditory canal) and slightly drawn inwards at its center – the umbo, where the handle of malleus is attached.
Size:
- Length: 9-10 mm
- Width: 8-9 mm
- Thickness: 0.1 mm
Structure:
- Outer epithelial/cutaneous layer: stratified squamous epithelium that normally reflects light
- Middle fibrous layer: thin/absent in pars flaccida; contains 3 types of fibers – radial, circular and parabolic; these fibers blend with the fibrocartilaginous tympanic ring at the circumference of tympanic membrane which anchors the tympanic membrane in the tympanic sulcus of the bony ear canal.
- Inner mucosal layer: single layer of squamous epithelium continuous with the lining of middle ear cavity and pharyngotympanic (eustachian) tube
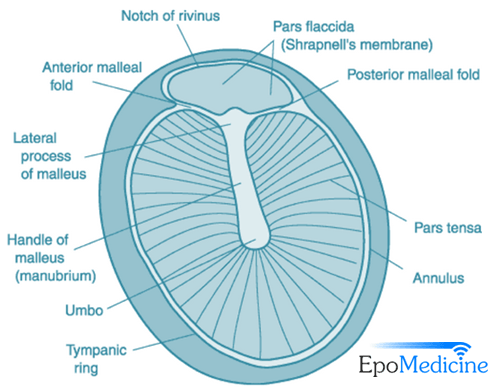
Components:
- Anterior and posterior malleolar fold: Converges to the lateral process of malleus from 2 ends of the tympanic notch of Rivinus
- Pars flacidda/Sharpnell membrane/Rivinus membrane: Part of relatively lax membrane lying above the malleolar folds; lack middle fibrous layer
- Pars tensa: Relatively taut and forms the remaining part of the tympanic membrane; contain all 3 layers
- Annulus tympanicus: Thick rolled periphery of pars tensa
- Umbo: Center of the tympanic membrane which divides it into 4 quadrants and the point of attachment for the handle of malleus
- Tympanic notch of Rivinus/Rivinus incisure: Notch (deficient area) in the superior part of fibrocartilaginous tympanic ring bridged by pars flaccida.
- Cone of light/Light reflex: In the antero-inferior quandrant, below and anterior to the handle of malleus
Color:
- Pars tensa: pearly white/grey
- Pars flaccida: pinkish
Blood supply: Branches from the External Carotid Artery (ECA)
Nerve supply (sensory only):
Medial/Inner surface: Jacobson’s branch of glossopharyngeal nerve (CN IX)
Lateral/Outer surface:
- Anterior 1/2 – Auriculotemporal nerve (CN V)
- Posterior 1/2 – Arnold’s branch of vagus nerve (CN X)
Mnemonic: TATA
1. Tympanic membrane
2. Auriculotemporal nerve (Anterior 1/2 – outer)
3. Tympanic branch of CN IX, i.e. Jacobson’s nerve (inner)
4. Auricular branch of CN X, i.e Arnold’s nerve (Posterior 1/2 – outer)
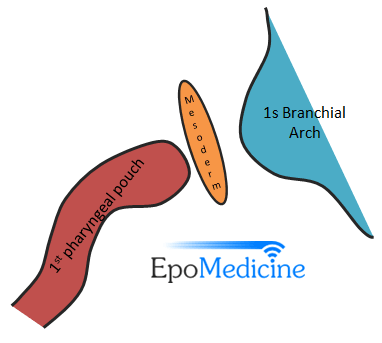
Embryology:
Middle ear begins to form by 3rd week and completes the development by 30th week. Tympanic membrane forms by the joining of expanding 1st pharyngeal pouch(endoderm lined) and groove (ectoderm lined) which is separated by a thin layer of splanchnic mesoderm. Hence, the 3 layers are derived from the 3 germinal layers.
- Outer epithelial layer: Ectoderm
- Middle fibrous layer: Mesoderm
- Inner mucosal layer: Endoderm
Functions:
- When the air-born sound vibrations reach the tympanic membrane, it vibrates and converts the air-born vibrations to mechanical vibrations.
- Gathers sound like a membrane of microphone
- Provides sonic shielding of the round window membrane
Applied anatomy:
- Umbo is in danger of perforation: Since, the arterial supply reaches from periphery towards the center, it has poor blood supply and in danger of perforation in inflammatory diseases of middle ear when arteries at periphery are thrombosed.
- Myringotomy incision: Myringotomy is an incision on the tympanic membrane under the direct vision to remove accumulated fluid or to provide aeration in case of malfunctioning eustachian tube. The incision is placed in postero-inferior quadrant to avoid injury to chorda tympani nerve and ear ossicles.
Clinical correlation:
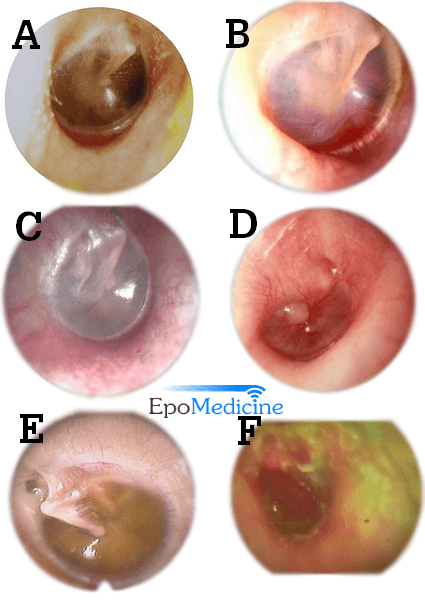
B. Rising sun appearance in Glomus jugulare
C. Bluish tympanic membrane in Secretory Otitis Media
D. Blebs of tympanic membrane in Bullous myringitis
E. Retracted tympanic membrane
F. Lighthouse sign in Acute suppurative Otitis Media
1. Retraction pockets: Due to lack of middle fibrous layer, pars flaccida often retracts first in response to negative pressure in the middle ear.
2. Myringitis granulosa: Affects only the outer epithelial layer; due to infection of external ear canal or constant irritation by wax
3. Myringitis bullosa: Blebs in the outer layer; due to viral infection, mycoplasma pneumoniae infection or middle ear effusion
4. Red tympanic membrane: Acute Otitis Media (AOM) or Glomus jugulare – this red reflex seen in glomus jugulare tumor is called “Rising sun” appearance
5. Blue tympanic membrane: Secretory otitis media, high jugular bulb
6. Schwartz sign: Pink reflex, seen through intact tympanic membrane, in the area of oval window. It indicates active otosclerosis usually during pregnancy.
7. Light house sign: Extruding discharge from the perforation of pars tensa in Acute suppurative otitis media

This was a very well explained article! Thank you!
This was a very helpful article. Thank you. Would you please add the surgical importance of layers of tympanic membrane?
Thank u so much. Really helpful