SYNONYMS: Cranial nerve seven (VII), Nervus facialis
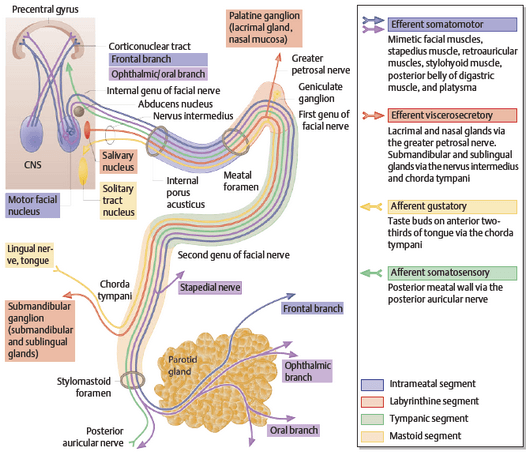
Supranuclear pathways
1. Somatomotor cortex: controlling motor component of facial nerve lies in precentral gyrus (Broadmann area 4,6,8)
2. Volitional component: Corticonuclear tracts descend and cross to supply both ipsilateral and contralateral facial (mainly to the contralateral side) nucleus i.e. frontal branch components of the facial nucleus receives bilateral cortico-nuclear tract innervation
3. Emotional component: Input to the facial nucleus from the basal ganglia and limbic system control involuntary facial expression associated with emotion.
4. Other inputs:
- From visual system (involved in blink reflex)
- From trigeminal nerve and nuclei (involved in corneal reflex)
- Auditory nuclei (involuntary closure of eye in response to loud noise)
Clinical correlation:
1. Wrinkling of forehead is a function of frontalis muscle and this is preserved in Upper motor neuron lesions (UMNL) of facial nerve. This is because, the frontal branch components of facial nucleus receives innervation from the cortex of both the sides.
2. Emotional (Involuntary) smile may be preserved in supranuclear palsy, while volitional (forced) smile is lost as the pathway for both are different.
3. Upper motor neuron lesion results in contralateral weakness while the lower motor neuron lesion results in ipsilateral weakness. Bell’s palsy and Ramsay hunt sydrome (Herpes zoster oticus) are the examples of lower motor neuron type of facial nerve palsy.
Intracranial part (15-17 mm)
Pons to Internal Acoustic Meatus
1. Nucleus:
- Motor nucleus (pons) – to motor fibers
- Superior salivatory nucleus (pons) – parasympathetic component to nerve of Wrisberg or Nervus intermedius
- Nucleus of solitary tractus (medulla) – receives sensory component from nerve of Wrisberg or Nervus intermedius
2. Before leaving brainstem: motor fibers wind around the abducens nucleus (CN VI) to form an internal genu
3. Leaves brainstem: at pontomedullary junction
4. After leaving brainstem: motor fibers align with nervus intermedius and together enters Internal acoustic meatus, along with vestibulo-cochlear nerve (CN VIII)
Clinical Correlation:
Facial nerve leave brainstem in close association with vestibulocochlear nerve at Cerebello-pontine angle (CP angle). Vestibular schwannoma and other tumors arising in the region of the cerebellopontine angle, may compress the facial nerve.
Intratemportal part
Internal acoustic meatus to Stylomastoid foramen
Mnemonic for segments: MLTM
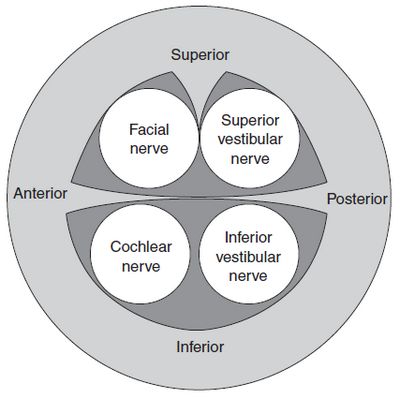
1. Meatal segment (8-10 mm): Within internal acoustic meatus – upto fundus
- Location: At the fundus or lateral end of the internal auditory canal (IAC), the transverse or falciform crest divides the IAC into superior and inferior portions. The superior portion is in turn further divided by the smaller and more laterally located vertical crest or “Bill’s bar.” The nerve lies in the anterior superior quadrant, above the falciform crest and anterior to Bill’s bar
2. Labyrinthine segment (4 mm): Fundus of Internal acoustic meatus to geniculate ganglion
- Fallopian canal: the nerve leaves internal acoustic meatus through the meatal foramen and enters fallopian canal or facial canal
- Geniculate ganglion: travels anteriorly untile geniculate ganglion is reached, and at this point –
- Completion of nerve: Intermedius nerve and motor nerve fibers join
- Greater Superficial Petrosal Nerve (GSPN): branchess off, which travels to pterygopalatine ganglion to innervate lacrimal, minor salivary glands and mucosal glands of nose and palate and receives taste from palate
- Skin of external acoustic meatus: few cells of the geniculate ganglion supply skin in and around the external acoustic meatus
- 1st genu: is formed as it turns sharply backward to continue as Tympanic segment
Note:
1. Vidian nerve (Nerve of pterygoid canal) = Greater superficial petrosal nerve + Deep petrosal nerve
Greater petrosal nerve carries parasympathetic fibers and Deep petrosal nerve carries sympathetic fibers (sympathetic plexus of Internal Carotid Artery). The Vidian nerve forms at the junction of these nerves on the base of the skull and enters the vidian (pterygoid) canal in the anterior wall of foramen lacerum. The nerve enters the pterygopalatine ganglion from its posterior surface and the sympathetic and parasympathetic information is distributed to all locations communicating with the ganglion.
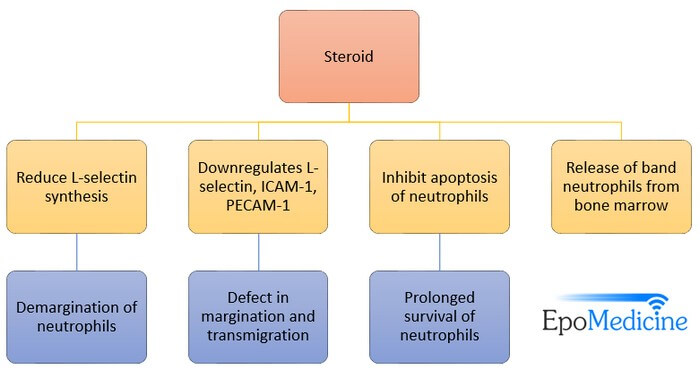
2. The facial or fallopian canal is narrowest (< 0.7 mm in diameter) in the labyrinthine segment and hence, most prone to palsy following edema of nerve caused by infection or inflammation.
3. Tympanic or Horizontal segment (11 mm): Geniculate ganglion to just above the pyramidal eminence
- Medial wall of middle ear: Runs horizontally on medial wall of medial ear cavity within fallopian canal
- Relations: lies above oval window and below lateral semicircular canal
Note: Tympanic segment is the commonest site of dehiscence of facial canal – both acquired (cholesteatoma) and natural, which makes it susceptible to injury.
4. Mastoid or Vertical segment (13 mm): Pyramid to stylomastoid foramen
- 2nd genu: Turns vertically downwards at ~ 90° at the level of pyramid forming 2nd genu
- Nerve to stapedius branches off, at 2nd genu
- Sensory nerve to skin of External Auditory Canal branches off
- Chorda tympani (terminal branch of the nervus intermedius carrying both secretomotor fibres to the submandibular gland and sublingual gland and taste to the anterior two thirds of the tongue) branches off near, the stylomastoid foramen
- Mastoid: Courses within fallopian canal in mastoid bone until stylomastoid foramen is reached
Note: Facial recess is a triangular space bounded by fossa incudis, facial nerve and chorda tympani (which branches from facial nerve making approximately 30°). This is an important surgical route for entry into middle ear, especially in combined approach tympanoplasty.
Extracranial part
1. Exits: the skull base through the stylomastoid foramen, between the mastoid tip laterally and the styloid process medially. The surgical landmarks necessary to identify facial nerve during parotid surgery has already been discussed earlier.
2. Branches in neck:
- Posterior auricular branch: to auricular muscles and occipitalis muscle
- Digastric branch: to posterior belly of digastric muscle
- Stylohyoid branch: to stylohyoid muscle
3. Passes into the parotid gland: where it branches at Pes anserinus, into temporofacial and cervicofacial division
Mnemonic to remember peripheral branches:
Mnemonic in English: Two Zombies Buggered My Cat
If you understand Hindi language: Tum Zyada Bakbak Mat Caro
- The upper temporofacial division gives: Temporal and Zygomatic branches
- Temporal branch: Muscles of auricle, Frontalis(voluntary raising of eyebrows), Corrugator, Procerus
- Zygomatic branch: Orbicularis oculi (proper eye closure), Zygomatic major
- Lower cervicofacial division gives: Buccal, Marginal mandibular and Cervical branches
- Buccal branch: Buccinator and orbicularis oris (proper mouth closure and muscle cheek activity), Nasalis, Levator labii superioris, aleque nasi, zygomatic major and minor, levator angularis oris
- Marginal mandibular branch: Depressor angularis oris, Orbicularis oris, Mentalis, Depressor labii inferioris, risorius
- Cervical branch: Platysma (move lower lip and jaw downwards and to the side)
Clinical correlation:
1. Motor function of facial nerve is tasted for these peripheral branches by asking the patient to wrinkle forehead, open closed eyelids against resistance, whistle and clench the teeth. How to examine facial nerve?
2. Injury to the parotid or any parotid mass or swelling can lead to the injury of facial nerve.
3. Sensory innervation to the skin of face is through the trigeminal nerve (CN V), hence general sensation from face remains intact in facial nerve palsy.
Note:
1. Facial nerve supplies the muscles of facial expression which are derived from the 2nd branchial arch.
2. The word “pes anserinus” refers to “goose feet-like”. Pes anserinus is also named for the common insertion of sartorius, gracilis and semitendinosus into the proximal tibia, medial to tibial tuberosity.
Summary
1. Course: Pontomedullary junction → Posterior cranial fossa → Internal acoustic meatus → Fundus of Internal acoustic meatus → Bony facial canal → Stylomastoid foramen
2. Facial Nerve Subdivision and Functions:
- Branchial motor: Muscles of facial expression, Posterior belly of digastric muscle, Stylohyoid muscle, Stapedius muscle
- Visceral motor: Salivation (lacrimal, submandibular, and sublingual), Nasal mucosa or mucous membrane
- General sensory: Sensory to auricular concha, External auditory canal, Tympanic membrane
- Special sensory Chorda tympani nerve (taste to anterior 2/3 of the tongue)
3. Donor nerve: The most common donor nerve for facial nerve grafting is Greater auricular nerve.
Thanks. That is great.
It is very interesting thanks so much.