Inflammation of the Appendix is one of the most common causes of Pain Abdomen presenting in the Emergency Room. Since its first description in the texts, there has been a lot of improvement in the quality of management due to the availability of resources and technology.
Appendix, in the initial days has not been described in the texts and not understood as the all the studies about anatomy was done on the primates (monkeys), until 1521 Berengario DaCarpi, an Italian Anatomist where he described it as a small cavity at the end of Cecum.
The identification of the appendix led to the reporting of gangrenous appendix in the autopsy of patients. In 1839, acute appendicitis was described with its symptomatology and appendix was considered as the one of the main causes for inflammatory process of the Right Lower Quadrant. The first known documented diagnosis of gangrenous appendicitis followed by removal of the appendix was done by Robert Lawson Tait in 1880. Later on it was known that, the first surgery for the removal of appendix was done in 1735 by Claudius Amyand. In 1886, Reginald H. Fitz published a paper describing the clinical features of inflammation of appendix and for the first time the word “Appendicitis” was coined, he also stressed on the surgical management and named it as “Appendectomy”.
Later in 1894 Charles H McBurney had proposed early laparotomy as the main mode of management and a procedure to follow Open Appendectomy which is being followed today with few modifications. The advent of Laparoscopy has also impacted on the procedure of Appendectomy, which have also proven to be advantageous.
Anatomy & Physiology
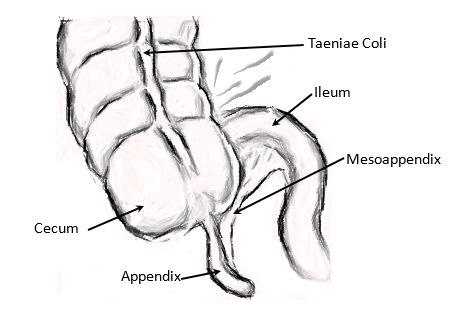
Appendix is a small tubular organ, part of the midgut, present at the junction of small and the large intestine.
Development
- Starts appearing at 8 weeks of gestational age as an outpouching from the cecal diverticulum. It grows and becomes elongated and tubular.
- As a result of differential growth of the walls of cecum, the appendix comes to lie in the postero-medial position and intraperitoneally. As the gut rotates, the appendix finally lies in the Right Lower Quadrant.
Abnormal position of the Appendix is seen in cases of:
Mal-rotation: Left Upper Quadrant
Situs Inversus: Left Lower Quadrant
Structure
- Size of the appendix varies from 5cm – 35cm (avg. 9cm), with a diameter of 3mm – 8mm.
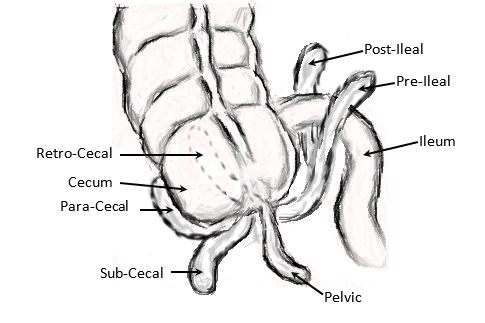
- Its base can be identified as the confluence of the 3 Taeniae Coli, whereas the position of the tip is variable most common being in the retrocecal position.
- Others are Paracecal, Subcecal, Pelvic, Postileal, Preileal and Retroperitoneal.
- The mesenteric attachment is derived from the ileal end of the mesentery known as Mesoappendix, which contains the Artery, Vein, Lymphatics, Sympathetic and Parasympathetic nerves.
The positions should be kept in mind during the examination of the patient as location of pain and tenderness changes accordingly.
Histology
- It is composed of the basic 4 layers of the GIT: Mucosa, Sub-Mucosa, Muscular and Serosa.
- Mucosa is arranged in the form of crypts with columnar type of epithelium, neuroendocrine cells and mucin producing cells. Lymphoid tissue is found in the Sub-Mucosa.
- Appendicular Artery – branch of Iliocolic Artery from the Superior Mesenteric Artery.
- Appendicular Vein – drains into Superior Mesenteric Vein via Iliocolic Vein.
- Lymphatics to Iliocecal Lymph Nodes finally Superior Mesenteric Nodes.
- Innervated by Sympathetic and Parasympathetic nerves from Superior Mesenteric Plexus.
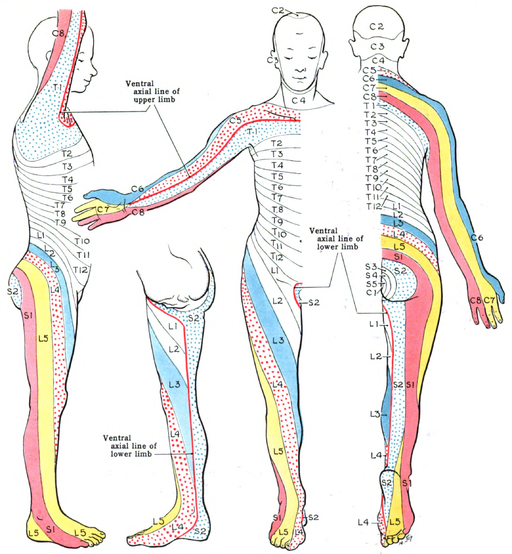
- Afferents enter the spinal cord at T10.
Physiology
- It has an Immunological Function of secreting Ig A and known to be a reservoir for colonic bacteria.
Appendicitis
Previously known as Peritiphilitis, renamed in 1800’s has been rising in incidence in the recent times owing to the advancement in the diagnostic and imaging technology.
Age
- Relatively uncommon in infants, rates increasing as age progresses till mid 20’s and gradually reducing.
Etiology
- Luminal Obstruction seems to be the important factor for the development of Appendicitis.
Obstruction may be caused due to:
Fecalith
Lymphoid Hyperplasia
Food debris
Stricture (due to past subsided inflammation)
Tumor
Pinworm (Enterobius)
Organisms found
- Gram Negative and Anaerobic Bacteria.
Pathology
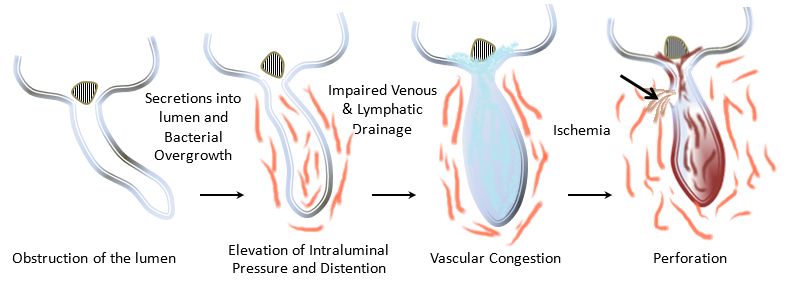
- The proposed theory for development of appendicitis is due to Luminal Obstruction.
- Distension of the appendix stimulates the nerves which causes the vague visceral pain, nausea and vomiting. Colonization of the Bacteria which enters the mucosa causes the inflammatory reaction and soon spreads to the serosa and peritoneum. This spread causes the shift of the character and location of the pain.
- Further distention causes impairment of blood supply causes ischemia and becomes gangrenous, and the area of poorest blood supply (ante mesenteric area) is subjected to perforation, this relieves the patient with all the symptoms temporarily but develops symptoms of diffuse peritonitis within few hours. If left untreated may develop into Appendicular Mass or Abscess.
Clinical Presentation
- The patient mainly complaints of a vague abdominal pain (commonly periumbililcal) which is later localized to the Right Lower Quadrant, colicky type and aggravating on movements.
- Pain is associated with Nausea, Vomiting and Anorexia.
Signs
- The patient is found to look ill, lie still, have pyrexia and tachycardia.
- Palpation of the abdomen reveals tenderness at the McBurney’s Point with guarding and rigidity.
- Few classical signs indicating the presence of appendicitis with peritoneal irritation are: Pointing Sign, Blumberg’s Sign/Rebound Tenderness, Rovsing’s Sign, Obturator Sign and Psoas Sign. Better examined in Left Lateral Position.
- Per Rectal Examination, reveals tenderness towards right side in case of a Pelvic appendix.
- In women Per-Vaginal examination should not be omitted to rule out cervical motion tenderness which indicates Pelvic Inflammatory Disease.
- Auscultation feature a ‘Silent Abdomen’ if diffuse peritonitis has set up, else would show silence localized to the area of peritonitis.
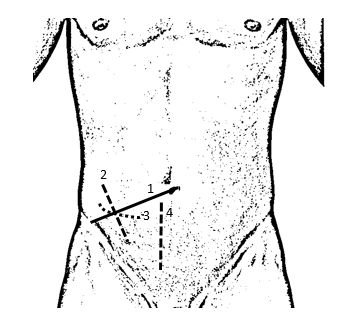
McBurney’s Point: A point at 1/3rd the distance between Anterior Superior Iliac Spine and Umbilicus.
Sherren’s Triangle: Between Anterior Superior Iliac Spine, Umbilicus and Pubic Symphysis. This is the area of Hyperesthesia seen in Gangrenous Appendicitis.
Kocher’s Sign: Shift of pain from the Umbilical Region to the Right Lower Abdomen from the history.
Pointing Sign: Coincidence of the point where patient points towards the site of pain and where maximum point of tenderness is.
Dunphy’s Sign: Aggravating pain in Right Lower Quadrant while cough.
Murphy’s Triad: Sequence of Pain in the Rt. Lower Quadrant followed by Vomiting and then increase in Temperature.
Blumberg’s Sign: Sudden pain on quickly removing pressure over the point of tenderness.
Rovsing’s Sign: Presence of pain in the right iliac fossa on palpation of the left iliac fossa.
Obturator Sign: Presence of pain on Internal Rotation of Right Hip. (Inflammed appendix lies on the Obturator Internus) – Pelvic Appendix.
Psoas Sign: Presence of pain on Extension of the Right Hip. (Inflamed appendix lies on Psoas Major) – Retrocecal Appendix.
Bapad Test: Aggravating pain on lifting the foot end of the bed i.e., movements.
Heal Tap Sign: Presence of pain on hitting the partially elevated Right Heel.
Differential Diagnosis
| General | Children | Women |
|---|---|---|
|
|
|
Lab
- Leukocytosis, Shift to Left (prominence of Immature Neutrophils-Band Forms).
- Urinalysis shows leukocyte esterase due to the proximity of the appendix and urinary bladder/ureter. In women, Urine Pregnancy Test also to be advised.
- CRP is found to be elevated.
Imaging
- Plain Radiograph – To rule out perforation, pneumonia, renal calculi, fecalith.
- Ultrasonogram – Enlarged, Immobile, Non-compressible, Thick and Inflamed wall, Periappediceal fluid appears as a TARGET.
- CT – Enlarged, Thick and Inflamed Wall, Free Fluid, Inflamed mesoappendix, Fecalith.
Scoring (Alvorado Score)
- Used in determining the likeliness of Appendicitis based on the Symptoms, Signs and Lab Data.
Variations in the Symptoms
- Retrocecal Appendix – The classical feature of the pain, rigidity and tenderness in the Right Lower Quadrant is unlikely, but tenderness may be present in the right flank. As it is present close to ureter, there may be complaints of hematuria, pyuria and pain radiating from the loin to groin.
- Pelvic Appendix – Pain and tenderness is not prominent, but a various other symptoms such as strangury/increased frequency, diarrhea and passage of blood with mucus from the rectum.
- Post-Ileal Appendix – Pain initially starts around the umbilicus, but there is no shift in the pain. Tenderness and rebound tenderness also is poorly elicited. There are complaints of diarrhea.
Management
Based on the situation at the time of presentation, appendicitis can be classified into types:
- Acute Uncomplicated: Inflammation of the mucosa of the appendix which presents with mild symptoms. This can lead to resolution, fibrosis or recurrent appendicitis.
- Acute Complicated: Complete obstruction of the appendix which in due course of time may become oedematous, gangrenous and lead to perforation with abscess/phlegmon.
Appendectomy
- Once the diagnosis is established according to the scoring systems and imaging, the decision is to be made when to perform the surgery which depends on the condition of the appendix seen on imaging.
- Pre-Operative Management:
- Proper counseling and explanation to be given about the situation, procedure to be executed, complications which may arise pre/intra/post operatively.
- Complete Surgical and Anesthetic fitness to be obtained.
- Patient should be Nil per Oral from the night before (in Emergency, Ryle’s tube to be placed and contents should be emptied).
- Surgical area to be cleaned with antibacterial agent and hair to be clipped. (Surgical Area – From Infra-mammary region to the upper half of the thigh.
- Antimicrobial Agents – Inj. Metronidazole 500mg (against Anaerobic Bacteria) and Inj. Ceftriaxone 1gm / Cefuroxime 1.5gm. (against Gram Negative Bacteria)
- Analgesics – Inj. Voveran i.e., Diclofenac Sodium 75mg (acts as an antipyretic too), Inj. Buscopan i.e., Hyoscine 10mg (smooth muscle relaxant & antiemetic).
- Antiemetics – Inj. Ondansetron 4mg (antiemetic).
- Pre-Operative Medications – Inj. Ranitidine 150mg / Inj. Pantoprazole 40mg (raise pH), Inj. Metoclopramide 10mg (reduce gastric secretions and increase the tone of LES), Inj. Tetanus Toxoid 0.5ml, Tab. Diazepam (reduces anxiety).
- Empty the bladder and rectum.
- Secure an Intravenous cannula and a Foley’s Caterer.
- Administration of Intravenous fluids, mainly crystalloids.
- Pre-Operative Management:
- In the Operation Theater:
- After the identification of the patient, confirmation of the type of surgery, complete general examination, the patient is hand over to the Anesthetist to administer the Spinal Anesthesia.
- The patient is then placed in the Operation Table in Supine position, the Surgical Area is painted and scrubbed with Bactericidal solution and the patient is draped with the sterile sheets keeping the surgical area open.
- The plane of anesthesia is verified, now the patient is ready for the procedure.
- INCISION: Widely incision used is the gridiron incision; others are Rutherford-Morison, Lanz and Right Lower Paramedian Incisions.
Gridiron Incision – Conventionally used for uncomplicated appendicitis.
Rutherford-Morison Incision – Used in case of paracecal and retrocecal appendix.
Lanz Incision – Cosmetically better, used in obese and is easy to extend the incision for better visualization.
Rt. Lower Paramedian Incision – In case of development of perforation and diffuse peritonitis.
Incisions
- Right Spinoumbilical Line.
- Gridiron Incision – An incision perpendicular to right spinoumbilical line at the McBurney’s Point.
- Lanz Incision – Horizontal Incision at the McBurney’s Point. It can also be described as an incision 2cm below the umbilicus centered at the right midclavicular-midinguinal line.
- Right Lower Paramedian Incision
- Incision is deepened keeping a bloodless field, as the muscle layer is reached they are split parallel to the fibers. First the external oblique is split extending from the rectus muscle to the iliac crest, followed by the internal oblique with the transversalis muscle. A modification of this process is the Rutherford-Morison procedure where the muscle is incised and cut at the McBurney’s point and extending laterally in the direction of the skin incision.
- The peritoneum is now incised, keeping in mind no internal structured is damaged.
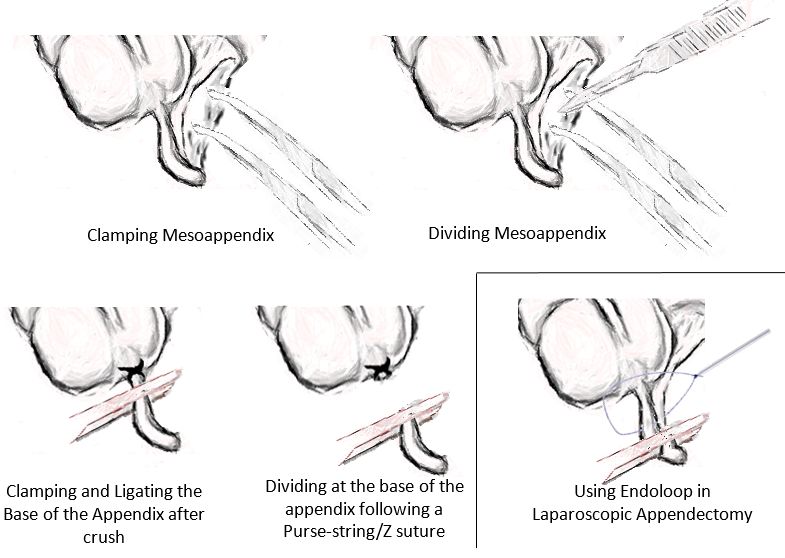
- Cecum is visualized, with the anterior taenia coli appendix is traced, both cecum and appendix are mobilized from their attachments and delivered out of the wound.
- The base of the mesoappendix is identified and clamped, divided and ligated.
- The base of the appendix is crushed using an artery forceps, and ligated close to the cecum. It is divided between the part ligated and the part crushed.
- The stump of the appendix is cauterized or buried using a purse-string or Z suture.
- The abdomen is thoroughly irrigated and drained.
- A part of the omentum is placed over the stump and cecum.
- Peritoneum and the transversalis fascia are sutured together, followed by internal oblique and then the external oblique. Abdominal wall is sutured in layers after hemostasis is confirmed.
- The abdomen is wiped off of any blood stains and the wound is cleaned with bactericidal solution and an Antiseptic Bandage is applied.
- Laparoscopic Appendectomy is started by creating 3 ports (umbilical, left lower quadrant and supraumbilical). Pneumoperitoneum is created, a similar procedure to open is followed except that during ligation, an Endoloop is used. The appendix is delivered and abdomen is inspected for any adhesions or infectious material and closed.
- Few other types of surgeries executed for appendicitis are – Single Incision Laparoscopic Appendectomy, Natural Orifice Appendectomy and Incidental Appendectomy.
In other situations –
Perforation: Handling of the gangrenous appendix should be gentle owing to its friable nature, after removing the appendix thorough, large volume irrigation and drainage has to be done to remove any infectious material from the abdomen.
Appendicular Abscess: The abscess is localized by the assistance of ultrasonogram, and is drained percutaneous, if found during the surgery, it should be removed followed by a thorough wash and placement of drains. An interval appendectomy is planned after 3 months.
Appendicular Mass: A complication of Acute Appendicitis following perforation, leads to the formation of an appendicular mass consisting of the inflamed appendix, part of the cecum with ileum, greater omentum and parietal peritoneum in the Right Iliac fossa. Ochsner-Sherren regimen is followed which states a conservative therapy (IV antimicrobials, IV fluids, Analgesics and Antipyretics) followed by an Interval Appendectomy after 6 – 12 weeks.
Retrocecal/Adherent Appendix: End of the Cecum is identified with the anterior taenia coli which is traced to the base of the appendix, it is separated from the cecum, vessels are identified and ligated, base is ligated and the stump is buried and the appendix is separated from the base to the tip. This procedure is known as Retrograde Appendectomy.
Mucocele of Appendix: Results due to chronic obstruction to the appendix leading to collection of sterile mucin, care to be taken not to puncture the cyst, any of the contents is retained in abdomen may lead to Pseudomyxoma peritonei.
- In the Post-Operative Ward:
- As the patent is shifted to the Post-Operative Room and needs to be taken care of the anesthetic dose as advised by the anesthetist.
- Fluid Balance has to be maintained by administering IV Ringer Lactate.
- IV Antimicrobials are to be continued till Day 3, and then switched to Oral (only if complicated).
- Antipyretics and Analgesics are administered as required.
- A regular check has to be done about the pulse rate, temperature, blood pressure, bowel movements, urine output and the condition of the wound. The wound bandage has to be changed every day.
- Sutures can be removed on day 7, based on the healing status.
- Patient is advised to sit by the end of the day and start walking on Day 1.
- Patient has to be Nil per Oral post 6 hours of surgery and should be allowed sips of water followed by liquid diet, soft diet and then normal food based on the response of the bowel movements.
- Patient can be discharged according to the recovery.
Complications
- Primary or Secondary Hemorrhage
- Surgical Site Infection
- Pelvic Abscess
- Paralytic Ileus
- Stump Appendicitis
- Fecal Fistula
- Adhesions, Intestinal Obstruction
- Right Direct Inguinal Hernia, injury to the Ilioinguinal nerve
- Incisional Hernia
- Other Post-Operative Complications such as Deep Vein Thrombosis, Respiratory Failure (GA), Venous Thromboembolism.
Summary
Appendix is a blind ended organ present at the junction of the small and large intestine. Derives its blood supply from Iliocolic artery.
Appendicitis is the inflammation of the appendix causing pain in the umbilical region followed by localization to right lower quadrant, nausea, vomiting and anorexia. On examination tenderness is found at the McBurney’s point with rebound tenderness as a classical signs.
Plan of management depends on Alvorado Scoring system which is based on symptoms, signs and lab values.
Emergency surgical management plays an important role, unless the score is not adequate or in case of appendicular mass or abscess.
Various techniques may be followed for the surgery such as: Open, Laparoscopy, Single Incision Laparoscopy and Natural Orifice Appendectomy.
Reference
- A History of Appendicitis – https://www.oumedicine.com/docs/ad-surgery-workfiles/williams_history-of-appendicitis-with-anecdotes-illustrating-its-importance.pdf
- The early days in the history of appendectomy-https: //hekint.org/2017/01/22/the-early-days-in-the-history-of-appendectomy/
- Bailey & Love, 27th Edition – The Vermiform Appendix.
- Schwartz’s Principles of Surgery, 10th Edition – The Appendix.
- Sabiston Textbook of Surgery, 20th Edition – The Appendix.
- Zollinger’s Atlas of Surgical Operations, 10th Edition – Appendectomy.

Graduated from one of the famous institutions in Telangana, Kamineni Institute of Medical Sciences. He has always been fond of writing articles in Medicine. Since the undergraduate years was interested in making creative Presentations and taking seminars.

There were few other signs we learnt back in medical school.
Ten Horn sign: Traction in the right spermatic cord in male causes pain in right iliac fossa in acute appendicitis.
Aaron sign: Continuous firm pressure over the McBurney’s point causes pain in the epigastrium, left hypochondrium, umbilical and precordial regions in chronic appendicitis.
Thank you Dr. Rob for the additions.:)